To evaluate neonatal autopsy rates at a tertiary hospital in southern Brazil ascertain the level of agreement between premortem and postmortem diagnosis.
MethodsThe authors reviewed all neonatal autopsies performed over a 10-year period and described the percentage of neonates who died and underwent autopsy. The authors tested for agreement between autopsy findings and the cause of death as defined by the neonatologist. Agreement between clinical diagnosis and autopsy findings was classified using the modified Goldman criteria. Additional findings at autopsy were grouped by organ system. Linear regression and multiple comparisons were used for statistical analyses.
ResultsDuring the study period, 382 neonates died at the Neonatal Intensive Care Unit (NICU). Consent to perform an autopsy was obtained for 73 (19.1%). The complete agreement between autopsy findings and the neonatologist's premortem diagnosis was found in 48 patients (65.8%). Additional findings were obtained at autopsy in 25 cases (34.2%). In 5 cases (6.9%), the autopsy findings contributed to subsequent genetic counseling. Seven autopsies (9.6%) revealed a diagnosis that would have changed patient management if established premortem. The autopsy rate increased by an average of 1.87% each year.
ConclusionDespite a high level of agreement between clinical diagnosis and pathological findings, autopsies provided relevant data regarding the cause of death, providing additional clinical information to neonatologists and allowing genetic counseling of family members.
Despite the emergence of new technologies, autopsy remains an important tool in the investigation of neonatal death, contributing to the ascertainment of the definitive cause of death and disclosing associated findings that were not suspected before death. 1 A neonatal autopsy is a marker of patient care and can provide vital information for neonatologists and family members about the cause of death, as well as on the accuracy of premortem clinical diagnosis.2,3
Several studies have assessed the importance of neonatal autopsy.4-10 Brodlie et al.11 reported that 25% of neonatal autopsies added some new information to the premortem clinical diagnosis, and in 3% of cases, this information was essential for diagnostic elucidation. In agreement with these findings, other studies reported that important additional information was found in 22 to 81% of perinatal autopsy cases. 9 Equally important are the divergences between clinical and pathological findings, occurring in 3-5% of patients, 12,13 even at a level IV NICU (Neonatal Intensive Care Unit).
Recently, magnetic resonance imaging (MRI) has been suggested as an adjunct to or even a substitute for autopsy. However, much of the additional information found at autopsy would likely be missed by postmortem MRI.3
The performance of neonatal autopsies, in addition to acting as a tool for quality control of patient care, improves the parents’ understanding of the cause of death and provides information for genetic counseling, including the risk of recurrence.14 Disclosure of initially unknown causes of death contributes to the continued improvement of neonatal care. The authors could not find any previous reports of neonatal autopsy rates in Brazil, which justifies this study.
In this context, the present study aims to assess the prevalence of neonatal autopsies in a single tertiary center in the last ten years, describe the level of agreement between clinical diagnosis and autopsy findings, and report on additional findings disclosed by postmortem examination.
MethodsThe authors conducted a retrospective study to evaluate the agreement between the causes of neonatal death attributed by the clinician prior to the postmortem examination and the findings at autopsy. The authors used a convenience sample consisting of all neonates who died in the NICU at Hospital de Clínicas de Porto Alegre and underwent autopsy from January 2008 to December 2018. The hospital has a level III NICU and is a referral center for high-risk pregnancies and those requiring fetal medicine follow-up.
The research project was approved by the institutional Research Ethics Committee, no. 2019-0744. The clinical diagnosis and the cause of death were obtained from patients’ electronic medical records, while the autopsy finding was obtained from the pathologist's report. All autopsies were performed by a qualified pathologist (RCR) with experience and skill in neonatal autopsies, following the institution's standardized protocol, and were only performed after authorization and written informed consent had been obtained from parents or legal guardians. Each autopsy included a thorough external examination, open dissection, and gross and microscopic (histological) examination of all organs. The external examination included whole-body photographs (front and side views) and close-up shots of any external abnormalities if present. Whole-body radiographs were used to detect any skeletal deformities. The weight of each organ was evaluated in relation to the expected mean for gestational age, and tissue samples from each organ were collected for histological examination.15 In all cases, a clinical geneticist was present at the start of the procedure to assist in and guide external examination, as well as to collect material for karyotyping and DNA extraction.
