To investigate the association between postpartum depression and the occurrence of exclusive breastfeeding.
MethodThis is a cross-sectional study conducted in the states of the Northeast region, during the vaccination campaign in 2010. The sample consisted of 2583 mother–child pairs, with children aged from 15 days to 3 months. The Edinburgh Postnatal Depression Scale was used to screen for postpartum depression. The outcome was lack of exclusive breastfeeding, defined as the occurrence of this practice in the 24h preceding the interview. Postpartum depression was the explanatory variable of interest and the covariates were: socioeconomic and demographic conditions; maternal health care; prenatal, delivery, and postnatal care; and the child's biological factors. Multivariate logistic regression analysis was conducted to control for possible confounding factors.
ResultsExclusive breastfeeding was observed in 50.8% of the infants and 11.8% of women had symptoms of postpartum depression. In the multivariate logistic regression analysis, a higher chance of exclusive breastfeeding absence was found among mothers with symptoms of postpartum depression (OR=1.67; p<0.001), among younger subjects (OR=1.89; p<0.001), those who reported receiving benefits from the Bolsa Família Program (OR=1.25; p=0.016), and those started antenatal care later during pregnancy (OR=2.14; p=0.032).
ConclusionsPostpartum depression contributed to reducing the practice of exclusive breastfeeding. Therefore, this disorder should be included in the prenatal and early postpartum support guidelines for breastfeeding, especially in low socioeconomic status women.
Verificar a associação entre a depressão pós-parto e a ocorrência do aleitamento materno exclusivo.
MétodoEstudo de corte transversal realizado nos estados da região Nordeste, durante a campanha de vacinação de 2010. A amostra consistiu de 2583 binômios mães-crianças com idade entre 15 dias e 3 meses. Utilizou-se a Escala de Depressão Pós-Parto de Edimburgo para rastrear a depressão pós-parto. O desfecho consistiu da ausência de aleitamento materno exclusivo nas 24 horas que antecederam a entrevista. A depressão pós-parto foi variável explanatória de interesse e as covariáveis foram: as condições socioeconômicas e demográficas, assistência pré-natal, ao parto e pós-natal, e fatores da criança. Realizou-se análise de regressão logística multivariada com o objetivo de controlar possíveis fatores de confusão.
ResultadosA amamentação exclusiva foi observada em 50,8% das crianças e 11,8% das mulheres apresentaram sintomatologia indicativa de depressão pós-parto. Na análise de regressão logística multivariada foi verificada uma maior chance de ausência do aleitamento materno exclusivo entre as mães com sintomas de depressão pós-parto (OR=1,67; p<0,001).
ConclusõesA depressão pós-parto contribuiu para redução da prática do aleitamento materno exclusivo. Assim sendo, esse transtorno deveria ser incluído nas orientações de suporte desde o pré-natal e nos primeiros meses pós-parto, especialmente, em mulheres de baixo nível socioeconômico.
The benefits of breastfeeding for maternal and child health are well-established in the scientific literature. Considering its importance, the World Health Organization (WHO) recommends the practice of exclusive maternal breastfeeding during the first six months of life, and after this period, the introduction of adequate and healthy complementary feeding together with the maintenance of breastfeeding for up to two years or more.1 Despite the well-known advantages of exclusive breastfeeding (EBF), Brazil still lags behind in complying with this recommendation. In recent years, there has been an increase in the prevalence of breastfeeding; however, the early termination of EBF can still be considered a major public health problem.2
Several factors have been attributed to early EBF interruption, such as socioeconomic and cultural conditions, those related to age, maternal schooling, family income, early introduction of artificial nipples, and care factors, such as the number of prenatal consultations, hospital postpartum practice, rooming-in in the maternity ward, basic health care follow-up, and others related to the conditions of birth and health of infants and the social support network.3
Recent studies have suggested an association between postpartum depression symptoms (PPD) with the early interruption of EBF4 and with breastfeeding (BF).5,6 PPD is a mood disorder that affects women within 4–6 weeks of delivery, reaching its maximum intensity in the first six months, which may be prolonged until the end of the first postpartum year.7 There is a hypothesis that depressed mothers are less confident about their ability to breastfeed and therefore would be less willing to continue breastfeeding when compared to those without depressive symptoms.4,8
There is no consensus on the association between PPD and duration of breastfeeding, since some studies have not found an association between these two factors,9,10 while others report that mothers with depressive symptoms are more vulnerable to early interruption of BF, including EBF, as they could have greater difficulties and dissatisfaction with this practice.4,8,11,12
In the Brazilian context, the prevalence of postpartum depression is above the average world rate and close to that of countries with a similar socioeconomic status, ranging from 7.2% to 39.4%.13,14 Therefore, considering the need to investigate the association between PPD and early termination of EBF, this study aims to verify the association between maternal postpartum depression and the practice of EBF in infants younger than 3 months.
