Evaluate the association between breastfeeding, exclusive breastfeeding at six months and the introduction of complementary feeding during the pre-pandemic and the COVID-19 pandemic periods.
MethodsCohort study conducted with puerperal women and their newborns in the immediate postpartum period at a reference maternity hospital in Southern Brazil between 2018-2020. The COVID-19 pandemic period and the need to work outside the home during restricted circulation were the factors of exposure. The outcome evaluated was the weaning in the first six months (breastfeeding and exclusive breastfeeding) and the introduction of complementary feeding before the sixth month of life.
Results547 puerperal women and their newborns were included. During the COVID-19 pandemic, there was a higher risk to weaning of exclusive breastfeeding up until six months (RR 1.16; 95%CI 1.03-1.31) and introducing complementary feeding early (RR 1.40; 95%CI 1.01-1.96). The need to work outside the home during the COVID-19 pandemic increased the risk of not breastfeeding exclusively at the sixth month (RR 1.27; 95%CI 1.08-1.49).
ConclusionsThe difficulties of the pandemic did reflect negatively on breastfeeding and complementary feeding practices. The pandemic was a risk factor for the early weaning of exclusive breastfeeding and the introduction of complementary feeding. However, not having to work outside the home during the pandemic period was a protective factor for exclusive breastfeeding at six months.
The early initiation of breastfeeding and its exclusivity contribute to significant health benefits for both the mother and baby. 1 In Brazil, preliminary data from the National Survey of Food and Child Nutrition (ENANI 2019) revealed that the prevalence of exclusive breastfeeding for six months was 45.7%, and continued breastfeeding for 12 and 24 months was 53.1% and 60.9%, respectively.2 On February 27th of the year 2020, Brazil was affected by the Coronavirus-19 disease (COVID-19). From the beginning of the pandemic until September 2020, the state of Rio Grande do Sul registered 158,033 confirmed cases of the disease and 3767 deaths. During this period, no treatment protocol had yet been established, the process of vaccination of the Brazilian population had not started and restricted circulation was recommended.3 Many questions and concerns were raised about COVID-19 and its impact on the maternal and child health group and there was a lack of evidence of how much this situation has influenced the prevalence of breastfeeding, exclusive breastfeeding and the introduction of complementary feeding. The World Health Organization (WHO) recommends that mothers be encouraged to initiate or continue with breastfeeding, as the benefits outweigh the transmission risks.4 Up until today, there is no evidence that Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) transmission occurs through breastmilk.5,6
In response to the need to develop effective COVID-19 prevention strategies like social distancing, the use of face masks, and hand and surface hygiene aimed to minimize the spread of the virus, a reorganization in the health services was also observed and adapted. In many cases, telephone consultations were implemented in Primary Care Attention that included prenatal and postnatal care. Although necessary, those measures can directly affect the initiation and continuation process of exclusive breastfeeding, as well as the introduction of complementary feeding. The data found in current literature is divergent, as some studies report challenges in continuing breastfeeding during the COVID-19 pandemic due to the lack of professional support. Other issues include physical problems such as latch difficulty, tiredness, and pain.7–9 In contrast, other studies indicate that the pandemic scenario may have facilitated breastfeeding and child nutrition practices due to the increased time spent at home that could be dedicated to the child.9–11
In Brazil, the emergence of COVID-19 has made social inequality even more evident, bringing back discussions about food and nutrition security. In the last two years, the occurrence of hunger has increased by 27.6% per year, placing the country back on the world hunger map. Since childhood food insecurity can generate growth and development deficits, as well as greater susceptibility to diseases and infections, the importance of continued breastfeeding up to two years or more is further reinforced.1,12
In this context, this study aims to evaluate breastfeeding and exclusive breastfeeding for the first six months and the introduction of complementary feeding during the pre-pandemic and the COVID-19 pandemic periods in a sample of women and their children from Southern Brazil.
MethodsThe Maternar study is a cohort study initiated in April 2018 and aimed to investigate the prenatal care and nutritional assistance received during pregnancy and its association with perinatal outcomes and breastfeeding.
The population is composed of puerperal women and their newborns admitted to the maternity ward of the Hospital de Clínicas de Porto Alegre (HCPA) for the monitoring of their childbirths and their immediate postpartum care. HCPA is a university hospital of national reference, certified and accredited by the Joint Commission International. Its Obstetric Center performs approximately 3500 childbirths per year, which mostly assists users of the Unified Health System (SUS) (96,4%) and is known for assisting in highly complex medical cases.
