To develop, validate, and test the reproducibility of a new test capable of assessing functional performance in children and adolescents (PAY test: Performance Activity in Youth).
Methodsparticipants without and with asthma were included in the development and validation phases, respectively. The PAY test includes five activities: transition from sitting to standing, walking 10 m, step climbing, shoulder extension and flexion, and star jumps. Participants underwent the Pediatric Glittre test (TGlittre-P test time), modified shuttle test (MST), and cardiopulmonary exercise test (CPET). Outcomes: PAY test and TGlittre-P test times, oxygen uptake (VO2peak), and distance walked in the MST.
Results8 healthy volunteers, aged 12 (7 - 15) years old were included in the development phase and 34 participants with asthma, aged 11 (7 -14) years old, in the validation phase. The PAY test elicited greater physiological responses (VO2peak 33.5 ± 6.9 mL/kg) than the TGlittre-P (VO2peak: 27.4 ± 9.0 mL/kg), but lower than the MST (VO2peak: 48.9 ± 14.2 mL/kg) and CPET (VO2peak: 42.0 ± 8.8 mL/kg), p < .05. Moderate correlation between the PAY test time and the TGlittre-P time (r = 0.70, p < .001) and distance walked in the MST (r = -0.72, p < .001). The PAY test time was longer in participants with asthma than in healthy participants (3.1 [3.0 - 3.3] min vs. 2.3 [2.1 – 2.4 min]), p < .001.; and the test was reproducible (ICC 0.78, CI 95% 0.55–0.90, p < .001).
ConclusionsThe PAY test is a valid and reproducible tool for assessing functional performance in children and adolescents with asthma.
A common finding in the most prevalent chronic respiratory disease in childhood, asthma, is the impairment of functional capacity.1,2 Among this population, the assessment of exercise capacity has become an essential outcome in quantifying functional impairment and responses to interventions. Therefore, field tests, such as the 6-minute walk test and shuttle tests (walking and running modalities), are widely used to evaluate exercise capacity in children and adolescents with chronic respiratory diseases.3–7 These tests can identify exercise capacity impairment; however, activities of daily living (ADL)8 is an important issue that is not covered by walking tests.
Some studies have reported the evaluation of ADL in different chronic conditions9–12 by using questionnaires or observation instruments. The Glittre-ADL test (TGlittre-P) has recently been validated for assessing ADL among the pediatric population with chronic respiratory disease.13 The advantage of the TGlittre-P is that it involves a broad range of functional activities. However, Almeida et al.14 evaluated children with cystic fibrosis using TGlittre-P and observed that the time to complete the test was similar to the normal predicted value. By contrast, Gianfrancesco et al.15 observed a difference in the time to perform the Glittre-ADL test between participants with asthma and the control group, but that difference can be shorter than the minimal detectable change.7 Thus, it seems that the Glittre-ADL test cannot discriminate between subjects with respiratory disease and healthy participants.
Considering that TGlittre-P was based on adult tasks, it is not representative of the ADL of children and adolescents, who usually expend more energy during their daily activities. Thus, there is no current test to assesses functional performance, beyond ADL, of children and adolescents with chronic respiratory conditions. This study aimed to develop a functional performance test (PAY: Performance Activity in Youth) for children and adolescents, to test its validity, reproducibility, and volunteer satisfaction with using the PAY test. The study was guided by the following question: Does the PAY test assess functional performance in children and adolescents?
MethodsThis is an observational study of the psychometric properties and physiological aspects of the cardiorespiratory system related to a new test to assess functional performance in children and adolescents aged 6 to 17 years old. Participants were enrolled in the study after their legal guardians had read, agreed to, and signed the informed consent and after the subject himself/herself signed the informed assent form. The study was approved by the institution's Ethics Committee (#2.236.325).
The study was conducted between April 2017 and December 2019 in the pulmonary rehabilitation laboratory at UNINOVE, in São Paulo, Brazil.
Healthy children and adolescents were selected for the first phase (they were employees’ relatives at the University), which focused on the study's development. Participants with asthma were selected for the second phase of the protocol.
The inclusion criteria for Phase 1 called for participants who were presumed healthy, with normal pulmonary function (> 80% of the predicted).16 The presence of acute or chronic diseases; the chronic use of medication; a respiratory infection in the last month; a body mass index (BMI) above the 85th percentile or below the 5th percentile in the age group of 6 to 12 years, or BMI greater than 30 kg/m2 or less than 18 kg/m2 for those over 13 years of age; premature birth; and those who were unable to perform the tests, either due to physical or cognitive limitations, were excluded from this phase. The inclusion criteria for Phase 2: participants with a clinical diagnosis of asthma (any severity according to GINA)10 and who were undergoing regular treatment (at least one visit to the physician every six months). The presence of asthma exacerbation in the last four weeks; an interruption or increase in the use of asthma intake medication in the last three months; premature birth; a body mass index (BMI) like Phase 1, and those who were unable to perform the assessments, either due to physical or cognitive limitations, were excluded from this phase.
