To evaluate the relationship between asthma control, family income and family costs of asthma in a population of children-adolescents; to detail the family costs of asthma in this age range; and to compare asthma costs for the families of children-adolescents and adults.
MethodsThe authors invited asthmatic subjects who attended a scheduled spirometry test at the Jundiaí School of Medicine (FMJ). The FMJ performs all spirometry tests requested by staff physicians who serve at the public healthcare system in the municipality. Volunteers responded to the ACQ, the Asthma Family Costs Questionnaire and underwent a spirometry test.
ResultsThe authors included 342 children-adolescents. Families of children-adolescents taking maintenance therapy and families of those reporting uncontrolled asthma symptoms were more likely to report any expenditure with asthma during the preceding month. In this age range, the smallest expenditures were on diagnostic tests and medical consultations, while home expenditures to avoid asthma triggers were the highest ones. As compared to adults’ families, the children and adolescents families reported a greater proportion of income committed with asthma. Expenditures with transportation to healthcare facilities for asthma care were greater in the families of children-adolescents as compared to the values reported by the adults’ families; in contrast, loss of income due to asthma was smaller in the families of children-adolescents.
ConclusionsChildren-adolescents’ asthma affects the household economy. The authors believe researchers should assess this outcome when designing studies about asthma. Finally, the study's data support the necessity of public policies in low-resource communities to minimize the economic impact of children and adolescents’ asthma.
The increasing access to inhaled corticosteroids has been contributing to the declining rate of health resource use by children and adolescents with asthma, but asthma is still a major public health problem.1 In the United States, asthmatic children incurred a higher rate of all-cause annual emergency department visits, hospitalizations, outpatient visits, and prescription drugs compared with school-aged children without asthma.2 In Brazil, a large countrywide study observed more than 29,000 yearly hospital admissions due to asthma in children from 5 to 14 years of age,1 and another study identified 5,014 asthma deaths from 1997 to 2014 in the population up to 19 years old.3 Most hospital admissions and deaths occur in subjects with moderate-severe asthma, but it is meaningful that mild asthmatic children and adolescents not taking maintenance therapy may experience life-threatening exacerbations as well.4-6
From the economic perspective, direct and indirect financial costs of pediatric asthma are high, exceeding 5 billion dollars per year in the United States.7In Portugal, 0.9% of the overall healthcare expenditures are directed to the care of children and adolescents’ asthma.8 Some countries spend more than 50% of the financial resources destined for asthma care on purchasing medicines,9,10 but spending money on asthma maintenance therapy is cost-effective. Countrywide studies showed that subsidizing inhaled medications for asthma, and other obstructive pulmonary diseases have contributed to reducing the rate of emergency room visits and hospital admissions, thus reducing the overall costs of these illnesses.1,11
There is extensive literature measuring the economic burden of asthma for the government and healthcare providers, but few studies investigated the effect of asthma on the household economy. Among adults, one cohort study demonstrated that initiating maintenance therapy for severe asthmatic subjects who were on no previous health care was associated with a 90% reduction in the family costs of asthma and a 20% increase in family income.12 The authors are not aware, however, of studies measuring the financial consequences of childhood and adolescence asthma on the family budget. Clarifying this issue is important because it has direct consequences for the asthmatic subjects and their families, especially those underprivileged, and it would provide us with new information to build an effective social support network for this population. Therefore, the aims of this study were to evaluate the relationship between asthma control, family income, and family costs of asthma in a population of children and adolescents; and to detail the family costs of asthma in this age range. The authors were also interested in comparing the family costs of asthma between children-adolescents and adults, as it would provide us reference parameters on this issue.
Material and methodsStudy populationThe authors conducted this study in Jundiaí, a 400,000-inhabitant city in Brazil. The authors invited every asthmatic subject who attended a scheduled spirometry test at the Jundiaí School of Medicine (FMJ) from August 2018 to July 2020. The FMJ performs all spirometry tests requested by the staff physicians who serve at the public healthcare system of the municipality. Thus, the present study population is a representative sample of all asthmatic subjects receiving health care at public facilities in Jundiaí city.
Inclusion criteria were asthma diagnosis, age above nine years old, and had outpatient care for asthma during the six months before the study admission. Exclusion criteria were pregnancy and other concomitant lung diseases, such as lung scars due to pulmonary infections, bronchiectasis, or congenital lung malformations. The Institutional Review Board of the Jundiaí School of Medicine approved the study (approval number 2.198.023). All subjects and caregivers signed informed consent. Subjects aged below 18 years signed the assent term.
Criteria for asthma diagnosis were recurrent respiratory symptoms lasting longer than one year and symptoms improvement after inhaled corticosteroids or relief after bronchodilator. Another criterion of asthma diagnosis was FEV1 improvement above 200 ml and 12% after bronchodilator in any spirometry test performed during the preceding year or between two spirometry tests.
Study proceduresAll eligible subjects who agreed to participate underwent a cross-sectional evaluation. They responded to the Asthma Control Questionnaire (ACQ), the Asthma Family Costs Questionnaire (AFCQ)12 and underwent a spirometry test with a Koko-PDS® spirometer. The spirometry tests were performed by a trained physiotherapist under the direct supervision of a chest physician.
