to determine the prevalence of mouth breathing and to associate the history of breastfeeding with breathing patterns in children.
Methodsthis was an observational study with 252 children of both genders, aged 30 to 48 months, who participated in a dental care program for mothers and newborns. As an instrument of data collection, a semi-structured questionnaire was administered to the children's mothers assessing the form and duration of breastfeeding and the oral habits of non-nutritive sucking. To determine the breathing patterns that the children had developed, medical history and clinical examination were used. Statistical analysis was conducted to examine the effects of exposure on the primary outcome (mouth breathing), and the prevalence ratio was calculated with a 95% confidence interval.
Resultsof the total sample, 43.1% of the children were mouth breathers, 48.4% had been breastfed exclusively until six months of age or more, and 27.4% had non-nutritive sucking habits. Statistically significant associations were found for bottle-feeding (p<0.001) and oral habits of non-nutritive sucking (p=0.009), with an increased likelihood of children exhibiting a predominantly oral breathing pattern. A statistically significant association was also observed between a longer duration of exclusive breastfeeding and a nasal breathing pattern presented by children.
Conclusionan increased duration of exclusive breastfeeding lowers the chances of children exhibiting a predominantly oral breathing pattern.
determinar a prevalência da respiração bucal e associar o histórico de amamentação com os padrões de respiração em crianças.
Métodoseste foi um estudo observacional com 252 crianças de ambos os sexos, com idades entre 30-48 meses, que participaram de um programa de assistência odontológica para mães e recém-nascidos. Como um instrumento de coleta de dados, foi entregue um questionário semiestruturado para as mães das crianças com perguntas sobre a forma e a duração da amamentação e os hábitos bucais de sucção não nutritiva. Para determinar os padrões de respiração desenvolvidos nas crianças, foram utilizados o histórico médico e o exame clínico. Foi realizada uma análise estatística para determinar os efeitos de exposição no principal resultado (respiração bucal), e o índice de prevalência foi calculado com um intervalo de confiança de 95%.
Resultadosdo total da amostra, 43,1% das crianças apresentaram respiração bucal, 48,4% foram amamentados exclusivamente até os seis meses de idade ou mais e 27,4% apresentaram hábitos de sucção não nutritiva. Foram encontradas associações estatisticamente significativas para uso de mamadeira (p<0,001) e hábitos bucais de sucção não nutritiva (p=0,009), com um aumento da probabilidade de as crianças apresentarem um padrão de respiração predominantemente bucal. Também foi observada uma associação estatisticamente significativa entre uma maior duração do aleitamento materno exclusivo e um padrão de respiração bucal apresentado pelas crianças.
Conclusãouma maior duração do aleitamento materno exclusivo diminui as chances de as crianças apresentarem um padrão de respiração predominantemente bucal.
Nutrition plays an important role in the growth and development of children. Maternal milk contains essential nutrients for newborns in the first months of life and has important functions in socioeconomic and psycho-emotional domains; exclusive breastfeeding is recommended for the first six months of life, and should be continued up to 2 years or more.1,2
The mechanics of breastfeeding in newborn are complex, and require the central nervous system to coordinate procedures for sucking, breathing, and swallowing.3,4 Children who are exclusively breastfed (EBF) during the first months of life exhibit a physiological suction pattern with more sucking movements, and are better coordinated when compared to those who are artificially bottle-fed; this phenomenon occurs because the orofacial muscles are exercised less in formula-fed infants, making those muscles more flaccid and hypotonic.5
The movements of milking executed by infants when breastfeeding favor a balance in the perioral muscle forces, and are key factors for the proper growth of the bones and the orofacial muscles, promoting the normal development of the stomatognathic system.6,7 When early weaning occurs, the child is unable to perform physiological movements and synchronized suction, and generally presents a tendency toward developing harmful habits, such as sucking a pacifier or the fingers, which can interfere in the process of nasal breathing.8
Breathing is a vital function of living organisms; in humans, breathing occurs physiologically through the nose.9 After birth, several factors can interfere with the regular breathing pattern; these factors can be conditional physical such as anatomical predispositions or can be present in the environment, in weather conditions, sleeping position, artificial feeding, and oral habits, including nonnutritive sucking.10
Mouth-breathing children are more predisposed to the development of facial changes, poor dental positioning, improper posture, and speech disorders.11 These conditions can further develop and trigger cardiorespiratory, endocrine, learning, sleep, and mood disorders that significantly and negatively affect overall health and quality of life.5,12–14 Studies have demonstrated that nose breathers have longer breastfeeding sessions, since the child keeps his/her lips sealed and lead up the tongue in a proper posture and as consequence establishes a correct pattern of breathing.15,16 Studies that accurately examine this relationship are lacking.