For inclusion criteria, the following was considered: ages greater than or equal to 19 years, the delivery of live births, or the delivery of dead fetus weighing more than 500 g and/or a gestational age greater than 20 weeks, as well as a residency in Rio Grande do Sul, Brazil. Postpartum women with psychological or mental impairment unable to communicate with the researcher and whose cognitive abilities were unfit to answer the survey were not included in the cohort study. For this analysis, mothers with breastfeeding restrictions (carriers of the human immunodeficiency virus HIV) were excluded, as well as neonatal and stillborn deaths.
Data were collected in two phases by trained researchers, based on two questionnaires pre-tested in a pilot study. The selection occurred by simple random sampling, using the daily list of hospitalized puerperas, and reviewing their electronic medical record. Subsequently, those who met the eligibility criteria were selected to participate in the interview from their hospital bed.
In the recruitment phase, which occurred during the check-in of the puerperal women and their newborns in the maternity ward, data regarding maternal sociodemographic, prenatal, delivery and childbirth characteristics were collected. The follow-up phase took place via phone calls 180 days after childbirth. At this time, the data collected was relevant to the mother's and baby's general health, breastfeeding practices, and the introduction of the complementary feeding process. Issues regarding the detection of contamination by the Sars-CoV-2 virus, the need of mothers to work outside of the home during social isolation, and routine changes during the COVID-19 pandemic were analyzed. A self-reported question about the diagnosis with a positive test for COVID-19 was included in the study questionnaire in March 2020.
The exposure factors evaluated were the COVID-19 pandemic period and the needing to work outside of the home during the time of restricted circulation to help control the number of infections in the city of Porto Alegre and in the State of Rio Grande do Sul. To define the pre-pandemic and COVID-19 pandemic groups, the baby's date of birth was used in order to consider the corrected age in cases of prematurity. The authors included in the COVID-19 pandemic period any mother and babies with six months old in the period from March 2020.
The evaluated outcome was the weaning in the first six months (of breastfeeding and exclusive breastfeeding) and the early introduction to complementary feeding. These were developed based on the WHO12 recommendations and the Ministry of Health of Brazil13 and were defined as follows: Breastfeeding: provision of breast milk during the first six months, regardless of the introduction of other foods or liquids; Exclusive Breastfeeding: offering only breast milk during the first six months and no other source of food or liquid; and Complementary Feeding: introducing complementary foods after six months of life.
Among the covariates evaluated, the maternal age was obtained using the date of birth registered in the mother´s electronic medical record (19 – 25; 26 – 34; ≥35 years); the educational attainment by years of schooling (≤ 8; 9 – 11; ≥ 12); family income was obtained in minimum wages through an answer card and later transformed into per capita and divided into tertiles; the number of residents in the household was identified through the interview with the mother, as well as her marital status (with partner/without a partner). Type of childbirth was found in the electronic medical record, such as the newborns’ birth weight. The gestational age at the time of childbirth was calculated based on the first ultrasound (recorded in the prenatal booklet) if it took place before the 20th week of gestation. When performed after the 20th week of gestation, the last menstrual period date registered was used. Birth weight for gestational age was assessed by Intergrowth-21st intrauterine growth curves, considering birth weight <10th percentile as small for gestational age and > 90th percentile as large for gestational age.
The research data was exported from REDCap®ฏ and analyzed in the IBM SPSS Statistics v.22 software package. The descriptive analysis was performed by calculating their frequency distribution (crude and relative) and their respective 95% confidence intervals. In the case of continuous variables, the mean and the standard deviation were calculated. The relationship between the sociodemographic and obstetric characteristics (comparing the pre-pandemic sample and the COVID-19 pandemic sample) was verified using Pearson's chi-squared test. Crude and adjusted Relative Risk (RR) with a progressive input of variables and their respective 95% confidence intervals (95%IC) were estimated by Poisson Regression with robust variance. The association was considered statistically significant when p < 0.05. Stratified analysis was performed, where the association between the exposure to work outside the home during the restriction of circulation among women in the COVID-19 pandemic period and the proposed outcomes were evaluated.