Phase 1 consisted of applying the PAY test to healthy volunteers and the CPET in a random order on the same day, at least one hour apart. Phase 2 consisted of the validation and reproducibility of the PAY test on two different days: on Day 1, volunteers were given the MST and pediatric TGlittre-P tests at least one hour apart, in a random order; on Day 2 (48 h after Day 1), they performed the PAY test and CPET at least one hour apart, in a random order (Fig. 2 - Supplementary online file).
Lung functionSpirometry was performed using the ULTIMA CPX equipment (MedGraphics Corporation®, MN, USA). The technical procedure, acceptance criteria, and reproducibility were according to the recommendation.16 The FVC, FEV1, FEV1/FVC, and FEF25–75% were recorded and expressed as percentage of the predicted value.16
The PAY testThe PAY test's development process started by investigating which activities children and adolescents with asthma find difficult to perform. These task choices were based on a quality-of-life questionnaire (Pediatric Asthma Quality of Life Questionnaire - PAQLQ), which was previously administered by the present research group and answered by a cohort of participants with asthma (data not published). At the end of this questionnaire, the participant was asked to identify three activities that they were limited in performing, considering their chronic disease. Among the 145 questionnaires returned, the most noted difficult activities were jumping star (or jumping jacks), stepping, running, walking, putting an object on a shelf, jumping rope, kicking a ball, throwing a ball into a basket, throwing a ball above the head, and cycling.
All these tasks were performed (for 4 min each) by healthy volunteers, while oxygen consumption (VO2), heart rate (HR), and minute ventilation (VE) were recorded. Then, the authors identified which ones should be included in the final version of the test (data not shown), because the authors knew that all those 10 activities would be too long to be included in a test. The criteria used to select the tasks for inclusion in the PAY test were: (i) tasks that involved the use of the upper and lower limbs, (ii) tasks with higher metabolic demand, and (iii) tasks that could make the protocol feasible. In the end, five of 10 tasks were included in the PAY test (described above).
The PAY test is administered in a 10-meter-long corridor. The participant is assigned two different tasks to perform at each end of the corridor. Between each task, the participant walks 10 m. The participant begins in a seated position and then follows this sequence (Fig. 2 - Supplementary online file):
- i.
Move from being seated on a chair to standing five consecutive times (the count is done when standing). Then, walk 10 m.
- ii.
Climb a single 25-cm step five consecutive times (the count is done when the right foot is on the step). Then, walk back 10 m.
- iii.
Lifting a dumbbell above the head (maximal shoulder flexion) five consecutive times (the count is done when the arms are up). Then, walk 10 m. The dumbbells’ weight is varied according to the participant's age: 1 kg for those under 10 years old, 2 kg for those 11–13, and 3 kg for those 14–18 (based on a pilot study not published and considering weights of activities of daily living).
- iv.
Perform a star jump (or jumping jacks) five consecutive times (the count is done when the arms are up). Then, walk back 10 m.
The completion of all these activities is considered one lap. The participant immediately starts the next lap and repeats the cycle twice more (three laps in total). The number of laps was chosen to ensure enough time to observe participants’ physiological responses during the test. There were no standardized phrases, however, the number of tasks and laps in the PAY test was counted aloud by the person administering the test. Participant is asked to complete each task as quickly as possible and to walk, not run, between the ends of the hallway. Participant is allowed to rest during the test if necessary; however, the timer does not stop, and participants are encouraged to return to the activity as soon as they can, or to stop the test due to fatigue or breathlessness. The professional stopped the test if the participant's SpO2 fell to < 82%.13
The HR and SpO2 (Nonin PalmSAT Model 2500) were evaluated continuously. Modified Borg lower limb fatigue and modified Borg dyspnea were evaluated at the beginning and end of the test. Two PAY tests were performed on the same day (30 mins apart). All participants underwent the test with continuous measures of gas exchange (VO2000; MedGraphics Corporation®, St. Paul, MN, USA).
Modified shuttle test (MST)The MST was performed in a 10-m-long corridor according to the description.17 The volunteer can walk/run during the test. The test finished when the participant was unable to reach the extremities two consecutive times according to the audio if he/she needed to stop because of fatigue or breathlessness, or if the SpO2 dropped below 82%.18 HR and SpO2 were continuously evaluated. Modified Borg lower limb fatigue, and modified Borg dyspnea were evaluated at the beginning and at the end of the test. The test was performed twice in the same day (30-min apart). Distance walked at MST in meters and predicted value19 were the outcomes. All participants performed MST tests connected to a system for gas exchange analyses (VO2000; MedGraphics Corporation®, St. Paul, USA).
