Emergence delirium is a common complication in children. Recorded mother's voice, as a non-pharmacological measure, is increasingly used to prevent the emergence of delirium in pediatric patients, but sufficient evidence is still needed to prove its efficacy.
MethodsEmbase, PubMed, Cochrane Library, Web of Science, CINAHL, and Sinomed databases were searched for randomized controlled trials exploring the efficacy of recorded mother's voice in preventing the emergence of delirium in pediatric patients undergoing general anesthesia. The original data were pooled for the meta-analysis with Review Manager 5.4.1. This study was conducted based on the Cochrane Review Methods.
ResultsEight studies with 724 children were included in the analysis. Recorded mother's voice reduced the incidence of emergence delirium when compared with either no voice (RR: 0.45; [95 % CI, 0.34 - 0.61]; p < 0.01; I2 = 7 %) or stranger's voice (RR: 0.51; [95 % CI, 0.28 - 0.91]; p = 0.02; I2 = 38 %) without increasing other untoward reactions. In addition, it shortened the post-anesthesia care unit stay time when compared with no voice (MD = −5.64; [95 % CI, −8.43 to −2.58]; p < 0.01, I2 = 0 %), but not stranger's voice (MD = −1.23; [95 % CI, −3.08 to 0.63]; p = 0.19, I2 = 0 %). It also shortened the extubation time and reduced the incidence of postoperative rescue analgesia.
ConclusionThe current analysis indicated that recorded mother's voices could reduce the incidence of emergency delirium, shorten post-anesthesia care unit stay time and extubation time, and decrease the incidence of postoperative rescue analgesia in children.
Emergence delirium (ED) is a common complication in children undergoing general anesthesia (GA).1 It is a mental disturbance during recovery from general anesthesia, which contains hallucinations, delusions, and confusion presented as moaning, irritability, involuntary physical activity, and thrashing around.2 The incidence of post-anesthesia ED is reportedly claimed to range from 10 to 80 % in children.3 Although it is typically temporary and resolved spontaneously, ED may cause clinically significant consequences, such as self-injury, unintended removal of indwelling vascular or urinary catheters, respiratory depression, prolonged length of post-anesthesia care unit (PACU) stay, and poor parental satisfaction.4,5 Therefore, appropriate methods are extremely needed to prevent ED in children under GA.
Currently, several anesthetics and sedatives including magnesium sulfate, dexmedetomidine, propofol, midazolam, and ketamine are being developed for the prevention of ED,4,6-9 however, they frequently prolong the recovery time and even cause drug-related side effects such as respiratory depression and postoperative nausea and vomiting (PONV), which limit their clinical application.9-11 In contrast, non-pharmacological methods, for instance, music therapy, acupuncture therapy, visual pretreatment, and clown doctors increasingly arouse people's interest,12-15 especially the recorded mother's voice, as a method with powerful feasibility and wide applicability, is proven to have a preventive effect on ED in several studies to date, but due to the small number of previous studies and individual opposite outcomes, its effectiveness still needed to be confirmed.
Thus, the authors carried out the current study with the objective of systematically collecting the existing literature regarding the efficacy of recorded mother's voice to prevent ED in pediatric general anesthesia procedures and applying meta-analysis to eligible outcome measurements, besides, the authors included PACU stay time, extubation time, postoperative rescue analgesia and possible adverse reactions as secondary outcomes to explore its effectiveness further.
MethodsThe meta-analysis was conducted and written in line with the principles of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement guidelines and registered on PROSPERO (CRD42023418332).
Study search and selectionTwo authors respectively searched Embase, PubMed, Cochrane Library, Web of Science, CINAHL, and Sinomed from database inception to March 2023 without language restrictions. A sensitive filter was used for randomized control trials (RCTs). The search terms included voice and emergence delirium. Details of the search strategy are in Supplemental Appendix 1. A manual search of the reference lists was conducted to seek missing RCTs. Another two researchers independently completed the preliminary screening based on titles and abstracts, and then the studies according to the eligibility criteria were included for full-text review. Any controversy about article selection or data abstract was resolved by consensus with the third reviewer.
Inclusion and exclusion criteriaStudies were included if the PICOS (population, intervention, comparison, outcomes, and study design) guideline were met: (a) Population: pediatric patients (< 18 years old) undergoing GA; (b) Intervention: perioperative use of recorded mother's voice; (c) Comparison: no voice or stranger's voice; (d) Outcomes: the incidence of ED, PACU stay time, extubation time, postoperative rescue analgesia and possible adverse reactions; (e) Study design: RCTs.
The exclusion criteria were as follows: (a) recorded mother's voice combined with other measures as an intervention group; (b) data were not able to meta-analysis; (c) unpublished materials or articles published in the form of summaries, reviews, case reports, letters and protocols. In case of sample overlap between studies, the authors retained the largest study.
Data extractionThe following data were abstracted: the first author, publication year, country, number of patients, age, surgical type, general anesthetics, anxiolytics, surgical and anesthesia time, intervention period, voice medium, the incidence of events or means and standard deviations of the outcome data, and the methods and criteria for the outcome data measurements. Two reviewers separately abstracted and cross-checked the data. If the variables were not reported in the articles, the authors would email the authors to request the data.