MethodsStudy site and populationThis study uses data from the survey “Evaluation of prenatal, birth care and care of infants under one year old in the Legal Amazon and the Northeast regions, Brazil, 2010”.13 The present was a cross-sectional study carried out in June 12, 2010, during the child multi-vaccination campaign in nine states in the Northeast region and eight in the Legal Amazon region, in Brazil. The original study had as a target population mothers and children under 1 year, from the priority municipalities according to the Infant Mortality Reduction Plan.
The inclusion criteria of the original study were: child aged less than 1 year, living in the same municipality of the vaccination unit where the study was performed, no twins or adopted children. If the mother had two children under 1 year of age, the youngest child was chosen for the study, aiming to minimize bias in the mother's recall. For the present study, data from the Northeast region were used and mothers with children under 15 days were excluded aiming to avoid confounding the symptoms of PPD and the phenomenon known as “maternity blues” or “baby blues”, a condition characterized by symptoms such as emotional lability and feelings of sadness and anxiety, often observed in the first two weeks postpartum.14,15
Sample size and sampling processSample size calculation for the original study13 considered an expected prevalence of 22% for “some complication during birth (self-reported),” according to data from the 2006/2007 National Demographic and Health Survey.16 The sample plans were created based on information provided by the State Health Secretariats, on: (A) number of vaccination units in each municipality; (B) estimate of the number of children under 1 year who would be vaccinated at each unit based on the 2009 vaccination campaign worksheets; (C) size of the resident population under 1 year in each municipality.
In the capitals, two-stage conglomerate sampling with drawing of lots was used. The sample size was multiplied by the design correction factor (deff=1.5), which determined a sample of 750 mother and child pairs for each state. In the first stage, the vaccination units were randomly selected by drawing lots, and for the second stage, a lot fraction was defined for each unit, in order to carry out the systematic selection in the vaccination line. The sample, for all the capitals, was self-weighted, i.e., all were equally likely to be selected.13
In relation to the countryside of each state, all municipalities that participated in the research were considered as strata, and the set of municipalities in the countryside of each state comprised a sampling domain. In each municipality, one to six vaccination units were randomly selected by drawing lots, depending on the population of the municipality and the number of existing vaccination units.13
The systematic selection of the interviewed mother–child pair sought to obey the interval determined in the sampling process, according to the lot fraction for each vaccination unit. However, in an attempt to adjust the interval to the day's demand, this interval was reduced at the beginning of the fieldwork, when a low demand for vaccination was observed on that day, considering the inclusion and selection criteria.13
The sample for the present study consisted of 2583 mother–child pairs, with children aged between 15 days and 3 months of age. A total of 324 cases did not answer the questionnaire, and thus, the sample for the PPD variable resulted in 2259 mother–child pairs.
Study variablesThe explanatory variable was PPD and the covariates were: maternal socioeconomic and demographic conditions [age, schooling, Bolsa Família Program (BFP) beneficiary (Federal government's program to guarantee food and access to education and health for low-income families)], prenatal care (prenatal care assistance, number of consultations, prenatal care start trimester, having received information on BF, breast examination during prenatal care, and prenatal evaluation by the pregnant woman); birth care (type of maternity, type of delivery, presence of companion during delivery); postnatal care (breastfeeding in the first hour of life, presence of companion and rooming-in after delivery, seeking health care service in the first week postpartum, home visits by a family health professional after childbirth, current home visits by a community health agent or another family health professional); child-related variables (gender, birth weight, hospitalization in the first month of life after discharge from the maternity ward). The outcome variable was the absence of the EBF practice in the 24h prior to the interview.
Maternal breastfeeding definitionTo classify the breastfeeding profile as EBF, the World Health Organization's definition was used: the child must receive only breast milk, and no other liquids or solids, except for drops or liquid preparations containing vitamins, oral rehydration solutions, mineral supplements, or medications.1 To classify the child as in EBF, a positive response was considered when breast milk consumption occurred in the last 24h prior to the interview and negative for all other inquired foods.