The present study aimed to determine the prevalence of mouth-breathing in children, associated with the duration and type of breastfeeding.
MethodsThis was an observational, cross-sectional, descriptive analytical study composed of children aged 30 to 48 months who participated in a maternal-infant dental care program called Preventive Program for Pregnant Women and Babies (PPGB). PPGB is an extension project of the dentistry course of the Universidade do Piauí in the Iniciativa Hospital Amigo da Criança (IHAC), in Maternidade Evangelina Rosa, Teresina, Piauí, Brazil.
From the total of medical records of 3,374 children assisted by the PPGB, 625 records initially filled the research criteria; from this data, the sample size was calculated. The inclusion criteria were as follows: complete primary dentition, normal birth weight, born at term, and good health. Children were excluded if they had tooth loss; had diseases such as dentofacial conditions; had large carious lesions that compromised occlusion; were syndromic; had neurological disorders or cleft lips or palates; or remained in the neonatal intensive care unit.
The present article is excerpted from a larger study about the implications of weaning on the oral motor system, with other variables. To calculate the sample size with the desired precision regarding the prevalence and to allow a confidence interval of 95%, a prevalence of 50% and an error of 4% were considered. The calculations were prepared using Epi-Info version 6.04b (CDC - Atlanta, Georgia, USA) in the StatCalc module, which uses the formula: s = [p (1-p)] * z2 / d2, where p is the prevalence in the population, z is the percentile of the standard normal distribution, and d is the maximum amplitude of the absolute value of the difference between the estimate and the population value, adjusted by a correction factor for finite populations. The result indicated that a sample of 252 children was required for the research.
Correspondence was sent to the parents of the identified children, inviting them to bring their children for a health evaluation, where they were informed of the study objectives. A semi-structured questionnaire was administered to the mothers of children, with open questions related to daily feeding habits and the use of bottle, and closed questions to characterize the following aspects of the population: gender, age, type and duration of breastfeeding, and presence of nutritive and non-nutritive oral sucking habits in the children. The data collection was conducted in the period from April of 2010 to June of 2011, by the researcher, previously trained and calibrated, aided by interns of the PPGB, who are students of dentistry of UFPI, insofar as children returned to the project.
The definitions of breastfeeding recommended by the World Health Organization (WHO) were used for the study.17 For this work, three of them were chosen: exclusive breastfeeding, breastfeeding, and bottle-feeding. Exclusive breastfeeding was defined as feeding in which the child receives breast milk directly from the breast or expressed milk, with no other liquid or solid food, except for vitamin drops. Breastfeeding was defined as a form of feeding where the child is fed human milk (directly from the breast or expressed) regardless of other foods; in bottle-feeding, the child ingests any kind of liquid or semisolid food from a bottle.
In the absence of a single clinical protocol for the diagnosis of mouth breathing, two methods were used. The first was a written history, as established by Abreu et al.,13 which advocates the following clinical manifestations as major signs: snoring, mouth open while sleeping, drool on the pillow, stuffy nose every day. The following are considered as minor signs: itchy nose; occasional congested nose; difficulty breathing at night or restless sleep; irritability or drowsiness during the day; difficulty or delayed food swallowing; episodes of throat infection, ear infection or sinusitis; and difficulty in school or grade repetition. The occurrence of two major signs or two minor signs in the patient's history is compatible with mouth breathing.