Participation in the study was voluntary by signing the informed consent form. The study followed the criteria of Resolution 466/2012 of the National Health Council, which was approved by the Institution's Ethics Committee (protocol n. 83872018.9.0000.5327).
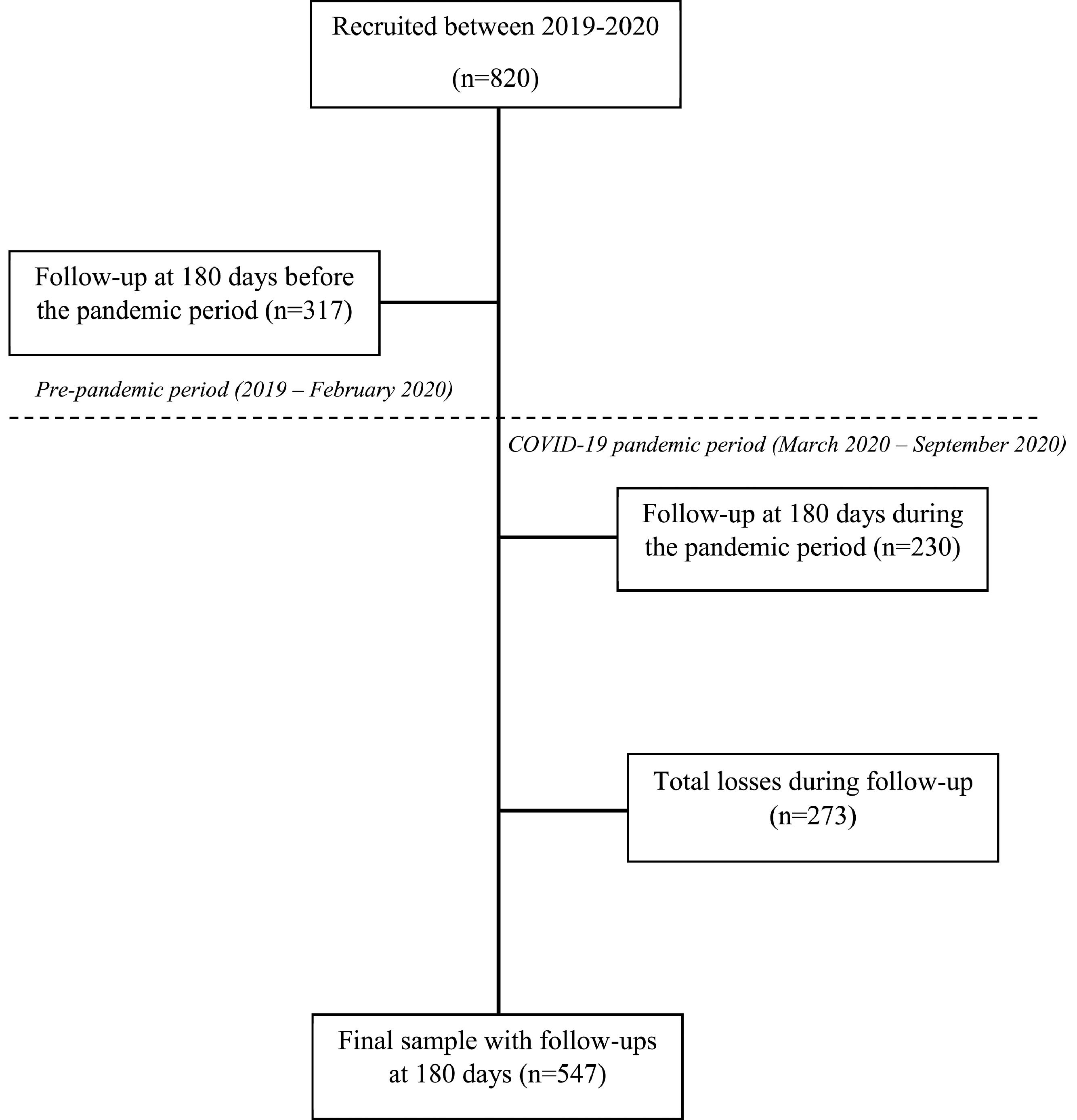
ResultsA total of 820 women and their newborns were recruited between January 2019 and February 2020. Out of these women, 547 (66.7%) women and their newborns are included in the follow-up phase of the study (Figure 1). The average age of the mothers that participated in the follow-up interview was 28.3 ± 6.3 years of age. There was a higher proportion of women with education attainment between nine and eleven years of schooling (63.1%). As far as neonatal characteristics, the vast majority of babies were born appropriate for gestational age (86.9%). Table 1 shows the sociodemographic, obstetric and neonatal characteristics among the women interviewed during the pre-pandemic and the COVID-19 pandemic periods. There were significant statistical differences observed between those periods and the type of delivery performed and birth weight for gestational age.