Postpartum depression assessmentThe Edinburgh Postnatal Depression Scale (EPDS), a tool developed by Cox et al.,17 which has been translated and validated in several countries, including Brazil, was used to screen for postpartum depression.18,19 The EPDS contains questions about how the woman has been feeling for the last seven days. This scale can be self-applied and has ten items, with scores ranging from 0 to 3, according to the presence and intensity of the depressive symptom. In this study the scale was applied through an interview. A score ≥12 was used as the cutoff point for PPD, considering the good predictive value shown by validation studies and the possibility of better comparability with the studies carried out in the region that also used the same cutoff.20,21
Data collectionA form with closed and pre-coded questions about sociodemographic characteristics of the family; prenatal, birth, and postpartum care; symptoms of postpartum depression; and data on the child's health was used for data collection. The interview was carried out after the vaccination, in a room reserved for this purpose at the Basic Health Unit (Unidade Básica de Saúde [UBS]), only with the mothers and children who met the inclusion criteria. In the capitals, home visits were made when children under 3 months were not accompanied by the mother on the day of the vaccination campaign, in order to apply the EPDS to the mother, thereby performing an active search for possible cases of PPD.
Analysis planThe database analysis used SPSS, version 13.0 (SPSS for Windows, Version 13.0, USA). The associations between the variables were expressed through odds ratios (OR) and their respective 95% confidence intervals (95% CI), defining as the reference category the one that theoretically had a higher chance of the mother to be exclusively breastfeeding. Pearson's chi-squared test was used to evaluate the association between categorical variables, with statistical significance set at p<0.05.
Aiming to control for possible confounding factors, a multivariate logistic regression analysis was performed, and variables with p<0.20 in the bivariate analysis were selected for this analysis. For the OR adjustments, the hierarchical input approach of variables in blocks was used, in three levels of determination, using the Enter method. Only the variables that showed a p-value <0.20 remained in the models. Model 1 included socioeconomic and maternal demographic variables. Model 2 included those related to prenatal care, while Model 3 included those related to postnatal care, the child's variables, and the occurrence of PPD.
Ethical aspectsThe project was approved by the Research Ethics Committee of the National School of Public Health (ENSP/FIOCRUZ), in compliance with Resolution No. 196/96 of the National Health Council, with research protocol No. 56/10 and CAAE No. 0058.0.031.000-10.
Before the questionnaire was applied, the mothers who agreed to participate in this study signed the informed consent form and were made aware that the confidentiality and privacy of the information provided was assured. When symptoms suggestive of postpartum depression were identified, the mothers were referred to the Psychosocial Care Centers (Centros de Atendimento Psicossocial [CAPS]).
ResultsThe sample consisted of 2583 mother–child pairs, with children aged between 15 days and 3 months of life, of whom 2259 (87.5%) answered the questionnaire about maternal mental health. Among these, approximately 12% had PPD. Most mothers were aged between 20 and 29 years (55.3%) and had eight or more years of education (71.9%). 41.5% of the children were in the age group between 31 and 60 days, 5.9% had low birth weight, and 50.8% had a diet consisting exclusively of breast milk. Regarding health care, it was observed that 98.7% received prenatal care, 80.9% of which was in the public health care network. Of these, 78.8% started to received health care in the first trimester of the pregnancy and 77.2% had at least six prenatal consultations.