The second method used was established by observation and palpation of the mentalis muscle. The relationship of the upper and lower lips to the resting position of the tongue was evaluated, and breath analysis of the child was performed while he/she was in a more relaxed position, according to the method established by Moyers.18 The test was indicative of mouth breathing if the child showed a lack of lip seal.
With these two diagnostic methods, the child's breathing pattern type was determined; children who presented characteristics compatible with mouth breathing in both methods were considered as mouth breathers.
A pre-test questionnaire was administered to 20 mothers who did not participate in the study, in an attempt to make the necessary adjustments for a better understanding of the addressed factors. The legal guardians signed the consent form, according to the recommendations of Resolution 196/96 of the Ministry of Health and the Declaration of Helsinki. The study was approved by the Ethics in Research Committee of UFPI (Opinion No. CAAE 0039.0.045.000-10).
The data were processed and analyzed using Stata, version 11.0 (Stata Corporation - College Station, TX, USA). To assess the association between variables, the chi-squared test was used. The multivariate analysis included variables with p<0.20 in the bivariate analysis, using Poisson regression in order to verify the independent variables associated with the presence of oral breathing, controlled for possible confusion factors (adjusted prevalence ratios [PR]). The results were presented as PRs, and the 95% confidence interval and associations were verified by the Wald's test. The results with p<0.05 were considered statistically significant.
ResultsThe study population was composed of 139 male children (55.2%) and 113 female children (44.8%), aged 30 to 48 months, with a mean age of 39.3 (± 4.7) months and a mean birth weight of 3,860.1 (± 619.7) grams; 114 (45.2%) of the children were from families earning 2 to 3 Brazilian minimum wages. In relation to breastfeeding, 122 (48.4%) of the children were exclusively breastfed until 6 months of age or more, and 199 (79.0%) were breastfed until 24 months. The breathing pattern presented by the children, considering the sign test and the type of labial occlusion, were predominantly oral in 109 (43.1%) children and predominantly nasal in 143 (56.9%) children.
According to the history reported by the mothers, the following signs were the most frequent: sleeping with open mouths, 119 (47.2%) of cases; drooling on the pillow, 100 (39.7%) of cases; and snoring, 95 (37.7%) of cases. The most prevalent minor signs were delay of swallowing food in 78 (30.9%) of cases; difficulty breathing or nocturnal restless sleep in 74 (29.3%) of cases; and episodes of throat infection, otitis, or sinusitis in 62 (24.6%) of cases. The clinical examination demonstrated that 125 (49.6%) of the children lacked labial seal.
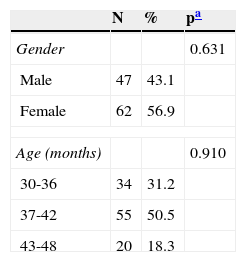
Table 1 presents the oral respiratory patterns (RP) by gender and age group. No association with respiratory pattern was observed for gender (p=0.631) or age (p=0.910).
Prevalence of a predominantly mouth breathing pattern according to sex and age (n=109).
| N | % | pa | |
|---|---|---|---|
| Gender | 0.631 | ||
| Male | 47 | 43.1 | |
| Female | 62 | 56.9 | |
| Age (months) | 0.910 | ||
| 30-36 | 34 | 31.2 | |
| 37-42 | 55 | 50.5 | |
| 43-48 | 20 | 18.3 | |
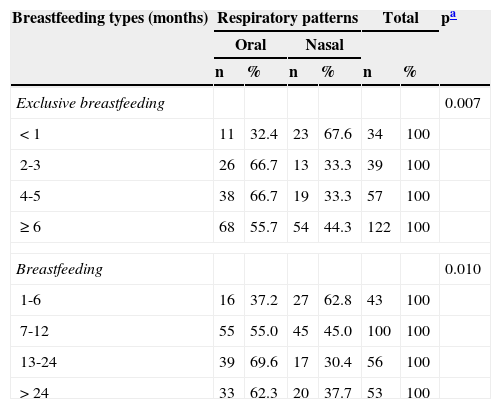
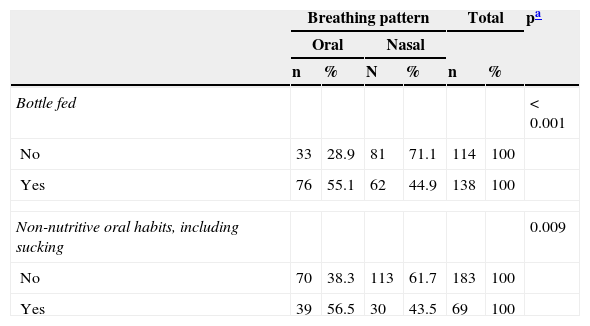
Tables 2 and 3 show that there was a statistically significant association between exclusive breastfeeding (p=0.007), breastfeeding (p=0.010), bottle feeding (p < 0.001), and non-nutritive sucking habits (p=0.009) with the children's type of respiratory pattern.