Sociodemographic, obstetric and neonatal characteristics among the women interviewed during the pre-pandemic and COVID-19 pandemic periods – Maternar Cohort Study, Rio Grande do Sul, Brazil, 2020 (n = 547).
| Characteristics | Period | p valuea | |||
|---|---|---|---|---|---|
| Total | Pre-pandemic COVID-19 (n = 317) | COVID-19 pandemic (n = 230) | |||
| n (%) | |||||
| Age (years) | |||||
| ≤ 24 | 190 (34.7) | 106 (33.4) | 84 (36.5) | 0.657 | |
| 25-34 | 238 (43.5) | 143 (45.1) | 95 (41.3) | ||
| ≥ 35 | 119 (21.8) | 68 (21.5) | 51 (22.2) | ||
| Education Attainment (years of schooling) | |||||
| ≤ 8 | 81 (14.8) | 46 (14.5) | 35 (15.2) | 0.471 | |
| 9 – 11 | 345 (63.1) | 195 (61.5) | 150 (65.2) | ||
| ≥ 12 | 121 (22.1) | 76 (24.0) | 45 (19.6) | ||
| Family income per capita | |||||
| Tertile 1 (R$ 82.5 – 412.5) | 217 (39.7) | 125 (39.4) | 92 (40.0) | 0.789 | |
| Tertile 2 (R$ 412.51 – 770.0) | 153 (28.0) | 86 (27.1) | 67 (29.1) | ||
| Tertile 3 (R$ 770.01 – 4125.0) | 177 (32.4) | 106 (33.4) | 71 (30.9) | ||
| Occupation | |||||
| Paid | 268 (49.0) | 164 (51.7) | 115 (50.0) | 0.689 | |
| Unpaid | 279 (51.0) | 153 (48.3) | 115 (50.0) | ||
| Marital Status | |||||
| With Partner | 453 (82.8) | 260 (82.0) | 193 (83.9) | 0.562 | |
| Without Partner | 94 (17.2) | 57 (18.0) | 37 (16.1) | ||
| Parity | |||||
| Primipara | 233 (42.6) | 138 (43.5) | 95 (41.3) | 0.603 | |
| Multipara | 314 (57.4) | 179 (56.5) | 135 (58.7) | ||
| Type of childbirth | |||||
| Normal | 333 (60.9) | 182 (57.4) | 151 (65.7) | 0.050 | |
| Cesarean | 214 (39.1) | 135 (42.6) | 79 (34.3) | ||
| Birth weight for gestational age | |||||
| Small for gestational age | 17 (3.1) | 11 (3.5) | 6 (2.6) | 0.027 | |
| Appropriate for gestational age | 472 (86.9) | 280 (89.5) | 192 (83.5) | ||
| Large for gestational age | 54 (9.9) | 22 (7.0) | 32 (13.9) | ||
| Breastfed within the first hour of life | |||||
| Yes | 252 (46.1) | 149 (47.0) | 103 (44.8) | 0.607 | |
| No | 295 (53.9) | 168 (53.0) | 127 (55.2) | ||
| Worked outside the home during the restricted circulation period | |||||
| Yes | - | - | 94 (40.9) | - | |
| No | - | - | 136 (59.1) | ||
The prevalence of breastfeeding and exclusive breastfeeding up to six months observed in the sample was 68.7% (376/547) and 34.2% (187/547), respectively. The introduction of complementary feeding at six months of age was identified in 79.7% (436/547). After adjusting for age, schooling, type of childbirth, birth weight for gestational age, and breastfeeding within one hour of birth, it was observed that the women interviewed during the COVID-19 pandemic period had a 16% (95%IC 1.03–1.31) highest risk to weaning of exclusive breastfeeding up until six months and a 40% (95%CI 1.01–1.96) highest risk of introducing complementary feeding before the sixth month, when compared to the women interviewed during the pre-pandemic period (Table 2).