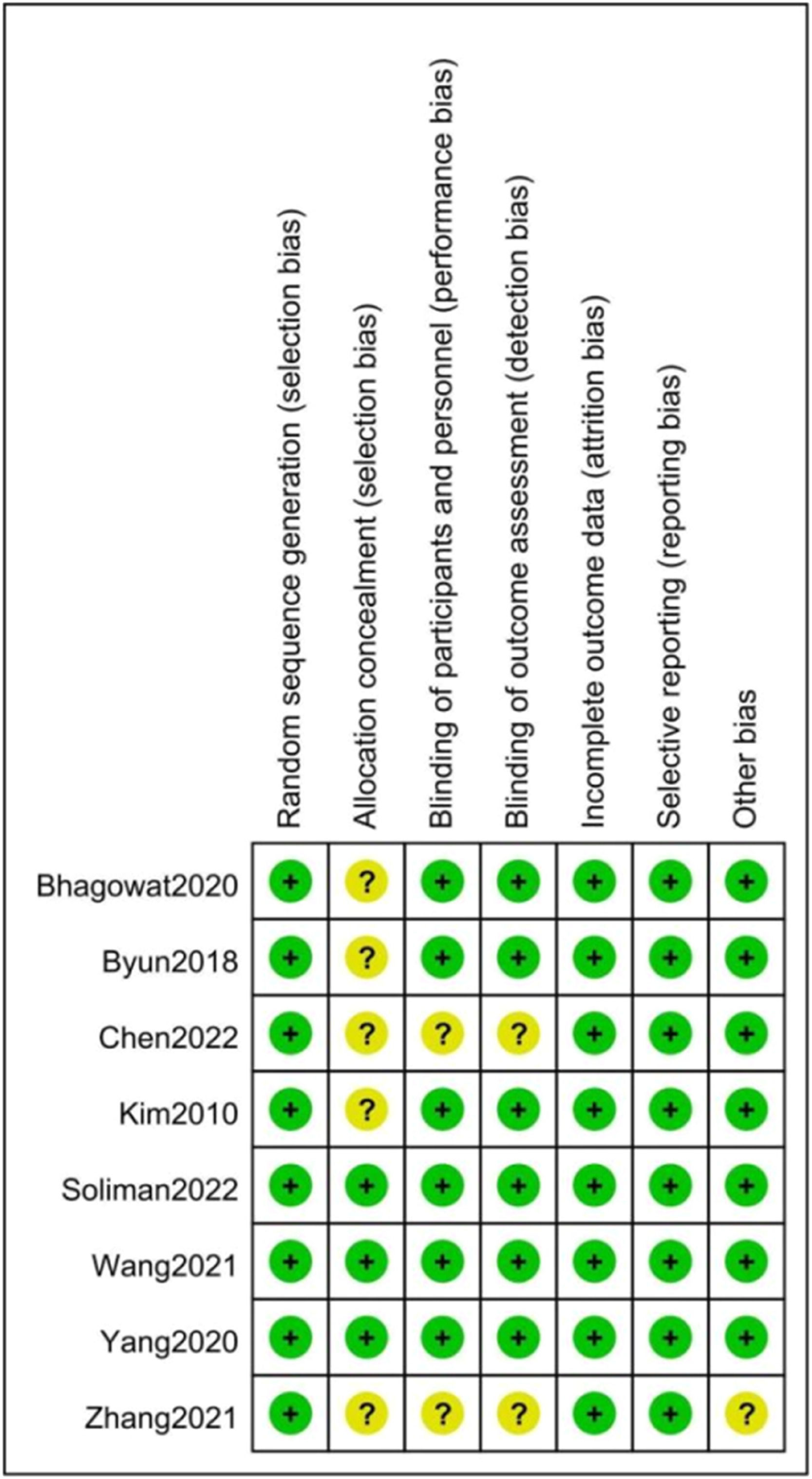
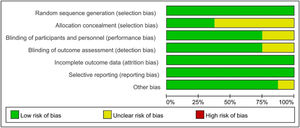
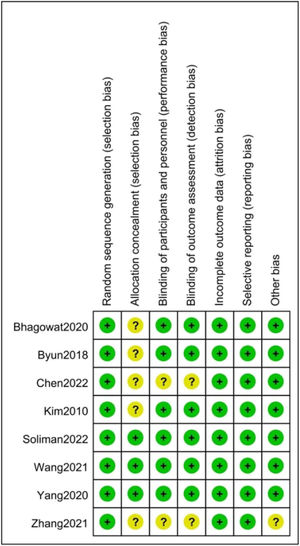
Quality assessmentThe methodological quality was evaluated by two researchers using the Cochrane risk of bias tool, which contained the methods of generating the random sequence, allocation concealment, blinding of personnel, participants, and assessors, incomplete results, selective reporting, and others. Each study was distributed to one of the three following risks: low risk (all quality criteria were completely coincided), moderate risk (one or more of the quality criteria were only partial match or unclear), or high risk (one or more of the quality criteria were not met or non-existent).16
Statistical analysisReview Manager 5.4.1 was used for the analyses of results. The standardized mean difference (SMD) and 95 % CI were calculated for continuous data with different units, and the mean difference (MD) and 95 % CI for the same units. A relative risk (RR) with the associated 95 % CI was used to analyze dichotomous data. For the overall effect, a P-value < 0.05 was considered statistically significant. I2 value and the Mantel-Haenszel method were employed to evaluate heterogeneity among studies. The data were pooled using a more conservative random effects model due to anticipated variations among included studies. I2 ≥ 50 % indicated strong heterogeneity between the studies. Subgroup analyses and sensitivity analyses were planned to explore the origin of heterogeneity. Sensitivity analyses were also designed to be performed in those studies with high risk.