Association between respiratory patterns and breastfeeding type (n=252).
| Breastfeeding types (months) | Respiratory patterns | Total | pa | ||||
|---|---|---|---|---|---|---|---|
| Oral | Nasal | ||||||
| n | % | n | % | n | % | ||
| Exclusive breastfeeding | 0.007 | ||||||
| < 1 | 11 | 32.4 | 23 | 67.6 | 34 | 100 | |
| 2-3 | 26 | 66.7 | 13 | 33.3 | 39 | 100 | |
| 4-5 | 38 | 66.7 | 19 | 33.3 | 57 | 100 | |
| ≥ 6 | 68 | 55.7 | 54 | 44.3 | 122 | 100 | |
| Breastfeeding | 0.010 | ||||||
| 1-6 | 16 | 37.2 | 27 | 62.8 | 43 | 100 | |
| 7-12 | 55 | 55.0 | 45 | 45.0 | 100 | 100 | |
| 13-24 | 39 | 69.6 | 17 | 30.4 | 56 | 100 | |
| > 24 | 33 | 62.3 | 20 | 37.7 | 53 | 100 | |
Associations of respiratory patterns with bottle feeding and the presence of non-nutritive oral habits (n=252).
| Breathing pattern | Total | pa | |||||
|---|---|---|---|---|---|---|---|
| Oral | Nasal | ||||||
| n | % | N | % | n | % | ||
| Bottle fed | < 0.001 | ||||||
| No | 33 | 28.9 | 81 | 71.1 | 114 | 100 | |
| Yes | 76 | 55.1 | 62 | 44.9 | 138 | 100 | |
| Non-nutritive oral habits, including sucking | 0.009 | ||||||
| No | 70 | 38.3 | 113 | 61.7 | 183 | 100 | |
| Yes | 39 | 56.5 | 30 | 43.5 | 69 | 100 | |
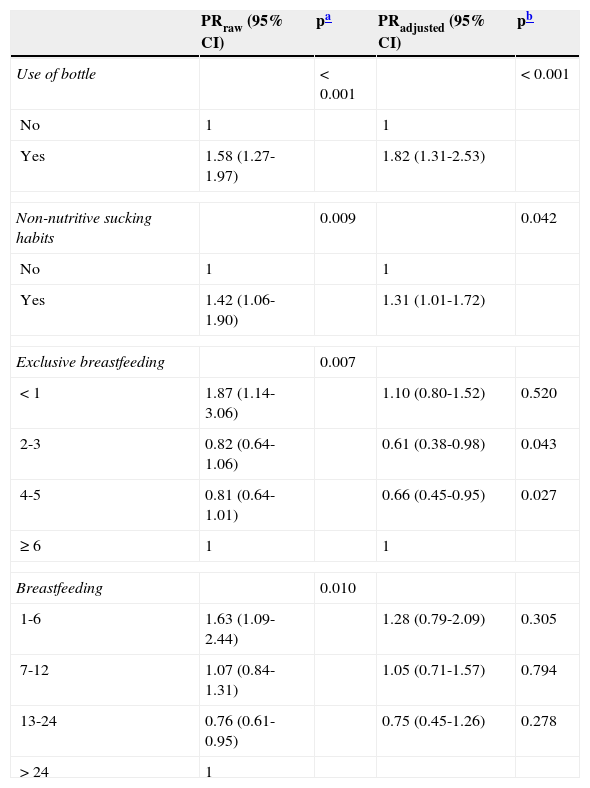
Table 4 presents the multivariate model using Poisson regression with robust variance for the independent factors associated with the predominant respiratory pattern, demonstrating that the use of bottle feeding (p=0.001), presence of non-nutritive sucking habits (p=0.048), and exclusive breastfeeding for 2 to 3 months (p=0.045) and from 4 to 5 months (p=0.043) were the only statistically significant independent factors in the model.