Clinical causes of death were classified among those most common in the neonatal period: prematurity and related conditions (immaturity, respiratory distress syndrome, necrotizing enterocolitis, intra/periventricular hemorrhage), pulmonary hemorrhage, perinatal asphyxia, central nervous system (CNS) disorders, blood diseases, congenital malformations and genetic syndromes, neonatal sepsis, and congenital infections. Comparisons between premortem clinical diagnoses and autopsy findings were made by two experienced neonatologists (ALC and CRH) and classified according to Kumar's modification16 of Goldman's system2 as below:
IA - Diagnosis that, had it been detected before death, would probably have to change in management that might have resulted in cure or prolonged survival.
IB - Diagnosis with significant implications for future genetic advice.
II - Diagnosis that, had it been detected before death, would probably not have led to change in management or survival because:
- •
No appropriate therapy was available at the time;
- •
Appropriate therapy was given even though the diagnosis was unknown at the time;
- •
Patient had an acute cardiopulmonary arrest that was appropriately managed, but the patient did not survive for definitive management;
- •
Patient had a “do not resuscitate” status.
III - Diagnosis that may not have been related to the main disease process and was a contributory cause of death.
IV - Diagnosis unrelated to the outcome and may or may not have affected the eventual prognosis of the patient.
V - Complete concordance between diagnosis before death and findings at autopsy.
This classification divides autopsy findings into major additional findings (classes I and II) and minor additional findings (classes III and IV). Major additional findings are underlying diseases or primary causes of death. Minor additional findings contain related diagnoses, contributory causes, antecedent conditions, or other important conditions. Additional findings disclosed at autopsy were classified into organ systems (cardiovascular, gastrointestinal, endocrine, respiratory, and neurological), genetic abnormalities, sepsis, and congenital infections.
The autopsy report was delivered to the parents during a face-to-face visit with the examining pathologist.
Statistical analysisStatistical analysis was performed in SPSS Statistics, Version 22.0. Continuous variables were expressed as mean and standard deviation or median and interquartile range. Categorical variables were expressed as absolute and relative frequencies. Student's t-test or the Mann–Whitney U test (in case of asymmetrically distributed data) were used to compare means. The chi-square test or Fisher's exact test were used to compare proportions. Statistical evaluation of agreement was not performed because the Goldman system is a qualitative approach to evaluate the agreement between clinical conclusions and pathologic findings of causes of death. To assess the behavior of the autopsy rate over the years during the period of analysis, a simple linear regression model was used. The significance level was set at 5%.
ResultsDuring the study period, 382 neonates died in the NICU. Permission for autopsy was obtained for 73 patients (19.1%), and these were all included in the study. The median age at death was one day (0- 11 days). The most frequent clinical causes of death were genetic syndromes and congenital malformations (54.8%), prematurity (20.5%), and sepsis (13.7%). Mean gestational age at birth was 32.8 (± 5.6) weeks, and the mean birth weight was 1862 (± 1012) g; 67.6% of patients were born preterm. The characteristics of the included patients are described in Table 1.
Patient characteristics.