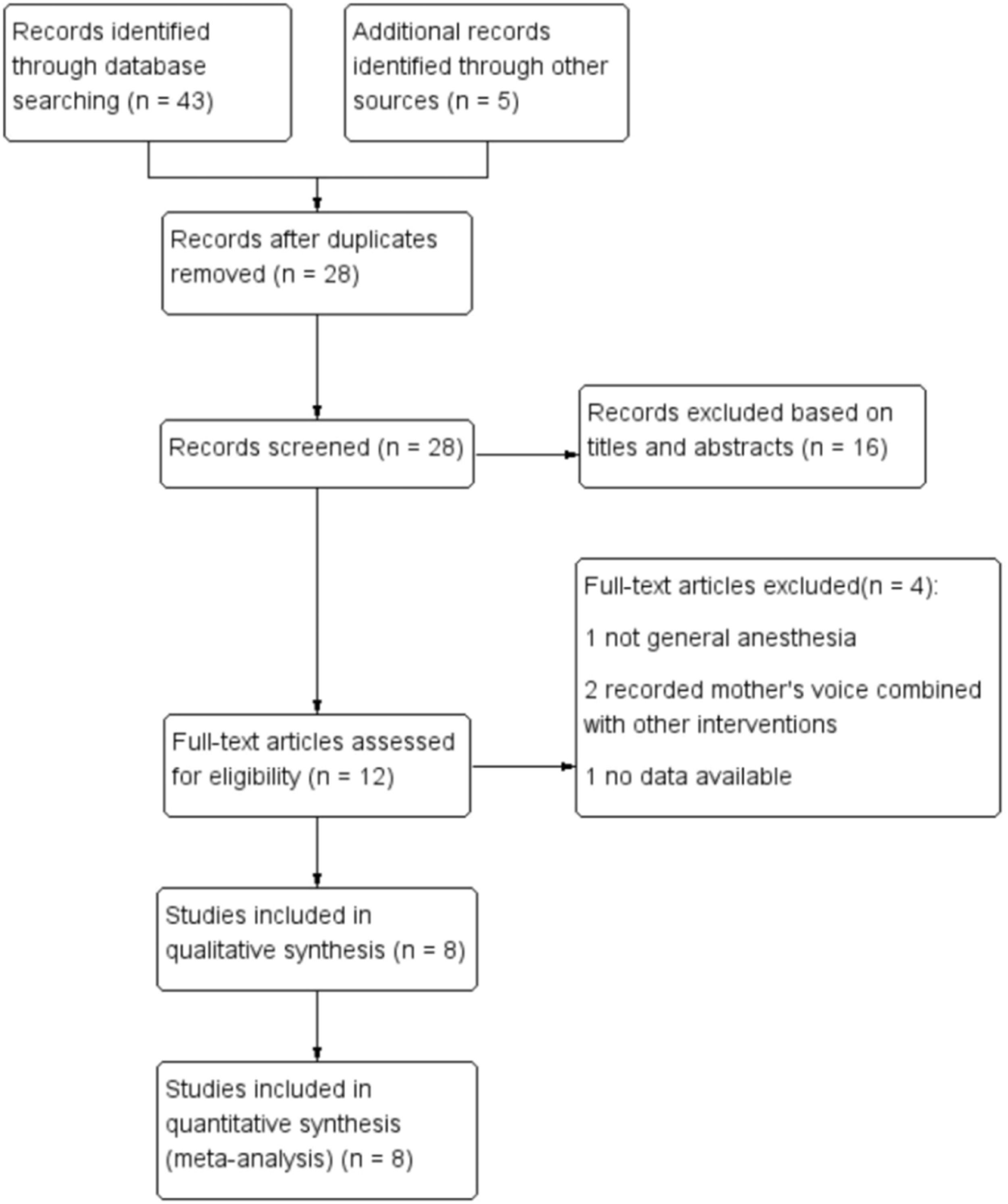
ResultsStudy identification and selectionThe initial search strategy identified 48 potentially relevant literature. After excluding 20 repeated articles, the authors further removed 16 kinds of literature by examining the titles and abstracts, and the remaining 12 studies were retrieved for the eventual determination of eligibility, of which 4 records were excluded. Consequently, the authors included 8 studies in this meta-analysis17-24 (Figure 1).