Crude and adjusted prevalence ratio for the factors associated to the raw respiratory pattern (n=252).
| PRraw (95% CI) | pa | PRadjusted (95% CI) | pb | |
|---|---|---|---|---|
| Use of bottle | < 0.001 | < 0.001 | ||
| No | 1 | 1 | ||
| Yes | 1.58 (1.27-1.97) | 1.82 (1.31-2.53) | ||
| Non-nutritive sucking habits | 0.009 | 0.042 | ||
| No | 1 | 1 | ||
| Yes | 1.42 (1.06-1.90) | 1.31 (1.01-1.72) | ||
| Exclusive breastfeeding | 0.007 | |||
| < 1 | 1.87 (1.14-3.06) | 1.10 (0.80-1.52) | 0.520 | |
| 2-3 | 0.82 (0.64-1.06) | 0.61 (0.38-0.98) | 0.043 | |
| 4-5 | 0.81 (0.64-1.01) | 0.66 (0.45-0.95) | 0.027 | |
| ≥ 6 | 1 | 1 | ||
| Breastfeeding | 0.010 | |||
| 1-6 | 1.63 (1.09-2.44) | 1.28 (0.79-2.09) | 0.305 | |
| 7-12 | 1.07 (0.84-1.31) | 1.05 (0.71-1.57) | 0.794 | |
| 13-24 | 0.76 (0.61-0.95) | 0.75 (0.45-1.26) | 0.278 | |
| > 24 | 1 | |||
PRraw, unadjusted variables at the bivariate analysis; PRadjusted, adjustment for other variables; 95% CI, 95% confidence interval.
The findings of this study provide important information about the relationship between breastfeeding and the breathing pattern of children. Studies examining this relationship and the prevalence of oral breathing during infancy are scare in the literature. Some researches have been conducted with school-aged children, but recall biases are almost always present; other studies have been conducted using convenience samples.7,12,19 Such samples may have been used primarily due to the technical difficulties associated with operational or commonly used methods for the diagnosis of mouth breathing, which are complex examinations conducted in tertiary care.7,16,20 The diagnosis of oral breathing is clinically performed through detailed anamnesis, since mothers typically do not report signs such as snoring, sleeping with the mouth open, and drooling on the pillow during routine visits.21
In this study, the interview protocol proposed by Abreu et al.13 was used in combination with the technique proposed by Moyers;18 these tests can be performed by professionals in various areas of primary health care. Following the early diagnosis of mouth breathing, it is important to refer the patient for interventional treatment, because mouth breathing has been associated with numerous adverse effects.13,15,20–22 Just under half of the children examined showed a predominantly oral breathing pattern, which is a high prevalence, but lower than that observed by other authors, including Abreu et al.,13 Felcal et al.,19 and Limeira et al.15 These studies were conducted with school-age children, whereas in the present study, the majority of the subjects were 3 years of age.
In the present work, statistically significant relationships were observed for the durations of exclusive breastfeeding and total breastfeeding with breathing patterns (Table 3). Nasal breathers exhibited a normal breathing pattern and were breastfed for a longer period than mouth breathing children, which was also observed in other studies.6,8,15,16 Children who were exclusively breastfed for over one month had a decreasing prevalence of developing a predominantly oral breathing pattern, and the possibility increased as the duration of exclusive breastfeeding increased. After the multivariate analysis, no association between breastfeeding and oral breathing was observed.