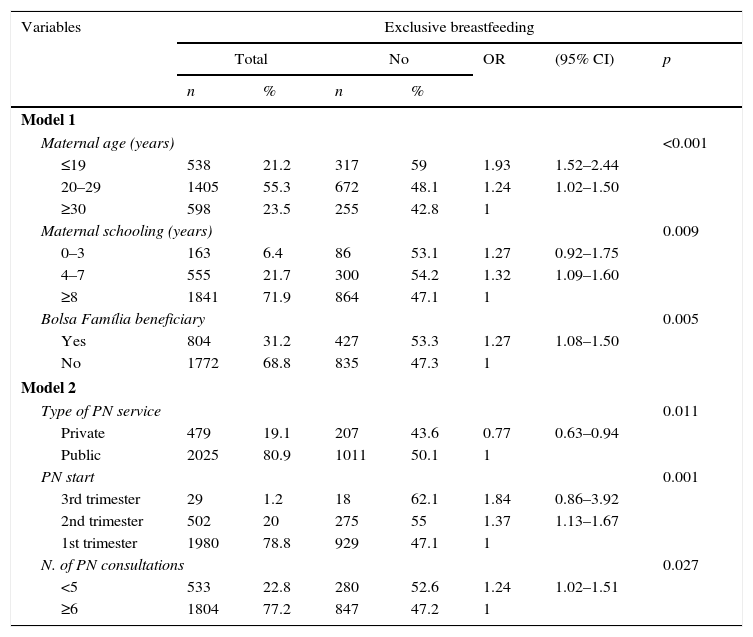
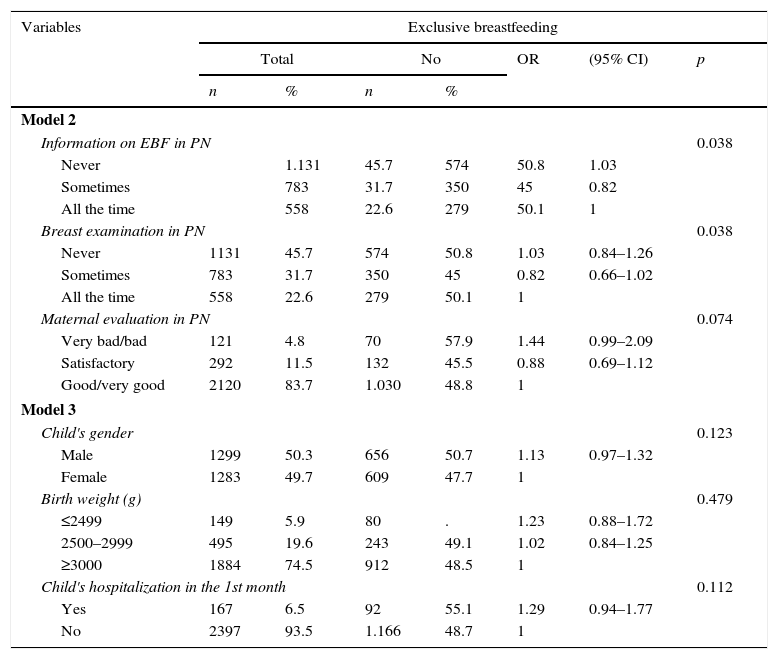
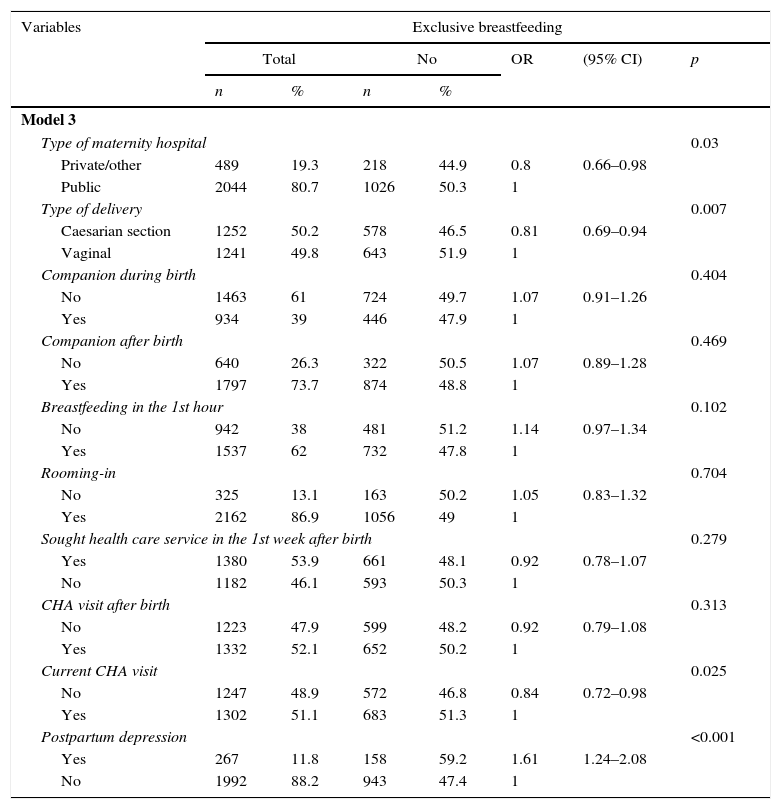
Tables 1–3 show the bivariate analyses; variables with p<0.20 were selected for the logistic regression analysis.