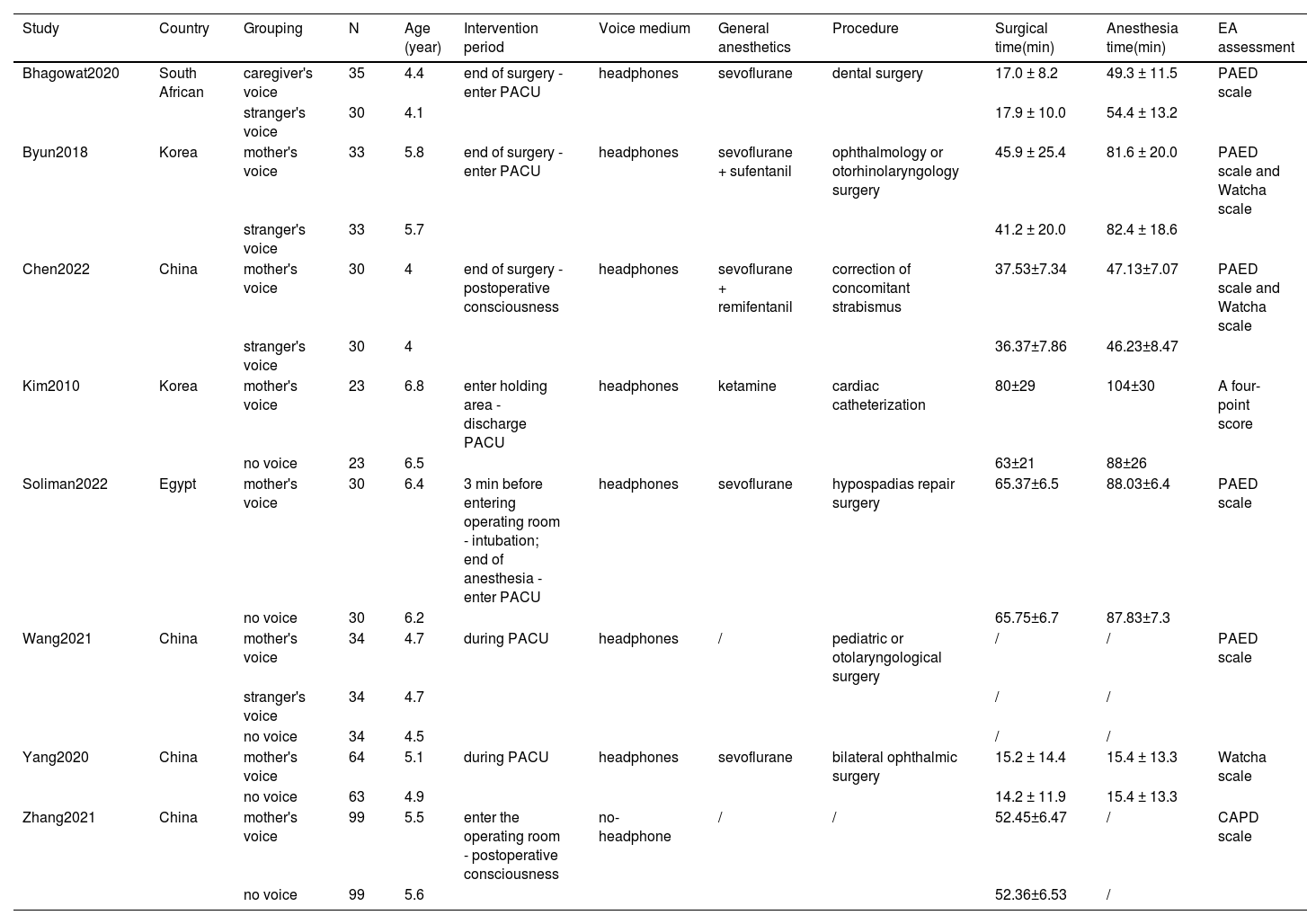
Study characteristicsTable 1 shows the basic features of the included studies. They were performed in four different countries, and all were published from 2010 to 2022. Children's average age ranges from 4 to 6.8 years. Four studies compared recorded mother's voice with no voice, and three studies compared recorded maternal voice with stranger's voice, in which a study indicated that the extended families played a critical role in child rearing and care locally, so they used the term ‘caregiver’ including both extended family members and parents,24 besides, one trial included three groups, in which the pediatric patients were randomized to either the use of recorded mother's voice, stranger's voice or no voice.18 The type of surgeries involved included ophthalmology, otolaryngology, dental, cardiac catheterization, and hypospadias repair. The type of general anesthetics included sevoflurane, ketamine, sevoflurane combined with sufentanil, and sevoflurane combined with remifentanil, unfortunately, only one trial showed the specific dosage.22 What's more, only one study mentioned the use of anxiolytics, in which ketamine was used before surgery.22
Characteristics of the included randomized-controlled trials.
PACU, post-anesthesia care unit; PAED scale, Pediatric Anesthesia Emergence Delirium scale; CAPD scale, Cornell Assessment of Pediatric Delirium scale.