Crude and adjusted relative risks by Poisson regression with robust variance between the outcomes (breastfeeding, exclusive breastfeeding and introduction of complementary feeding at six months) and the COVID-19 pandemic period – Maternar Cohort Study, Rio Grande do Sul, Brazil, 2020 (n = 547).
RR, relative risk; IC95%, 95% Confidence Interval; Model 1, crude; Model 2, adjusted for age and schooling; Model 3, adjusted for age, schooling, type of childbirth, birth weight for gestational age and breastfeeding within the first hour of life; Bold,p < 0.05.
Table 3 shows the crude and adjusted relative risk of the stratified analysis between the outcomes and the maternal exposure to working outside the home during the restricted circulation in the COVID-19 pandemic period. After adjustments made for: age, schooling, type of childbirth, birth weight for gestational age and breastfeeding within the first hour of life, it was identified that women who worked outside the home during the restricted circulation period had a 27% (95%CI 1.08–1.49) greater risk to weaning of exclusive breastfeeding up until six months when compared to those who were able to stay at home during the restricted circulation period.
Crude and adjusted relative risks by Poisson regression with robust variance between the outcomes (breastfeeding, exclusive breastfeeding and introduction of complementary feeding at six months) and the mother's needing to work outside the home during the COVID-19 pandemic period – Maternar Cohort Study, Rio Grande do Sul, Brazil, 2020 (n = 230)a.
RR, relative risk; 95%IC, 95% Confidence Interval; Model 1, crude; Model 2, adjusted for age and schooling; Model 3, adjusted for age, schooling, type of childbirth, birth weight for gestational age and breastfeeding within the first hour of life; Bold, p < 0.05.
Among the women interviewed during the pandemic period, twelve (5.2%) tested positive for Sars-CoV-2. The frequency for breastfeeding, exclusive breastfeeding until six months and complementary feeding after the sixth month for these women were 75% (9/12), 25% (3/12) and 83.3% (10/12), respectively (data not shown in table).
DiscussionThis study showed that during the pre-pandemic and COVID-19 pandemic periods, there was a greater risk of weaning exclusive breastfeeding during the first six months, as well as introducing complementary feeding before the sixth month of life. In addition, during the period of restricted circulation and greater social isolation in the pandemic, women that needed to work outside of the home were at greater risk of weaning exclusive breastfeeding during the first six months of life.
The authors did in fact, observe a 16% higher risk of not being exclusively breastfeeding at six months among the women interviewed in the pandemic period. Two different studies with Italian women participants found that the lockdown due to COVID-19 was a predictor for the decrease of exclusive breastfeeding duration.14,15 A case-control study showed that of the women in the control group, 86.39% practiced exclusive breastfeeding before COVID, while only 70.39% practiced exclusive breastfeeding during confinement.14 However, a study that took place in Belgium,10 found that 91% of breastfeeding women reported that the baby's diet did not change due to the pandemic. In this same study, among the few women that stopped breastfeeding during the pandemic, 88% reported that the interruption to breastfeeding was not caused by COVID-19.10
Regarding the introduction of complementary feeding before the sixth month of life, the authors observed a higher risk of occurrence among the interviewed women during the COVID-19 pandemic. Similar results were observed in a case study carried out in Northeastern Italy,14 which results in point to a 20% higher probability of introducing complementary feeding before the sixth month among the women in the COVID-19 group. Several factors, such as psychological, emotional, and social, can contribute to the early initiation of complementary feeding.9 One study looked at complementary feeding practices during the COVID-19 outbreak in Indonesia and determined that in the pandemic context, maternal knowledge about complementary feeding plays an important role in its adequate practice.16
A sensibility analysis was performed exclusively with the women interviewed during the COVID-19 pandemic and stratified by the needing to work outside the home during the period of restricted circulation. It was observed that women that needed to work outside the home during the pandemic were at a higher risk of weaning exclusive breastfeeding before the sixth month of life. The authors believe that because leaving the house during the period of restricted circulation became less necessary; this may have favored the correct breastfeeding practice due to the increased maternal time available to the child. Corroborating the hypothesis, a Belgian study with pregnant women and lactating women reported that among the women interviewed who were breastfeeding during the COVID-19 pandemic, 91% declared that there was not an evident change in the feeding of their baby since the beginning of the pandemic. Among 9% of the women who reported changes in infant feeding, in 82% of cases, the reported change was related to an increase in the breastfeeding frequency in comparison to the period prior to the pandemic. The authors also describe that one of the main maternal reasons for this increase in breastfeeding frequency was that staying at home with the baby allowed breastfeeding and the desire to protect their children against COVID-19 with breastmilk.10 One study performed in the United Kingdom investigated the intervention of the COVID-19 pandemic in the breastfeeding experience and showed that it could be positive due to the greater amount of time spent at home, undergoing less social pressure, and expecting fewer visits. But it can also be negative as far as a weaker support system, breastfeeding safety concerns, and social isolation.17