Socioeconomic status and prenatal care in relation to the absence of exclusive breastfeeding in children under 3 months. Northeastern Region, 2010.
| Variables | Exclusive breastfeeding | ||||||
|---|---|---|---|---|---|---|---|
| Total | No | OR | (95% CI) | p | |||
| n | % | n | % | ||||
| Model 1 | |||||||
| Maternal age (years) | <0.001 | ||||||
| ≤19 | 538 | 21.2 | 317 | 59 | 1.93 | 1.52–2.44 | |
| 20–29 | 1405 | 55.3 | 672 | 48.1 | 1.24 | 1.02–1.50 | |
| ≥30 | 598 | 23.5 | 255 | 42.8 | 1 | ||
| Maternal schooling (years) | 0.009 | ||||||
| 0–3 | 163 | 6.4 | 86 | 53.1 | 1.27 | 0.92–1.75 | |
| 4–7 | 555 | 21.7 | 300 | 54.2 | 1.32 | 1.09–1.60 | |
| ≥8 | 1841 | 71.9 | 864 | 47.1 | 1 | ||
| Bolsa Família beneficiary | 0.005 | ||||||
| Yes | 804 | 31.2 | 427 | 53.3 | 1.27 | 1.08–1.50 | |
| No | 1772 | 68.8 | 835 | 47.3 | 1 | ||
| Model 2 | |||||||
| Type of PN service | 0.011 | ||||||
| Private | 479 | 19.1 | 207 | 43.6 | 0.77 | 0.63–0.94 | |
| Public | 2025 | 80.9 | 1011 | 50.1 | 1 | ||
| PN start | 0.001 | ||||||
| 3rd trimester | 29 | 1.2 | 18 | 62.1 | 1.84 | 0.86–3.92 | |
| 2nd trimester | 502 | 20 | 275 | 55 | 1.37 | 1.13–1.67 | |
| 1st trimester | 1980 | 78.8 | 929 | 47.1 | 1 | ||
| N. of PN consultations | 0.027 | ||||||
| <5 | 533 | 22.8 | 280 | 52.6 | 1.24 | 1.02–1.51 | |
| ≥6 | 1804 | 77.2 | 847 | 47.2 | 1 | ||
OR, odds ratio; CI, confidence interval; PN, prenatal.
Prenatal care and child variables in relation to the absence of exclusive breastfeeding in children under 3 months. Northeast region, 2010.
| Variables | Exclusive breastfeeding | ||||||
|---|---|---|---|---|---|---|---|
| Total | No | OR | (95% CI) | p | |||
| n | % | n | % | ||||
| Model 2 | |||||||
| Information on EBF in PN | 0.038 | ||||||
| Never | 1.131 | 45.7 | 574 | 50.8 | 1.03 | ||
| Sometimes | 783 | 31.7 | 350 | 45 | 0.82 | ||
| All the time | 558 | 22.6 | 279 | 50.1 | 1 | ||
| Breast examination in PN | 0.038 | ||||||
| Never | 1131 | 45.7 | 574 | 50.8 | 1.03 | 0.84–1.26 | |
| Sometimes | 783 | 31.7 | 350 | 45 | 0.82 | 0.66–1.02 | |
| All the time | 558 | 22.6 | 279 | 50.1 | 1 | ||
| Maternal evaluation in PN | 0.074 | ||||||
| Very bad/bad | 121 | 4.8 | 70 | 57.9 | 1.44 | 0.99–2.09 | |
| Satisfactory | 292 | 11.5 | 132 | 45.5 | 0.88 | 0.69–1.12 | |
| Good/very good | 2120 | 83.7 | 1.030 | 48.8 | 1 | ||
| Model 3 | |||||||
| Child's gender | 0.123 | ||||||
| Male | 1299 | 50.3 | 656 | 50.7 | 1.13 | 0.97–1.32 | |
| Female | 1283 | 49.7 | 609 | 47.7 | 1 | ||
| Birth weight (g) | 0.479 | ||||||
| ≤2499 | 149 | 5.9 | 80 | . | 1.23 | 0.88–1.72 | |
| 2500–2999 | 495 | 19.6 | 243 | 49.1 | 1.02 | 0.84–1.25 | |
| ≥3000 | 1884 | 74.5 | 912 | 48.5 | 1 | ||
| Child's hospitalization in the 1st month | 0.112 | ||||||
| Yes | 167 | 6.5 | 92 | 55.1 | 1.29 | 0.94–1.77 | |
| No | 2397 | 93.5 | 1.166 | 48.7 | 1 | ||
OR, odds ratio; CI, confidence interval; EBF, exclusive breastfeeding; PN, prenatal.