There appears to be a consensus in the literature regarding the time required for the establishment of breastfeeding and nasal breathing patterns. According to Santos-Neto,9 breastfeeding from the fifth month of life is a preventive factor against loss of lip closure, but this protection is only established in babies older than twelve months. However, the author did not specify whether the breastfeeding was exclusive or complete. Limeira et al.15 showed that protection occurred in children who were breastfed exclusively for the first six months of life and that the likelihood of developing a nasal breathing pattern increased as the breastfeeding duration increased, which was also observed in the present study.
Breastfeeding aids nasal breathing due to the physiology of this type of feeding, as it prevents air from entering through the mouth during feeding, forcing air to pass through the nose and stimulating all of the orofacial muscles.9,16 Moreover, the nutritional and immunological protection provided by human milk prevents or reduces the risk of respiratory infection,22 which can result in mouth breathing due to nasal obstruction.23
The WHO1 recommends exclusive breastfeeding until six months of age and complementary breastfeeding up to the age of 2 years or older. Children who are breastfed for a shorter period have been shown to present a higher risk for respiratory tract infections such as pneumonia, sinusitis, and otitis. The American Academy of Pediatrics24 reaffirmed the WHO recommendations for exclusive breastfeeding for the first six months of life and continued breastfeeding with the introduction of complementary foods for infants at least 12 months of age or older, as desired by the mother and child.
In the present study, bottle feeding was a statistically significant risk factor for respiratory patterns because more than half of the children with a predominantly oral breathing pattern used a bottle, even considering that all of the children were breastfed initially for different periods. Breastfeeding by bottle negatively interferes with orofacial development and leads to loss of the labial seal; moreover, it favors an improper position of the tongue and changes the shape of the jaw.6,9 When a child is bottle-fed, the facial muscles are exercised in a different manner than during breastfeeding, and the child's tongue must function as a milk dispenser, making it hypotonic and unable to stay in the correct position at rest. Studies on the sucking pattern of babies have observed other changes in the mechanics of sucking in bottle-fed children, such as changes in suction and a decrease in arrhythmic sucking movements.3,4
The absence of contact between the lips is undoubtedly a characteristic sign of mouth breathers. In this study, an analysis of the clinical manifestations in children classified as mouth breathers showed that sleeping with the mouth open was the most common sign, and was present in approximately half of the sample. The next most common signs were drooling on the pillow and snoring. The majority of children who had exclusively breastfed until six months of age showed a better seal of the lips, which was also observed in previous studies.6,15
The oral habit of non-nutritive sucking (pacifier or finger) has been shown to have direct and indirect harmful effects on some aspects of the child's health. When a baby frequently uses a pacifier, he/she will become a habitual mouth breather because of a compensatory facial and lingual muscle postural hypotonic4,5,9 which further interferes with normal breastfeeding mechanics.25–27 In the present study, it was evident that non-nutritive sucking habits were related to the respiratory pattern of infants, and those with these habits were more likely to develop an oral breathing pattern (p=0.009).
Currently, the majority of mothers believe in the benefits of breastfeeding, which has been confirmed by the observed increases in breastfeeding rates.28,29 However, bottles and pacifiers are still introduced often, even in children who are exclusively breastfed; this practice appears to increase the risk of early weaning,26 demonstrating that the use of the bottle is still an ingrained habit in Brazil and other countries.30
There is a high prevalence of a predominantly oral breathing pattern among children, and a significant association exists between exclusive breastfeeding and respiratory pattern. An increased duration of breastfeeding increases the likelihood of developing a normal breathing pattern. Motivational strategies and programs to increase the awareness of mothers should be implemented to make them more capable and to improve the safety of breastfeeding.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Lopes TS, Moura LF, Lima MC. Association between breastfeeding and breathing pattern in children: a sectional study. J Pediatr (Rio J). 2014;90:396–402.
Work linked to the Universidade Federal do Piauí, Teresina, PI, Brazil and Universidade Estadual de Campinas, Campinas, SP, Brazil.