A methodological quality assessment was conducted, and the results were shown in Figures 2 and 3. Two of the included RCTs were ranked low risk. Six were assessed to be moderate risk, the most frequent reason for unclear risk was selection bias (inadequate reporting of allocation concealment (n = 5)). In addition, there were 2 studies that reported performance bias and detection bias. To sum up, the quality of the 8 articles was low to moderate risk.
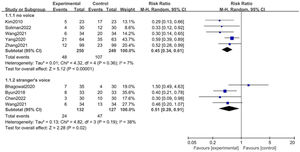
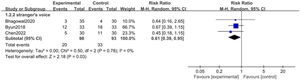
Primary outcomesAll studies involving 724 children provided data on ED. Using the Pediatric Anesthesia Emergence Delirium (PAED) scale for estimating ED in three studies,18,19,24 Watcha scale in one study,17 PAED scale combined with Watcha scale in two studies,20,23 whereas other studies used the assessment methods including Cornell Assessment of Pediatric Delirium (CAPD) scale21 and a four-point score (1: calm, 2: restless but could be easily appeased, 3: moderately agitated and not easily consoled, and 4: aggressive, confusion or thrashing about).22 Due to the authors only reporting the number of children at each score, the authors considered that children with a score of 3/4 had ED according to the Watcha scale. As the results showed, the number of presenting ED in children using a recorded mother's voice was significantly fewer than no voice (RR: 0.45 [95 %CI, 0.34 - 0.61]; p < 0.01; I2 = 7 %), what's more, when compared with stranger's voice, there was also significant difference with no significant heterogeneity (RR: 0.51; [95 % CI, 0.28 - 0.91]; p = 0.02; I2 = 38 %) (Figure 4).
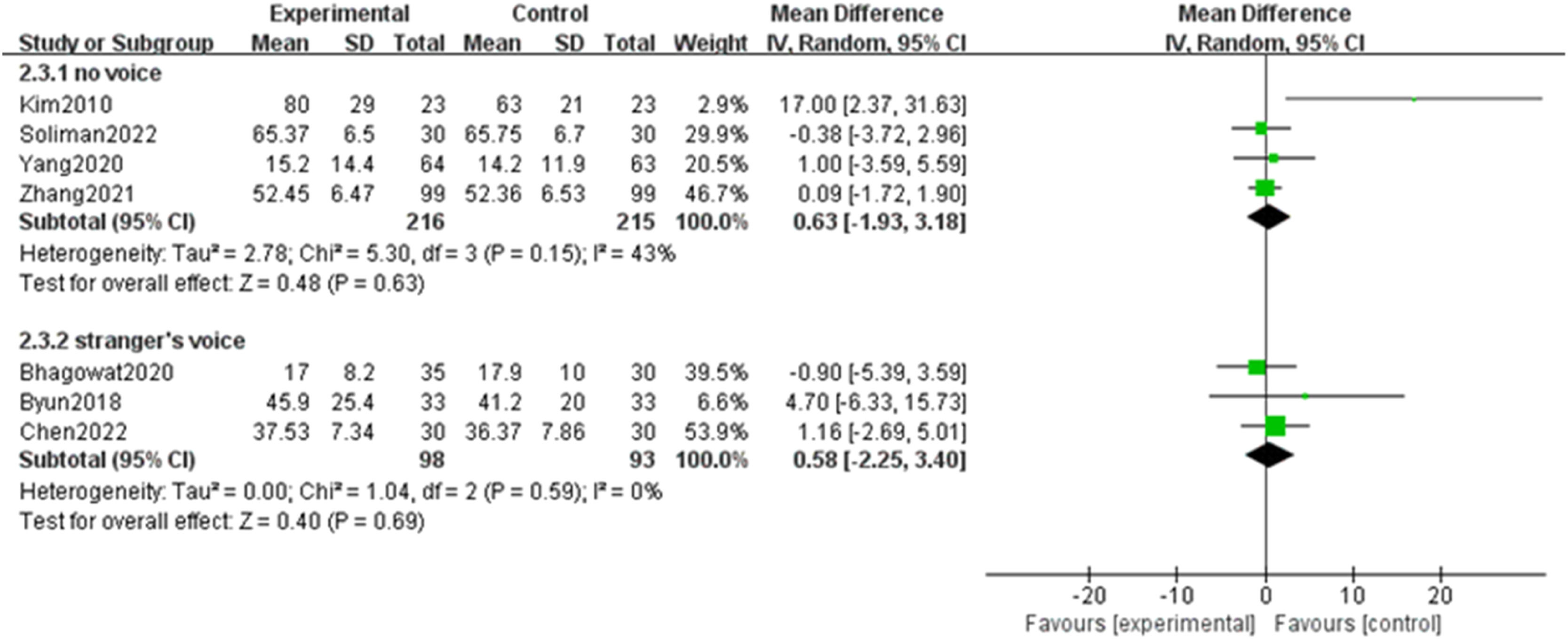
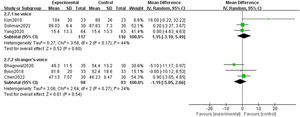
Secondary outcomesThe surgical time was reported in seven studies with 622 children. Our meta-analysis showed that there was no significant difference when compared with neither no voice (MD: 0.63; [95 % CI, −1.93 to 3.18]; p = 0.63, I2 = 43 %) nor stranger's voice (MD: 0.58; [95 % CI, −2.25 to 3.40]; p = 0.69, I2 = 0 %) (Figure 5). Six trials including 424 children provided data on anesthesia time, similarly, there was no significant difference when compared with neither no voice (MD: 1.15; [95 % CI, −3.19 to 5.49]; p = 0.60, I2 = 44 %) nor stranger's voice (MD: −1.19; [95 % CI, −5.05 to 2.66]; p = 0.54, I2 = 24 %) (Figure 6).