| Characteristics | N |
|---|---|
| Sex | |
| Malea | 30 (41.1%) |
| Femalea | 43 (58.9%) |
| Mother's age (years)b | 25.3 (± 7.2) |
| Gestational age (weeks)b | 32.8 (± 5.6) |
| Type of pregnancya | |
| Singleton | 69 (94.5%) |
| Multiple | 4 (5.5%) |
| Mode of deliverya | |
| Vaginal delivery | 31 (42.5%) |
| Cesarean section | 42 (57.5%) |
| Birth weight (grams)b | 1862 (± 1012) |
| Delivery room resuscitationa | |
| Yes | 51 (69.9%) |
| No | 20 (27.4%) |
| Apgar scorec | |
| 1-min | 2 (1; 5) |
| 5-min | 5 (1; 7) |
| Postnatal age at death (days)c | 1 (0; 11) |
| Mechanical ventilationa | 56 (76.7%) |
| Early sepsisa | 31 (42.5%) |
| Late-onset sepsisa | 24 (32.9%) |
| Genetic syndromesa | 19 (26%) |
| Congenital malformationsa | 42 (57.5%) |
Table 2 reports the agreement between premortem clinical findings and diagnosis at autopsy. There was complete concordance between pathological and clinical diagnosis in 48 cases (65.8%). In 25 cases (34.2%), the pathologist described additional findings obtained at autopsy. Of the additional findings, 80% were Class I and II and 20% were Class III and IV. In 5 autopsies (6.9%), findings contributed to subsequent genetic counseling (class IB). Furthermore, 7 autopsies (9.6%) revealed important information that would have changed patient management (class IA), potentially leading to cure and/or increased survival if diagnosed before death. Of these seven patients, five had a clinical diagnosis of congenital malformation, and the additional findings at autopsy were purely cardiological (hypoplastic left heart syndrome, heart failure due to early closure of the ductus arteriosus, cardiac tamponade, and aortic stenosis). Two of these seven patients had a clinical diagnosis of sepsis, while the autopsy findings were coarctation of the aorta and congenital herpes infection.
Additional findings by the pathologist were classified using the Goldman criteria and described according to the clinical cause of death (Table 3). Given the above, the authors observed no statistically significant association between the clinical cause of death and the Goldman classification (p = 0.206), indicating that agreement between premortem and postmortem findings was independent of the cause of death.