In addition to socioeconomic issues, emotional and psychological aspects can interfere with the practice and duration of breastfeeding.9,11 A narrative review concluded that the COVID-19 pandemic impacted both positively and negatively the breastfeeding practice. This finding seems to be associated with individual characteristics of the aspect of maternal life.9 Among the main reasons for the negative influence of the pandemic are the increased responsibilities with the children at home and the lack of family, emotional and professional support, which seem to have led to an increase in the experience of anxiety and stress-related to breastfeeding.9 Evidence about the mental health of infants during the COVID-19 pandemic is still scarce, a fact that makes it difficult to assess the impact of the COVID-19 pandemic on breastfeeding decisions and expectations and how it affects the psychological and emotional aspects of the mother.9 However, it is known that these women naturally are facing numerous changes in their lives that make them particularly vulnerable to mental disorders.9,11,18 A study carried out in five European countries identified high levels of depressive symptoms and generalized anxiety among pregnant and lactating women during the COVID-19 pandemic when compared to the prevalence described in the literature in the pre-pandemic period.18
Brazilian data related to the 2008 “II National Survey on the Prevalence of Breastfeeding”, which interviewed 3,776 women who were breastfeeding, showed that not being on maternity leave increased the chance of weaning by 23%.19 Although the 2019 ENANI saw an improvement in the exclusive breastfeeding rates for the first six months in Brazil, continued breastfeeding for up to 12 months is still under the standard rates seen in upper-middle, lower-middle and low-income countries,1,2 possibly due to the mother's return to work, without protective legislation for breastfeeding women. In a systematic review that analyzed the impact of maternity leave on breastfeeding duration in six continents, there was a positive association between maternity leave and the time spent breastfeeding. Returning to work was one of the main reasons for the early weaning.20 In Brazil, as provided by the Federal Constitution of 1988 - article seven, the period of maternity leave was extended for 120 days without adversely affecting their employment status or salary. However, that legislation only covers women who are inserted in the formal labor market and for those who do not surpass the 180 days proclaimed by the health system.21 Female participation in the work field is growing by the year, double shifts have become more and more frequent, and women's need to assume childcare responsibilities and their workload (inside and outside the home), have led to changes in how childcare and nutrition are handled.20,21
Among the limitations that can be registered, the authors acknowledge the fact of being a study carried out in a maternity hospital in Southern Brazil, that although of reference for the State of Rio Grande do Sul, the results must be interpreted within its possible external validity. In addition, the study was conducted with adult puerperal women and should be carefully analyzed in populations of different age groups. The present study was able to detect associations as small as RR = 1.39, considering p-value < 0.05 and power of 80% and the proportion of 31.2% of not being breastfed at six months. However, for the outcomes of exclusive breastfeeding and introduction of complementary feeding, statistically significant results were observed, demonstrating that this sample has the power to detect this association. The authors focused on the lack of studies related to the prevalence of breastfeeding and the introduction of complementary feeding during the COVID-19 pandemic. Therefore, it is believed that the results presented in this study contribute to a better understanding of the implications of the pandemic period on breastfeeding and complementary feeding rates.
The present study's data suggest that the evident difficulties imposed by the pandemic reflect negatively on the prevalence of breastfeeding and the introduction of complementary feeding. Not needing to work outside the home during the restricted circulation period was a protective factor against weaning, as it increased exclusive breastfeeding up to six months of life. Finally, it is fundamental to support women who breastfeed, as the practice is not merely the woman's responsibility. Society as a whole must provide the necessary conditions so that women working outside are able to breastfeed.
FundingThis study was sponsored by FIPE/HCPA (The Hospital de Clínicas de Porto Alegre Research and Events Incentive Fund), Brazil.
Hospital de Clínicas de Porto Alegre.