To present signs and symptoms and clinical course in cystic fibrosis patients with false-negative newborn screening (CF NBS).
Materials and methodsAll children presented in this paper were covered by CF NBS. The group of 1.869.246 newborns was screened in the Institute of Mother and Child in Warsaw within a period of 01.01.1999 – 31.05.2019. Screening protocols evolved over time from IRT/IRT to IRT/DNA/EGA.
ResultsThe authors identified 11 patients with false-negative NBS, in whom CF was diagnosed based on clinical symptoms or the examination of siblings with positive CF NBS. In the study group, the diagnosis was made significantly later in comparison to positive CF NBS patients ranging from 2 months to 15 years of age. CF NBS strategy does not significantly affect the sensitivity of the screening.
ConclusionIn the presence of clinical symptoms, additional diagnostics must be implemented, in spite of the negative screening results. At first, the sweat test should be conducted, followed by a DNA analysis of the most common mutations in the given population. The diagnostic process requires searching for CFTR mutations not typically associated with a high chloride concentration in sweat. Repetition of sweat chloride concentration enables the diagnosis in children whose initial chloride values in sweat are borderline, and no CF-causing mutations are detected. In strong clinical indications, the extension of DNA analysis (EGA) is recommended in order to identify rare CF variants. In children with meconium ileus, genetic analysis is mandatory.
Cystic fibrosis (CF) has a profound impact on both quality of life and life expectancy; hence early detection is a priority to improve patient outcomes. Additionally, it opens a window to early therapeutic interventions. A milestone in the development of diagnostics for CF and the introduction of cystic fibrosis screening (CF NBS) was the detection of elevated immunoreactive trypsinogen levels (IRT) in CF patients in 1979.1 Ten years later, the CF transmembrane conductance regulator (CFTR) gene was discovered.2-4
Elevated IRT in the serum of newborns with CF as a consequence of pancreatic injury suggests CF but is not pathognomic for this entity. The IRT assessment is the first stage of contemporary CF NBS protocols worldwide. In subsequent phases, the options are to analyze IRT a second time, find pancreatitis-associated proteins (PAP) or perform molecular DNA analysis with the different range of variants.5,6 Tests are carried out using dried blood spots collected from newborns. Different approaches are utilized in different countries.
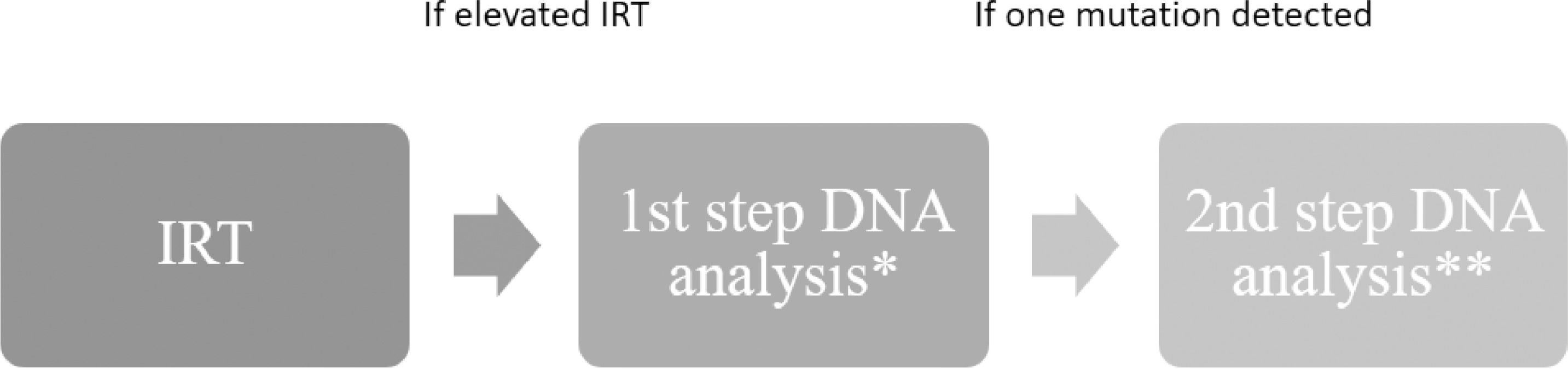
The CF NBS enables early diagnosis in asymptomatic or poorly symptomatic newborns (e.g. slightly weaker weight gain) after a positive result. Detection leads to the implementation of appropriate treatment and brings health benefits: better respiratory outcomes and the prevention of severe malnutrition.7-10 Unfortunately, some children with CF are not diagnosed by screening programs, just as in the neonatal screening programs for other disorders.11 Over the past 20 years, the Polish screening program has undergone modifications, which increased the number of detected mutations. Currently, CF NBS in Poland includes an expanded genomic analysis what theoretically should reduce the number of false-negative cases (Figure 1). Nevertheless, it should be remembered that false negatives still occur due to the correct first stage of screening (normal IRT).