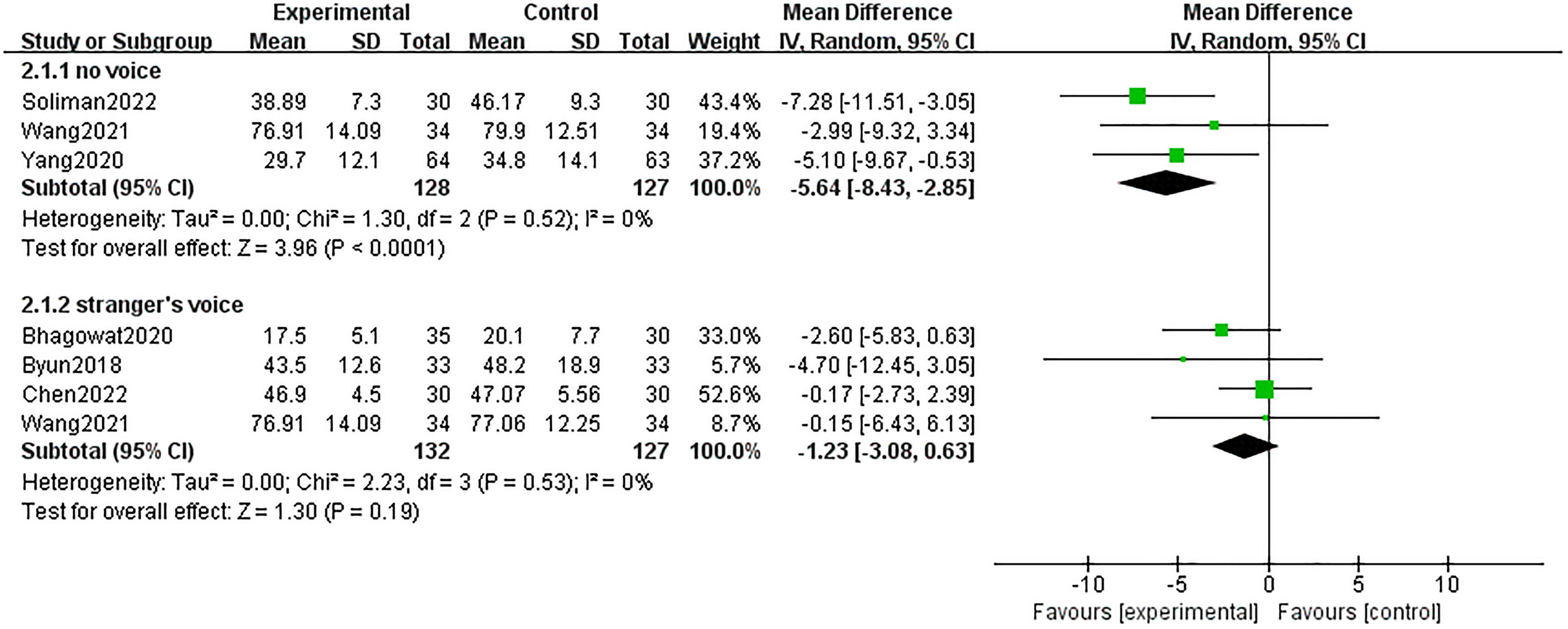
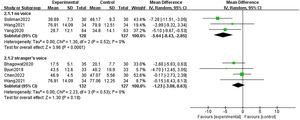
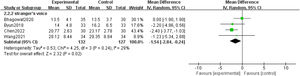
Six studies including 480 pediatric patients reported PACU stay time. Four of them used the Aldrete score as the method to assess the eligibility of discharging PACU, and one used the Steward Recovery Score (SRS) scoring system,18 when SRS was 4 or higher, children could be transferred out of the PACU. Compared to no voice, recorded mother's voice significantly reduced the PACU stay time (MD: −5.64; [95 % CI, −8.43 to −2.58]; p < 0.01), and almost no heterogeneity (I2 = 0 %). However, there was no significant difference when compared with a stranger's voice (MD: −1.23; [95 % CI, −3.08 to 0.63]; p = 0.19, I2 = 0 %) (Figure 7).