Birth, postnatal care, and maternal mental health in relation to the absence of exclusive breastfeeding in children under 3 months. Northeast region, 2010.
| Variables | Exclusive breastfeeding | ||||||
|---|---|---|---|---|---|---|---|
| Total | No | OR | (95% CI) | p | |||
| n | % | n | % | ||||
| Model 3 | |||||||
| Type of maternity hospital | 0.03 | ||||||
| Private/other | 489 | 19.3 | 218 | 44.9 | 0.8 | 0.66–0.98 | |
| Public | 2044 | 80.7 | 1026 | 50.3 | 1 | ||
| Type of delivery | 0.007 | ||||||
| Caesarian section | 1252 | 50.2 | 578 | 46.5 | 0.81 | 0.69–0.94 | |
| Vaginal | 1241 | 49.8 | 643 | 51.9 | 1 | ||
| Companion during birth | 0.404 | ||||||
| No | 1463 | 61 | 724 | 49.7 | 1.07 | 0.91–1.26 | |
| Yes | 934 | 39 | 446 | 47.9 | 1 | ||
| Companion after birth | 0.469 | ||||||
| No | 640 | 26.3 | 322 | 50.5 | 1.07 | 0.89–1.28 | |
| Yes | 1797 | 73.7 | 874 | 48.8 | 1 | ||
| Breastfeeding in the 1st hour | 0.102 | ||||||
| No | 942 | 38 | 481 | 51.2 | 1.14 | 0.97–1.34 | |
| Yes | 1537 | 62 | 732 | 47.8 | 1 | ||
| Rooming-in | 0.704 | ||||||
| No | 325 | 13.1 | 163 | 50.2 | 1.05 | 0.83–1.32 | |
| Yes | 2162 | 86.9 | 1056 | 49 | 1 | ||
| Sought health care service in the 1st week after birth | 0.279 | ||||||
| Yes | 1380 | 53.9 | 661 | 48.1 | 0.92 | 0.78–1.07 | |
| No | 1182 | 46.1 | 593 | 50.3 | 1 | ||
| CHA visit after birth | 0.313 | ||||||
| No | 1223 | 47.9 | 599 | 48.2 | 0.92 | 0.79–1.08 | |
| Yes | 1332 | 52.1 | 652 | 50.2 | 1 | ||
| Current CHA visit | 0.025 | ||||||
| No | 1247 | 48.9 | 572 | 46.8 | 0.84 | 0.72–0.98 | |
| Yes | 1302 | 51.1 | 683 | 51.3 | 1 | ||
| Postpartum depression | <0.001 | ||||||
| Yes | 267 | 11.8 | 158 | 59.2 | 1.61 | 1.24–2.08 | |
| No | 1992 | 88.2 | 943 | 47.4 | 1 | ||
OR, odds ratio; CI, confidence interval; CHA, community health agent.
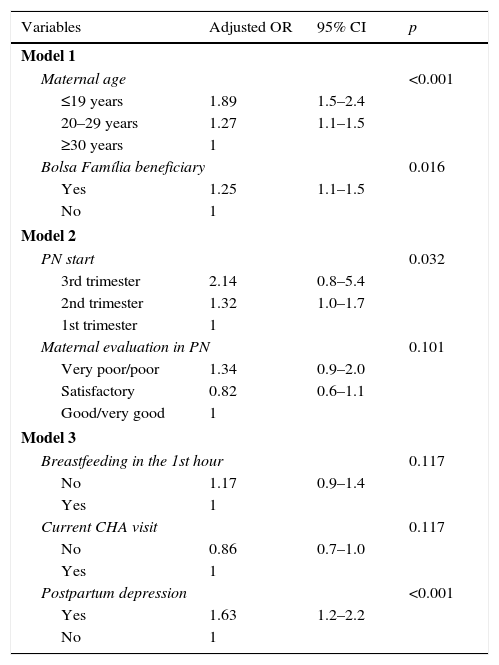
Table 4 shows, after adjustment in the multivariate logistic regression analysis, a significantly higher chance of absence of EBF among children whose mothers had PPD (OR=1.63), were adolescents (OR=1.89), started prenatal care later during pregnancy (OR=2.14), or were BFP beneficiaries (OR=1.25).