Current newborn screening model in Poland (IRT/DNA/EGA).
The aim of the study was to present signs and symptoms, clinical course, and CFTR variants in cystic fibrosis patients with false-negative newborn screening (CF NBS) in Poland.
Materials and methodsCF NBS was implemented initially as a pilot study in 4 Polish districts in 1999 and was suspended in August 2003. In September of 2006, after a 3-year break, CF NBS was resumed in the same districts. In the following years, the program was gradually expanded, and by June 2009, it was implemented in the whole country. During the pilot study, 444.063 newborns were examined. Subsequently, from September 2006 to May 2019, in the same area, 1.425.183 newborns were tested (in total, 1.869.246). All the children presented in this paper were covered by CF NBS between January 1999 and May 2019.
In the study period screening algorithm and CFTR mutation panel was modified over time. The following models were implemented: IRT/IRT, IRT/IRT/DNA with a gradually expanded panel of mutations from the most common F508del to 17 of the most frequent mutations, covering in first stage 675 mutation by Sanger method.12 Modifications of the CF NBS scheme have been described previously in detail.13 Finally, an expanded genetic analysis (EGA) was implemented to reach the IRT/DNA/EGA model. I this strategy, initially, IRT analysis was performed in every patient. If IRT exceeded 99.4 percentile (specific value depended on the kit), genetic analysis was further performed. Samples with normal IRT were not further tested. Regardless of the IRT level, DNA analysis was carried out in patients with meconium ileus (MI). This allowed identifying 97% of mutated alleles of the CFTR gene in the Polish population.14 Sensitivity was calculated as the number of true positive NBS results divided by the total CF population. According to the arrangements for the Polish NBS program, information about MI should be reported to the screening laboratory.
In this paper, the authors defined a positive screening result as an increase in IRT between 3-5. day and also at week 4 for the IRT/IRT scheme. For other schemes, the result was positive if a child with elevated IRT had been detected with at least one CFTR gene mutation. Each child with a positive screening result was summoned to the CF center where specialist consultations and sweat tests were conducted according to standards.15 The late diagnosis was defined as a failure to diagnose CF subsequent to screening a month after birth. All caregivers gave their informed consent before inclusion into the cystic fibrosis newborn screening, performing DNA analysis, and all diagnostic procedures. The CF NBS has been approved and supported by the Polish Ministry of Health. The study was also approved by Institutional Ethical Committee.
ResultsAmong children born and screened from 01.01.1999 to 31.05.2019, a late diagnosis of CF was made in 11 cases. The sensitivity of CF NBS in reference to time and method, was shown in Table 1. Detailed data for each patient is presented in Table 2. All patients were diagnosed based on clinical symptoms or the examination of siblings with positive CF NBS. In 10 cases, the IRT result was normal. In one case IRT concentration was elevated, however, the patient was not invited to a verification visit because DNA analysis showed no mutation of the CFTR gene (case 9). At diagnosis, the age range was from 2 months to 15 years of age.
Characteristics of the false-negative patients.