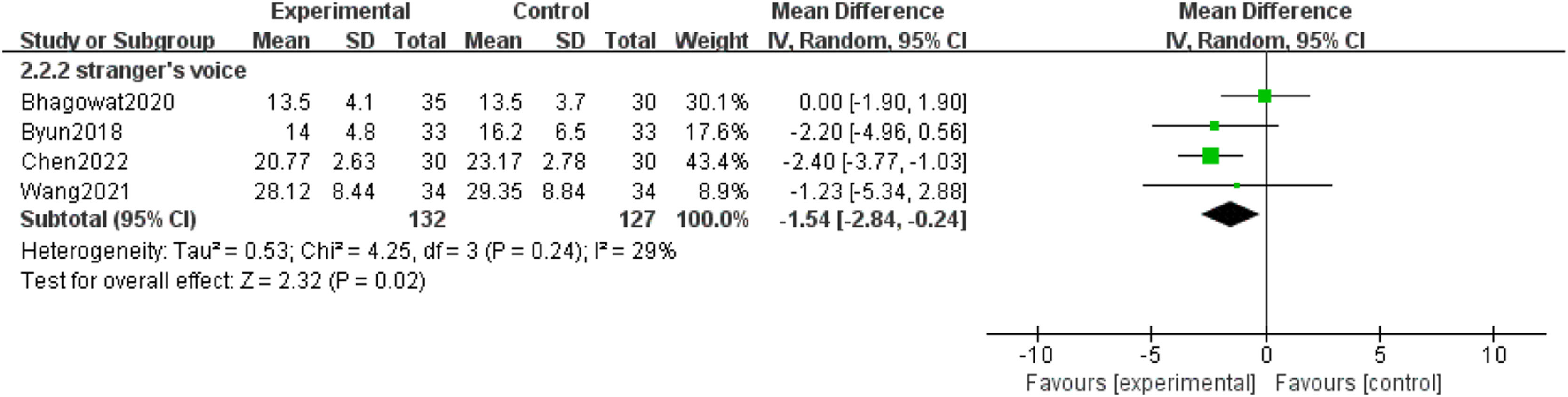
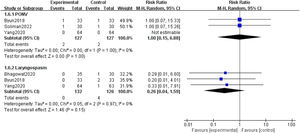
In total, four trials including 259 children provided data on extubation time. Our meta-analysis showed that there was a significant difference when compared with a stranger's voice (MD: −1.54; [95 % CI: −2.84 to −0.24]; P = 0.02, I2 = 29 %). However, the authors did not conduct a meta-analysis to compare the mother's voice with no voice because there was only one study18 (Figure 8).
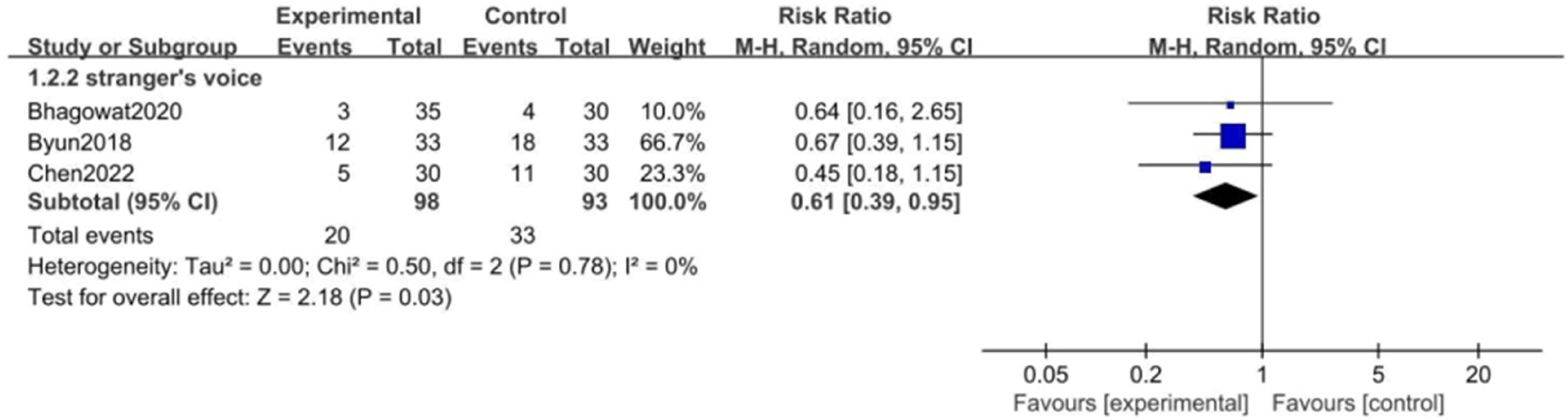
The incidence of postoperative rescue analgesia was reported in three studies with 191 children. They all used fentanyl as the rescue analgesia in PACU. There was a significant difference when compared with a stranger's voice (RR: 0.61; [95 % CI 0.39 - 0.95]; p = 0.03, I2 = 0 %) (Figure 9).
Individual studies had reported adverse reactions including laryngospasm and PONV, there was no significant difference, and the results are shown in Figure 10.