Logistic regression of factors associated with the absence of exclusive breastfeeding in children under 3 months. Northeast region, 2010.
| Variables | Adjusted OR | 95% CI | p |
|---|---|---|---|
| Model 1 | |||
| Maternal age | <0.001 | ||
| ≤19 years | 1.89 | 1.5–2.4 | |
| 20–29 years | 1.27 | 1.1–1.5 | |
| ≥30 years | 1 | ||
| Bolsa Família beneficiary | 0.016 | ||
| Yes | 1.25 | 1.1–1.5 | |
| No | 1 | ||
| Model 2 | |||
| PN start | 0.032 | ||
| 3rd trimester | 2.14 | 0.8–5.4 | |
| 2nd trimester | 1.32 | 1.0–1.7 | |
| 1st trimester | 1 | ||
| Maternal evaluation in PN | 0.101 | ||
| Very poor/poor | 1.34 | 0.9–2.0 | |
| Satisfactory | 0.82 | 0.6–1.1 | |
| Good/very good | 1 | ||
| Model 3 | |||
| Breastfeeding in the 1st hour | 0.117 | ||
| No | 1.17 | 0.9–1.4 | |
| Yes | 1 | ||
| Current CHA visit | 0.117 | ||
| No | 0.86 | 0.7–1.0 | |
| Yes | 1 | ||
| Postpartum depression | <0.001 | ||
| Yes | 1.63 | 1.2–2.2 | |
| No | 1 | ||
OR, odds ratio; CI, confidence interval; PN, prenatal; CHA, community health agent.
Model 1: adjusted for maternal schooling.
Model 2: adjusted for the variables of Model 1 and the variables: prenatal service type, number of prenatal consultations, prenatal breast examination, and information on breastfeeding in the prenatal care.
Model 3: adjusted for the variables in Models 1 and 2 and the variables: gender of the child, hospitalization in the first month, type of delivery, and type of maternity hospital.
This study showed a prevalence of approximately 12% for PPD in mothers with children aged between 15 days and 3 months. Studies carried out in Brazil on this subject have shown very wide-ranging estimates, varying from 7.2% to 39.4%.14,22 This disparity in results can be attributed to the use of different methodological strategies, such as different study designs and different tools for screening and diagnosis, as well as the timing of the postpartum interview.6,11
A study carried out in Recife (PE), with a sample of 276 postpartum women between the 4th and 6th weeks postpartum, which used the EPDS as a screening tool and also considered as cutoff a score ≥12, found a prevalence of PPD of 10.5% among the assessed women.20 Conversely, Andrade Gomes et al.,23 using the EPDS with a score ≥13, found a higher prevalence in a study performed in maternity hospitals in Fortaleza (CE), where 24.2% of the assessed women had symptoms of PPD. These divergent estimates may be due, among other factors, to the different moments at which the surveys were carried out, the different cut-off points of the screening tool, and the method used for sample selection.
The present study showed that mothers with symptoms suggestive of PPD had a 1.63-fold higher chance of EBF interruption. This result indicates the importance of investigating maternal mental health as one of the possible determinants of early weaning.
The association between PPD and the practice of EBF is not yet well-established in the literature; however, this issue has been the subject of several scientific studies, since one of the consequences of PPD may be the reduction of EBF duration.6 Despite this observation, there is no consensus yet, as some studies indicate that mothers with depressive symptoms are more likely to abandon the practice of EBF,4,8 whereas others have not found an association between these factors.9,10
The result found in this study is in agreement with that obtained by Hasselmann et al.8 when evaluating the association between PPD and early interruption of EBF in the first two months of life, using EPDS score ≥12 as the screening method. These authors found that children of mothers with depressive symptoms were at a higher risk for EBF interruption, both in the first month (RR=1.46, p=0.06) and in the second month of follow-up (RR=1.21; p=0.03), even after these variables were controlled for potential confounding factors.