In the 25 patients with additional findings at autopsy, cardiovascular system abnormalities were most common (48% of cases), followed by malformations and genetic syndromes (20%) and CNS changes (12%). Changes in the gastrointestinal (8%), respiratory (8%), and endocrine (8%) systems were less frequent. Neonatal sepsis and congenital infections occurred in 4% of cases, respectively. In addition, 2 out of 25 patients had more than one additional finding.
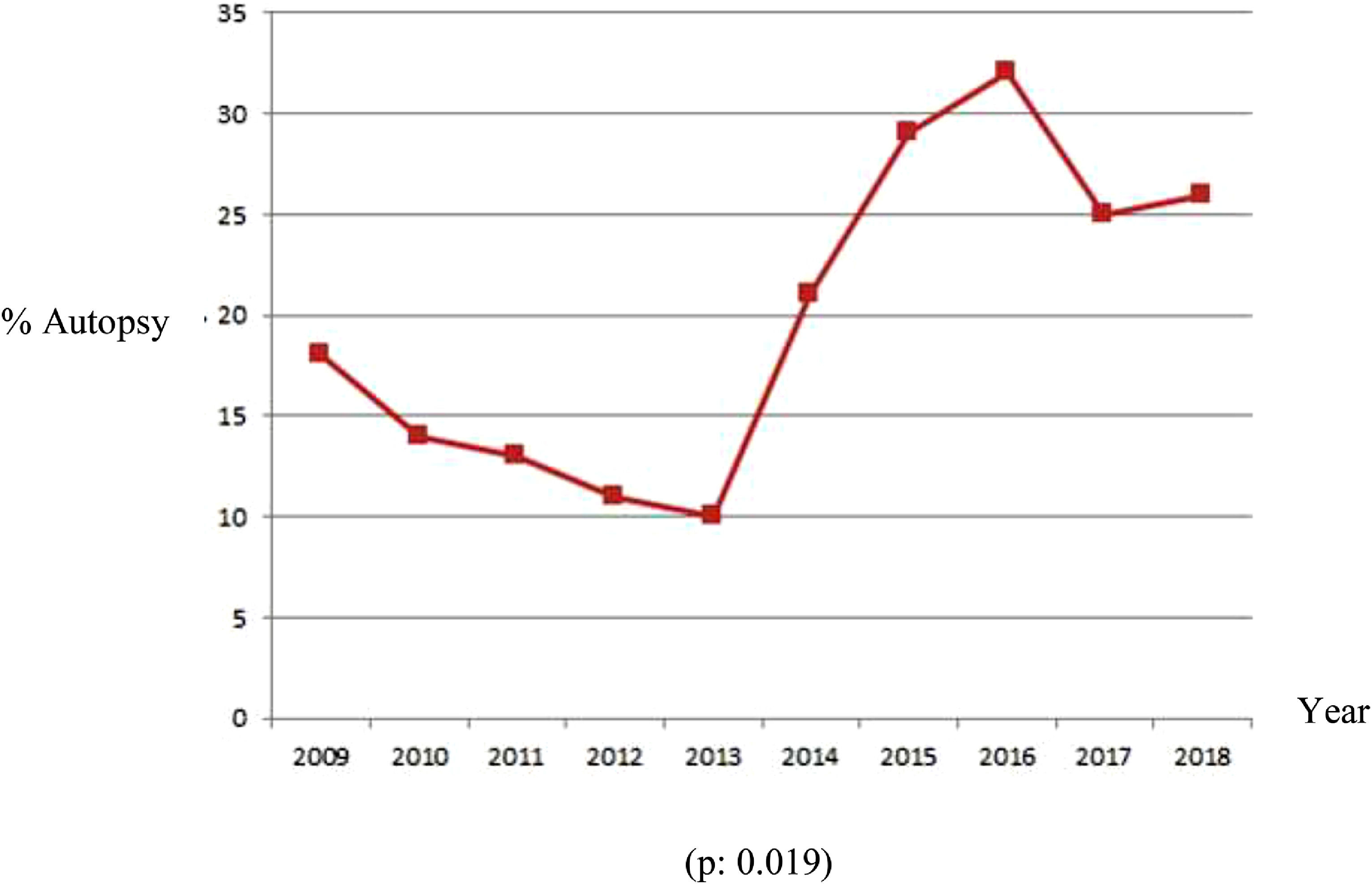
During the study period, there was a steady increase in autopsy rates, as shown in the graph below (Figure 1). The linear regression model showed a significant average increase of 1.87% per year.
DiscussionIn this study, the authors found an autopsy rate of 19.1% for neonates who died during a NICU stay at the study's facility over a 10-year period. The Level III NICU at our university-affiliated tertiary care hospital is a referral center for the Southern region of Brazil, a middle-income country, and our neonatal mortality rate is approximately 7%. Autopsy rates vary across centers; a review by Heazel and Fenton showed perinatal autopsy rates of 5% in low-income countries compared to up to 60% in high-income countries. 15 The authors did not find any previous reports of neonatal autopsy rates in Brazil. Although the global literature suggests that neonatal autopsy rates are decreasing,17,18 the authors have seen an increase in the percentage of autopsies performed at our service in recent years, largely due to awareness-building outreach work by multidisciplinary teams and to greater clarification and acceptance by patients’ families. The medical and psychological team has shown the families the importance of an accurate diagnosis for genetic counseling and clarification of the condition that caused the death, and this work has led to the highest acceptance rate of the examination in recent years.
The most common clinical causes of death in the study's sample were genetic/congenital malformations (accounting for more than half of the cases) and prematurity—findings that have also been described in other centers.18
The present study's hospital is also a referral center for high-risk pregnancies, with preterm births corresponding to approximately 14% of deliveries per year, which may explain the high frequency of prematurity as a cause of death. In addition, 15% of preterm infants in the present study had a gestational age below 24 weeks.