Family income and family costs of asthmaThe authors applied the AFCQ to estimate the family income and family costs of asthma during the preceding thirty days. Early economic data were not accounted for due to the risk of memory bias. The AFCQ questionnaire estimates the direct costs of asthma paid with personal funds, which include expenses with transportation, diagnostic tests, doctor consultations, medicine purchase, hospital expenses, acquisition of medical devices such as air humidifiers or nebulizers, household reforms to avoid environmental triggers, and other direct expenses reported by the subject. It also estimates indirect costs such as loss of working days due to asthma, loss of time waiting at or moving to health facilities for asthma care, and other indirect costs reported by the subject. Family income encompassed regular and eventual incomes, pension and retirement benefits, governmental and non-governmental help, donations, or any other income during the preceding thirty days. Financial values were inflated to June 2021 and converted to USD. The authors applied the Brazilian inflation index published at https://www.ibge.gov.br/explica/inflacao.php.
Statistical analysesThe primary aim of this study was to evaluate the relationship between asthma control, family income, and family costs of asthma in a population of children and adolescents. Markers of asthma control were uncontrolled asthma symptoms according to the ACQ questionnaire score ≥ 1.5 and airway obstruction in the spirometry test. The criterion of airway obstruction was the FEV1/FVC ratio below the lower limit of normality in the spirometry test performed at the study visit.13 The authors also evaluated the relationship between maintenance therapy need and the study outcomes (family income and family costs of asthma), because maintenance therapy need is a marker of persistent asthma. The authors calculated a sample of 72 subjects in each study group considering the median asthma costs of 5 USD in the group reporting controlled asthma symptoms (ACQ < 1.5) and 10 USD in the group reporting uncontrolled asthma symptoms (ACQ ≥ 1.5), a standard deviation of ±10, 95% confidence interval, and 80% power.
Continuous and ordinal variables were depicted in median and interquartile, while nominal variables were depicted in absolute numbers and proportions. The authors used the Mann-Whitney and Chi-Square tests for comparisons between two groups and the Kruskal-Wallis test for comparisons between more than two groups. The authors also performed binary logistic regression analyses to evaluate if markers of uncontrolled asthma (independent variable) would predict any asthma expenditure during the preceding thirty days (dependent variable). The authors adjusted the regressions for the per capita family income because it would interfere in the relationship between the dependent and independent variables.14 The method of data entry into the regression models was the Backward Likelihood Ratio. The authors used the Hosmer-Lemeshow test to measure goodness-of-fit, and the tolerance test and variance inflation factor in measuring collinearity. Data fitted with the model, and the authors observed no collinearity (SPSS 25.0; SPSS Inc., Chicago, IL, USA).
ResultsThe authors included 1,072 subjects in the study, 342 children and adolescents, and 730 adults. Children and adolescents reported fewer comorbidities, fewer asthma symptoms, less use of inhaled maintenance therapy, and got better spirometry test values as compared to adult subjects (Supplementary Table 1). In contrast, their legal guardians reported similar family costs of asthma [USD; 58 (10-156) & 49 (0-142), p 0,15] and greater proportion of family income committed with asthma expenditures [1.4 (0.2-5.6) & 1.1 (0.0-3.7), p 0,01] as compared to adults (Supplementary Table 1).
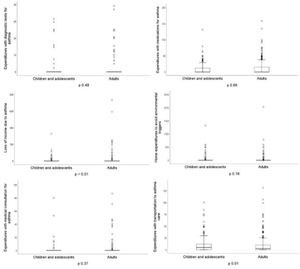
Fig. 1 shows a detailed comparison of the family costs of asthma between children-adolescents and adults. Loss of income due to asthma was greater in the families of adult asthmatic subjects, while expenditures with transportation to healthcare facilities for asthma care were greater in families of children and adolescents with asthma. Expenditures with medications, medical consultations, diagnostic tests, and home expenditures to avoid triggers of asthma were similar between groups.
Table 1 depicts comparative analyses of the per capita income of children-adolescents families grouped according to the status of asthma control. Per capita income was lower in the families of subjects reporting uncontrolled asthma symptoms as compared to those reporting controlled symptoms (p 0.01), but there was no association between per capita income and inhaled corticosteroid need or airway obstruction in the spirometry test.
Comparative analyses of the family income between subjects grouped by markers of asthma control.
Financial values depicted in USD, inflated to June 2021.
Table 2 shows higher asthma costs in families of children and adolescents reporting uncontrolled asthma symptoms and in those reporting inhaled corticosteroids need, but there was no association between family costs of asthma and airway obstruction.
Comparative analyses of the family costs of asthma between subjects grouped by markers of asthma control.
Financial values depicted in USD, inflated to June 2021.