Similar results to those of the abovementioned studies were obtained by Gaffney et al.5 using EPDS score >10 as the cutoff point for PPD indication. These authors verified that mothers with depressive symptoms had a higher chance of lower-intensity breastfeeding, calculated by the mean proportion of breast milk, and the early addition of cereals to the diet of infants younger than 2 months. One of the justifications for this finding is that breastfeeding self-efficacy, which is demonstrated by maternal confidence in breastfeeding, tends to be affected by depressive symptoms.4 In the literature, there is a higher probability that women with high self-esteem in the postpartum period will remain longer in EBF.24
This study also observed a greater trend of EBF discontinuation in younger women. Adolescents (≤19 years) had a 1.89-fold higher chance of early interruption of EBF, while women aged between 20 and 29 years showed a 1.27-fold higher chance when compared to those aged ≥30 years. Several studies have confirmed these results, as they suggest that maternal age may be associated with the interruption of EBF, so that the younger the mother, the greater the risk for early weaning.3,25 This finding can be explained by the greater experience and knowledge about breastfeeding that older women have, by the possible insecurity of adolescents regarding their ability to breastfeed,26 and also because they are more prone to feeding errors, which may be related to the lower socioeconomic status or repetitive eating habits, which in many cases are inadequate.27
Studies have associated higher per capita income as a protective factor for EBF.28,29 In the present study, it was observed that families who were BFP beneficiaries, i.e., those with lower per capita family income, were more likely to interrupt EBF early (OR=1.25, p=0.016), showing the importance of investigating low socioeconomic status as a risk factor for early weaning.
In contrast to the results found, Mascarenhas et al.29 observed that children from very poor families showed no increased risk of early EBF interruption, which could be justified by the absolute lack of income to acquire a breast milk substitute. According to Carrascoza et al.,30 the analysis of the influence of this factor may show a dichotomous character, since the families of high socioeconomic level have, in most cases, higher education level, which would be a facilitator to the understanding of breastfeeding benefits, while at the same time having greater access to breastmilk substitutes. Conversely, families with low socioeconomic status usually have lower levels of education, which would negatively influence the practice of EBF.
In addition to the socioeconomic and demographic factors, there is also the influence healthcare-related issues, specifically in the prenatal period. This study showed a greater chance of early interruption of EBF in mothers who started prenatal care later during the pregnancy. This result was in agreement with that observed by Oliveira et al.,2 in a study carried out in a city in the semi-arid region of Paraíba, where a longer median duration of exclusive/predominant breastfeeding was found among women who started prenatal care earlier during pregnancy.
Studies have shown that information offered during prenatal care contribute to the decision of women to practice BF as well as to its duration, probably because prenatal care is a favorable moment for educational interventions aimed at guiding and encouraging the practice of breastfeeding.2,31
The present study was carried out in strategic regions for policies aimed to reduce health inequities, especially for the maternal–child group, by providing a multi-vaccination campaign, which made it possible to assess a representative sample of the population, in addition to prioritizing relevant aspects of health care and nutrition of infants. Considering that this is a cross-sectional study, some aspects, due to their complexity, could be obtained with greater reliability in a prospective follow-up.
The findings of this study reinforce that the genesis of early EBF interruption can be characterized as multifactorial, as there is a complex inter-relationship between the economic, cultural, health care, and social support dimensions involved in the explanatory model of EBF duration. Considering the analyzed aspects, among the several associated factors, the authors emphasize the importance of conducting studies that investigate the influence of mental health in postpartum women, due to the consequences on the mother–infant interaction23 and on the practice of EBF, in order to support actions that will promote integral attention to maternal and child health.
FundingBrazilian Ministry of Health, Secretariat of Science, Technology, and Strategic Inputs, Department of Science and Technology.
Conflicts of interestThe authors declare no conflicts of interest.
The authors would like to thank the Ministry of Health for funding the research and the database availability, the participating women, the fieldwork team, and the research coordinators. They also thank the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) for the research productivity grant to Marilia Lima and Pedro Lira.
Please cite this article as: Silva CS, Lima MC, Sequeira-de-Andrade LA, Oliveira JS, Monteiro JS, Lima NM, et al. Association between postpartum depression and the practice of exclusive breastfeeding in the first three months of life. J Pediatr (Rio J). 2017;93:356–64.
Study conducted at Universidade Federal de Pernambuco, Pós-graduação em Saúde da Criança e do Adolescente, Recife, PE, Brazil.