It also bears stressing that the fetal medicine and medical genetics services are a reference for the whole Southern region of Brazil, which again contributes to the high rate of neonates with congenital malformations born at this hospital. The fetal medicine service is staffed by a multidisciplinary team composed of specialist physicians (neonatologist, palliative care neonatologist, medical geneticist, interventional obstetrician, neurosurgeon, pediatric surgeon, pediatric cardiologist), a psychologist, and a bioethicist. From this perspective, the neonatal autopsy is particularly important, as postmortem examination may contribute to the diagnosis of genetic conditions and malformations not previously identified during life.2,3 With a view to clarifying postmortem diagnoses and providing closure to parents and other family members, the pathologist who performs the autopsies schedules an appointment with the child's parents and explains the report and the autopsy findings in detail.
Sample collection for DNA extraction during the autopsy ensures material availability for molecular analysis in the future. The specific examinations for each case were only carried out according to the results of the autopsy, always in combination with the family members. In 5 of the autopsies performed during the study period (6.9%), the findings contributed to subsequent genetic counseling of the infants’ families. In this context, parents were followed at the hospital's medical genetics service for future preconception counseling and received the results of karyotyping and DNA extraction.
The authors found a high rate of agreement between clinical and postmortem examination in the main diagnoses; however, several additional findings were disclosed by autopsy, occasionally revealing conditions that proved fatal. Previous studies have shown varying rates of concordance.17-20 In the present study's sample, there was an agreement between the anatomic and clinical diagnoses in 48 cases (65.8%), while additional findings were revealed at autopsy in 25 (34.2%). In 80% of cases, the autopsy findings were Class I and II. In 7 autopsies (9.6%), the results revealed findings that could have changed management in the ICU, potentially resulting in cure or prolonged survival (Class IA). Among these, cardiac malformations (present in 4 of the 7 patients) stand out, as they are associated with significant morbidity and mortality, but early diagnosis often allows adequate management. In Brazil, cardiovascular defects are responsible for 39% of deaths in children with congenital malformations under one year of age.21 Based on the autopsy reports of these patients, management protocols were modified at out NICU; the authors currently recommend echocardiography and a formal fetal cardiology assessment for all patients followed by the fetal medicine service who have major malformations and echocardiography for those with altered cardiovascular examinations or abnormal heart test results. Overall, additional findings have been reported in 22 to 81% of autopsies,9 with 3 to 5% of these having prognostic implications.21,12,13 Costa et al. 17 found that 66% of autopsies revealed additional information. They also found that, in 5.7% of cases, the autopsy findings would likely have had prognostic implications if they had been known before death (Class IA), and in 9.4%, findings were relevant for further genetic counseling (Class 1B). Despite advances in diagnostic technology, postmortem examination by autopsy continues to provide important clinical data, especially in neonatal intensive care settings. The authors’ findings are consistent with those reported elsewhere in the literature and provide further evidence of this importance.
Some limitations of this study are worth noting. Cases referred for autopsy were possibly those in where there was an identified need for further investigation of the cause of death. The authors still lack an established routine of performing an autopsy in all patients who have a fatal outcome, whether because of limited acceptance of parents or because the reasons for death were clear. Another limitation is the small number of autopsies performed at the service during the study period, which may limit the generalizability of the authors’ findings.
Postmortem MRI was not done in any of the cases reported here. However, seeking to assess whether autopsy findings were potentially detectable by postmortem MRI, de Sévaux et al.3 found additional findings obtained by autopsy in 48% of the cases evaluated. Of these, 56.3% probably would not have been detected by postmortem MRI. Therefore, even if such imaging had been obtained, it likely would not have been able to provide the wealth of detail afforded by anatomic examination. Thus, it is important to stress the role of autopsy in the NICU environment as well as to corroborate the hypothesis that it will not be completely replaced by postmortem MRI.
The present study's results corroborate those of previous studies and highlight the important role of autopsy after neonatal death. Despite a high level of agreement between clinical diagnosis and anatomic findings, autopsy provides important data regarding the cause of death, providing relevant, potentially practice-changing additional clinical information to neonatologists and informing future genetic counseling of parents and other family members. The unique accuracy of an autopsy to determine the causes of neonatal death is an essential element of good clinical practice and should be part of any systematic approach to neonatal intensive care.