Subgroup analyses and sensitivity analysesThere was no significant heterogeneity in our analyses and no study was ranked high risk. Considering the diversity of intervention periods, the authors divided them into two categories, namely, simple postoperative intervention and postoperative combined intraoperative and/or preoperative intervention, then there were five trials in the simple postoperative intervention group,17,18,20,23,24 three trials not.19,21,22 Subgroup analyses based on intervention periods showed that using the mother's voice only during the postoperative period also reduced the incidence of ED and PACU stay time (Supplemental Fig. 1). Besides, a post hoc sensitivity analysis was conducted to examine the effect of headphones. One trial did not use headphones during the case, while all other trials used headphones as the voice medium.21 After excluding the no-headphone trial, the sensitivity analysis demonstrated that the mother's voice still reduced the incidence of ED (RR: 0.41; [95 % CI, 0.27 to 0.62]; p < 0.01; I2 = 29 %) (Supplemental Fig. 2).
DiscussionThe current meta-analysis was the first to research the utility of recorded mother's voices on ED in pediatric patients after GA. Here, our outcomes suggested that recorded maternal voice could significantly decrease the incidence of ED, shorten the PACU stay time and extubation time, and reduce the incidence of postoperative rescue analgesia. However, due to the low quantity of the trials and the clinical differences, caution should be mentioned while interpreting the results.
Children had a strong dependence on their parents, especially mothers, so they were more prone to ED after surgery as a result of separation anxiety from their mothers.25 Nevertheless, parental presence during induction of anesthesia or parent presence recovery program, as solutions to the above problems, remained controversial.26-29 On the one side, the presence of parents might add to medical workers’ management burden and increase the risk of potential infection. On the other side, it was reported that 74 % of parents especially mothers frequently experienced preoperative anxiety due to concerns about their children.30 By contrast, the recorded mother's voice with an accompanying effect like the presence of mothers could avoid these concerns. As previous research showed, recorded maternal voice for children undergoing cardiac catheterization was associated with a greater reduction of maternal anxiety perioperatively,22 which might be attributed to more participation in the process of medical care for their children. Furthermore, it was reported that maternal anxiety was one of the risk factors for ED in pediatric patients,31 as it aggravated preoperative anxiety in children.32 Similarly, our meta-analysis suggested that recorded maternal voice might be an effective strategy to decrease the number of children with ED after GA. Interestingly, the recorded mother's voice also shortened the PACU stay time and extubation time in children undergoing GA.
The mechanism of the mother's voice to prevent ED was still unclear, probably being associated with children's positive emotional responses induced by the mother's voice. As shown in an animal experiment, during parental separation, the mother's voice suppressed the separation-induced up-regulation of receptors in specific areas of the brain such as hippocampus and amygdala, and thus increased the autonomic stability.33 Another study reported that mothers' voices increased children's ability to interact with others by eliciting greater activity in primary auditory regions compared to stranger's voices.34 Further research were needed to confirm the association between the mother's voice and physiological changes in children undergoing GA and then explore the wider clinical application of the mother's voice.
Postoperative pain was one of the risk factors hindering the recovery of children from GA, nearly 45 % of children with ED experienced pain during the early period of awaking.35 Uncontrolled pain might contribute to maladaptive behaviors, increase costs, and exert a negative impact on mental health.36,37 Nowadays, non-pharmacological techniques are increasingly used to reduce pain due to being simpler and safer compared with drugs.14,38 In the current analysis, a recorded mother's voice could reduce the incidence of postoperative rescue analgesia, and previous studies showed that the incidence of postoperative rescue analgesia could reflect the postoperative analgesic effects.39,40 The reason why a mother's voice had an analgesic effect might be the fact that it could divert children's attention and then reduce pain-related stress.41
Interestingly, our results suggested that compared to a stranger's voice, the recorded mother's voice did not shorten PACU stay time. Based on this discovery, the authors speculated that the unique role of recorded maternal voice might work in the early stage of consciousness recovery without a sustained effect, by comparison, soothing and encouraging language, no matter who it came from, might play a critical role in maintaining children's emotional stability. However, the presumption required a longer follow-up to confirm. Another interesting point was the use of recorded maternal voice only during the postoperative period might be sufficient to prevent ED and promote children's recovery after GA, but further research is needed to confirm whether preoperative intervention could prevent ED.
LimitationsThe current study had some shortcomings. First, the sample sizes of studies were relatively insufficient, which might bias our results. Second, age, procedure, anesthesia, anxiolytics, and evaluation scales were the potential bias-inducing factors, therefore, the authors used a random effect model in our meta-analyses to avoid these biases, but the authors could not employ adequate subgroup analyses to explore more appropriate intervention options due to the small number of eligible studies. Third, the authors could not evaluate the long-term effects of the recorded mother's voice because nearly none of the included studies reported relative long-term evaluation indicators such as the incidence of postoperative delirium and the length of hospital stay.
ConclusionThis meta-analysis provided new evidence for the efficacy of recorded mother's voice on ED in pediatric patients after GA. In summary, the outcomes suggested that maternal voice could significantly reduce the incidence of ED, shorten the PACU stay time and extubation time, and decrease the incidence of postoperative rescue analgesia. The method was promising in clinical practice due to its safety and simplicity. However, considering the existing limitations, further studies are needed to support the clinical benefits of recorded maternal voice in ED of pediatric patients after GA.