| Case/gender | Genotype (legacy /HGVS nomenclature) | Age of diagnosis [month] | Cause of the diagnostics | Clinical symptoms at the time of diagnosis | Subsequent sweat tests [mmol/L]a | Screening strategy |
|---|---|---|---|---|---|---|
| 1/M | F508del/R347Pc.1521_1523delCTT/ c.1040G>C | 63 | sibling with positive CF NBS | respiratory infectionscoughdigital clubbinglow body massdiarrhea, PI | 80,175,9 | IRT/IRT |
| 2/F | N1303K/del 2,3(21 kb)c.3909C>G/ c.54-5940_273+10250del21kb | 9 | respiratory infections low body mass | respiratory infectionsisolation PAcoughdiarrhea, PIlow body mass | 56,8131 | IRT/IRT |
| 3/F | c.3718-24G>A/? | 180 | pneumonia with isolation PA low body mass | respiratory infectionslow body mass | 70,654,334,060,382,470,852,467,870,7 | IRT/IRT/DNA (F508del only) |
| 4/F | F508del/2143delT c.1521_1523delCTT/c.2012delT | 3 | low body mass | MI, PIcoughlow body mass | 49,860 | IRT/IRT/DNA (F508del only) |
| 5/F | F508del/F508del c.1521_1523delCTT/ c.1521_1523delCTT | 2 | low body mass diarrhea | MI, PIdiarrhealow body mass | 76,9118 | IRT/IRT/DNA (47 mutations) |
| 6/M | R334W/R334Wc.1000C>T/ c.1000C>T | 162 | sibling with positive CF NBS | chronic rhinosinusitis | 70,072,2 | IRT/IRT/DNA (F508del only) |
| 7/F | ?/? | 72 | respiratory infections low body mass | respiratory infectionsdiarrhea, PIlow body mass | 53,765,368,9 | IRT/DNA/EGA |
| 8/F | F508del/3849+10kbC>T c.1521_1523delCTT/c.3717+12191C>T | 43 | respiratory infections cough | coughrespiratory infections | 6878,2 | IRT/DNA/EGA |
| 9b/M | S1347PfsX13/S1347PfsX13c.4035-4038dup/ c.4035-4038dup | 4 | respiratory infections low body mass | respiratory infectionslow body masscholestasisdiarrhea, PI | 76,194,496,8 | IRT/DNA/EGA |
| 10/F | 3849+10kbC>T/H199Rc.3717+12191C>T /c.596A>G | 8 | respiratory infections | coughrespiratory infectionslow body massmetabolic alkalosis | 60,563,069,166,8 | IRT/DNA/EGA |
| 11/M | F508del/F508del c.1521_1523delCTT/ c.1521_1523delCTT | 8 | respiratory infections low body mass | respiratory infectionsdiarrhea, PIlow body masscoughwheezing | 71,774,366,571,4 | IRT/DNA/EGA |
PI, pancreatic insufficiency; PA, Pseudomonas aeruginosa; M, male; F, female; HGVS, Human Genome Variation Society.
? - In CF NBS no mutations of the CFTR gene detected.
Two of the 11 children developed MI (cases 4 and 5), however, this fact was not reported to the screening laboratory, and adequate CF diagnostics was not initialized. During the diagnosis period, patients presented various clinical symptoms, most often recurrent respiratory infections, malnutrition, and diarrhea. Four patients remained pancreatic sufficient (cases 3, 6, 8 and 10). Their stools were normal, and the elastase-1 concentration was above 200 µg/g. In two female patients, 3849+10kbC> T mutations were identified in one allele (case 8 and 10) and in the second allele F508del and H199R, respectively. Mutation H199R was not described in the CFTR 2 database. The third pancreatic sufficient patient was R334W homozygote (case 6). In the fourth patient, despite sequencing of all exons and performing the MLPA, the presence of variants with unclear phenotypic consequences in one CFTR gene allele was confirmed (case 3).
Among the study group, in one fully symptomatic patient, the testing failed to detect mutations in both alleles (case 7). In all examined children, sweat chloride values were high, and DNA analysis, except for the cases mentioned earlier, enabled the detection of two mutations of the CFTR gene.
DiscussionAll the described children with late diagnosis underwent CF NBS. In 10 out of 11 examined patients, IRT was low, and screening test was discontinued (as described in Materials and methods). Thus, none of these 10 cases would have been detected by the screening, regardless of the type of strategy. Similarly, Sinclair et al. described 6 false-negative CF patients in the British Columbia NBS IRT/DNA/IRT program, of which 4 patients had normal IRT.16
In the present study, only in one case was IRT above the upper limit (case number 9). In this patient, despite the use of a broad genetic panel (675 variants), the first step of DNA analysis was negative, and the test was completed. EGA analysis (second step) was not performed, which, in this case, would identify both variants. Hitherto the IRT / EGA strategy is not utilized in Poland and, to our knowledge, in any EU country due to the high cost.17,18 After the appearance of symptoms and strong clinical indications, the extension of DNA analysis was performed and confirmed the presence of S1347PfsX13 variants in both alleles.
False-negative IRT in children with MI is a well-known phenomenon. However, many professionals who have occasional contact with CF patients are unaware of the need to report MI to a screening center. The authors emphasized the need to train neonatologists and pediatric surgeons in cystic fibrosis and the importance of feedback about MI occurrence.