Families of children and adolescents taking inhaled maintenance therapy, and families of those reporting uncontrolled symptoms of asthma, were more likely to report any expenditure with asthma during the preceding month, even after adjusting the analyses for the per capita income [Adjusted OR 2.1; 95 CI (1.3-3.4) and Adjusted OR 3.1; 95 CI (1.5-6.3), respectively], while airway obstruction in the spirometry test was not associated with asthma expenditures (Supplementary Table 2).
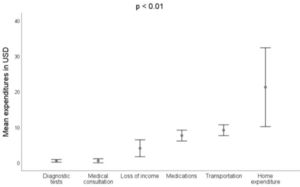
Fig. 2 shows a detailed description of the family costs of asthma in children and adolescents. The smallest expenditures were on diagnostic tests and medical consultations, while home expenditures to avoid triggers of asthma were the highest expenditures (p < 0.01).
DiscussionThe present study shows that non-controlled asthma in children and adolescents on regular outpatient care entails important economic consequences for their families. Families of children and adolescents reporting uncontrolled symptoms informed lower family income and higher family costs of asthma as compared to the families of children and adolescents reporting controlled symptoms. Meanwhile, families of children and adolescents who had taken inhaled maintenance therapy before enrollment in the study reported higher family costs of asthma as compared to the families of children and adolescents who had not taken maintenance therapy. Interestingly, there was no association between asthma costs and the presence of airway obstruction in the spirometry test, but our sample might be underpowered for this analysis. Notably, family income did not bias the relationship between markers of asthma control and asthma costs because the authors adjusted these associations in the regression models. This is the first study to our knowledge addressing this issue in this age range. One previous study demonstrated that initiating maintenance therapy for asthma was associated with 90% reduction in the family costs of asthma and a 20% increase in family income, but this study evaluated adult subjects with severe asthma who were on no previous health care.12 The present study'sresults have practical implications as they measure the effect of childhood and adolescence asthma on economic outcomes and support the necessity of public policies in low resource communities to minimize the economic impact of children and adolescents’ asthma.
In the present study, the family costs of asthma were similar between children-adolescents and adults. This observation contrasts with the lower per capita income in children and adolescents’ families and the better symptom score and spirometry test values in this age range as compared to adult subjects. Maybe parents of asthmatic children and adolescents were more inclined to invest family resources in the care of their offspring while adult subjects would be less prone to spend funds in the care of themselves. Additionally, detailed asthma expenditures differed between age ranges. Children and adolescents’ families reported higher costs with transportation to healthcare facilities than adults’ families, probably because they should acquire two transportation tickets, one ticket for the underage asthmatic subject and another ticket for the companion parent, while adult asthmatics could go to the healthcare facility without an escort. Conversely, families of adult asthmatics reported a greater loss of income due to asthma, probably because adult asthmatics who provide financial support for their families may be unable to work during asthma exacerbations; while families of children and adolescents with asthma might designate the most available family member to escort the asthmatic underage to the healthcare facility. Scrutinize the pattern of asthma expenditure is important as far as it provides information to guide the actions to minimize this problem, which could include free transportation pass to parents of asthmatic children and adolescents; and promote waive of payroll deduction for asthmatic adults who need to miss working days to take care of their asthma.
The detailed description of the expenditures with children and adolescents’ asthma shows that expenses with medical consultations and diagnostic tests were the smallest, probably because the public healthcare system was effective in providing these demands without charge. The expenditures with medications, however, were beyond expected if the authors take into account that short-acting bronchodilators, inhaled corticosteroids, and oral medications for asthma exacerbations have been providing free-of-charge under-medical-prescription in Brazilian public pharmacies since the year 2003. It is also noteworthy that the highest expenditures were on prevention of asthma triggers at home, which includes reforms, acquisition of air humidifiers, air cleaners, and others, which is understandable as these items are not provided by the government.
There are studies demonstrating that elderly asthma is more severe than adult asthma,15 but proper maintenance therapy prevents asthma exacerbations,16 minimizes loss of lung function and airway remodeling17 in both age ranges. In the current study, the authors provide evidence that childhood and adolescence asthma is associated with lower symptoms scores and better spirometry test values than adult asthma, thus showing that asthma severity is likely to get worse since the transition from adolescence to adulthood. This piece of information is meaningful as it supports strict control of childhood asthma.
Positive aspects of the present study are that the authors enrolled subjects across all disease severities and from all public healthcare facilities in the municipality. These study characteristics increase the external validity of the results. Limitations are that the authors cannot infer about the relationship between asthma control and family costs of asthma among subjects attended at private healthcare facilities, and the authors did not obtain prospective information to estimate the effect of asthma control changes on the household economy.
Finally, the authors conclude that asthma control affects the household economy in a population of children and adolescents. Future studies should investigate if the effect of asthma on the household economy affects the quality of life of asthmatic subjects and their families. The authors believe researchers should consider the possibility of assessing the household economy, in addition to other outcomes, when designing studies about asthma. Finally, our data support the necessity of public policies in low-resource communities to minimize the economic impact of children and adolescents’ asthma.
FundingThis study was funded by FAPESP (grant 2017/18367-9).
This study was conducted at the Faculdade de Medicina de Jundiaí, Jundiaí, SP, Brazil.