Two of 11 (18%) described children presented MI, which was consistent with previous observations.19-21 It is well documented that newborns with CF and meconium ileus tend to have low initial IRT values, resulting in a false-negative outcome.22 For this reason, it is obligatory to include information about MI in a sampling paper. The failure to report this important information in both presented cases contributed to the late diagnosis of CF.
The S1347PfsX13 (nucleotide nomenclature c.4035_4038dupCCTA protein nomenclature p.Ser1347ProfsTer13) mutation leads to duplication of four nucleotides in exon 22, which results in a frameshift and premature introduction of STOP codon within NBD2 domain. This case indicates how the heterogeneity of the Polish population may cause difficulties in the diagnostic process. It is important to underline the need to carry out early diagnostics in patients with negative NBS who have typical CF symptoms.
In homozygous S1347PfsX13 patients the cause that initiated the process of diagnosis for CF was cholestasis. A similar case was described by Heidendael et al.23 in a child born prematurely in 27th week of gestational age. The newborn was covered by CF NBS, and symptoms of the underlying disease were overlapped by complications related to prematurity and the consequences of MI. Cholestasis occurred at 5 weeks of age, after a 3-week period of total parenteral nutrition after MI surgery. These problems caused the delay in diagnosis, which was finally confirmed at the age of 10 weeks by genetic findings (two pathogenic F508del and N1303K mutations). In the studied patient, cholestasis as the predominant symptom was accompanied by recurrent respiratory infections and the presence of fat in stools. Of note, no relation between IRT and cholestasis levels has been found in the literature.
Significant body mass deficiency can affect sweat test values. The interpretation of sweat test results may raise doubts if the body mass deficiency is found in patients with negative CF NBS results. Dunn et al. described the diagnostic difficulties of a one month-old boy, homozygous F508del mutation.24 Elevated sweat tests were combined with other diseases which could lead to malnutrition. The treatment changed after obtaining the result of DNA analysis and elastase-1 concentration in the stool. In several of the studied cases, the leading symptom initiating the diagnostics procedure was malnutrition. The age of diagnosis in these cases was significantly higher. In case 1 the boy was diagnosed at the age of 5. He presented with evident symptoms of pancreatic insufficiency and digital clubbing. His chest X-ray showed changes characteristic for cystic fibrosis: distension and peribronchial thickening. However, the diagnosis process was initiated after a positive CF NBS result in a younger sibling. Neemuchwala et al. described a case of CF diagnosis in a child with false-negative CF NBS25 with a similar history. Although their case presented a younger child, his radiological changes were more advanced.
Serious problems preceded the diagnosis in a girl (case 3) who had significant body mass deficiencies, gastroesophageal reflux disease but without accompanying diarrhea. The diagnostic process was introduced after the occurrence of pneumonia and isolation of Pseudomonas aeruginosa. Sweat tests carried out in subsequent years initially showed borderline results. At the age of 15 they reached values above 60 mmol/l. The further follow-up did not reveal pancreatic insufficiency. The chest X-ray and CT showed the presence of bronchial thickening. She had pulmonary exacerbations 3-4 times per year. No CFTR gene mutation was identified except for the variant with unknown clinical consequences (c.3718-24G>A), although the genetic examination included a panel of mutations enabling detection of 97% of mutated alleles in the Polish population as well as MLPA. In this situation, it was helpful to repeat the sweat tests several times.
In conclusion, newborn screening is a highly reliable (sensitivity 94-97%) screening tool for an early diagnosis of cystic fibrosis.13 It provides the opportunity to postpone the progression of the disease and avoid associated complications. When patients present clinical symptoms characteristic of cystic fibrosis, the CF diagnostics must be implemented, in spite of the negative result of screening. At first, the sweat test should be conducted. In patients with an abnormal concentration of electrolytes in sweat, DNA analysis is the next step to perform with a panel of the most common mutations in the population. The CF diagnosis is very important in siblings of children diagnosed previously. The diagnostic process requires consideration and caution. Professionals should take into account the possibility of mutations not typically causing a high chloride concentration in sweat.
Sweat chloride concentration measured by quantitative pilocarpine iontophoresis is a useful diagnostic test. Thanks to its repetition during subsequent months of observation, the finding of increased electrolyte concentration in sweat enabled the diagnosis in a child whose initially sweat tests were borderline and two pathogenic CFTR gene mutations were not isolated.
Annotation about MI on screening paper accelerates the diagnostic process and allows quicker diagnosis in children with normal IRT results.