Pediatric glittre test - TGlittre-PThe adapted version of the Glittre test for the pediatric population was applied as previously described.13 The test consists of a volunteer carrying a backpack for 5 laps around a specific circuit.13 HR and SpO2 were continuously evaluated. Modified Borg lower limb fatigue, and modified Borg dyspnea were evaluated at the beginning and at the end of the test. The test was performed twice on the same day (30-min apart). All participants performed the TGlittre-P connected to a system for gas exchange analyses (VO2000; MedGraphics Corporation®, St. Paul, USA).
Cardiopulmonary exercise test (CPET)CPET was performed on an exercise treadmill (Millenium Classic CI®, Inbramed/ Inbrasport, Brazil) with a ramp protocol. For children aged 6 to 12 years, the Half-Bruce protocol was used, which has load increments every 1.5 min.21 Participants wear a face mask connected to a system composed of a gas analysis module and a computerized metabolic system (MGC, CPX System. Medical Graphics Corporation, USA), which measures gas exchange variables, breath-to-breath. Electrocardiographic tracing, HR20 and SpO2 were continuously recorded. Modified Borg lower limb fatigue, and modified Borg dyspnea were evaluated at the beginning and at the end of the test.
QuestionnairesAsthma control was assessed using the Asthma control questionnaire (ACT or C-ACT, depending on the subject's age).22,23 Asthma was considered controlled when the score was over 20, partially controlled when the score was between 16 and 19, and uncontrolled when the score was ≤ 15.
After performing the protocols, participants reported the degree of difficulty in performing each test by a Likert scale. There were four questions: (i) satisfaction with performing the test, (ii) dyspnea and (iii) lower limb fatigue during the test, and (iv) time taken to perform the test. Each answerer ranged from 0 to 4, with higher values indicating more positive responses. The total score is from 0 to 16 points is the outcome.
OutcomesThe PAY test time, the TGlittre-P time, distance walked at MST19, the workload at CPET, peak oxygen consumption (VO2peak), peak minute ventilation (VEpeak), heart rate (absolute and percentage of the predicted value based on equation = 208 − (0.7 × age))20 and total score of satisfaction questionnaire.
Statistical analysisThe sample size of Phase 2 was calculated based on a moderate correlation between PAY test time and TGlittre-P time. A sample of 29 participants was necessary for a correlation of 0.6 between the TGlittre-P time and PAY test time, with p = .5 and 80% power.
The normality of the studied variables was analyzed using the Shapiro–Wilk test. The parametric data were presented as mean (SD), and non-parametric data as median (IQR 25–75%).
For Phase 1, the Wilcoxon test was used to compare the VO2peak, VEpeak, and HR between the PAY test and CPET in healthy participants. For Phase 2, validity, physiological responses (HR, VO2peak, VEpeak) of the PAY test were compared to those of the TGlittre-P, MST, and CPET by repeated ANOVA with Bonferroni post hoc. Additionally, the distances walked at MST, TGlittre-P time, and CPET workload were correlated with the PAY test time. The discriminative validity was assessed by comparing the PAY test time of Phase 1 (healthy participants) with the PAY test time of Phase 2 (participants with asthma). For reproducibility, low reliability was indicated by an intraclass correlation coefficient (ICC) absolute agreement of less than 0.50; moderate reliability was considered between 0.51 and 0.75, and strong/excellent reliability was indicated by values of 0.76 or above.24 The Bland–Altman plot was used to analyze reproducibility and agreement between the PAY tests’-times. The satisfaction questionnaire scores relating to the PAY test, MST, and TGlittre-P were compared using the Wilcoxon test.
A P-value less than 0.05 was considered statistically significant. SPSS version 22 was used for the data analysis.
ResultsFifty-two children and adolescents were eligible to participate in this study: 10 healthy participants and 42 participants with asthma. Ten participants with asthma were excluded: three because of a lack of understanding regarding how to execute the test, and seven who developed an acute infection prior to the study beginning.
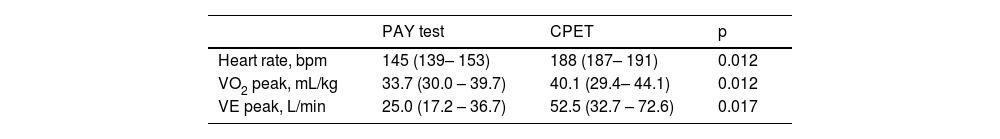
Phase 1Eight participants were classified as having a normal pulmonary function (Table 1). They finished the PAY test without difficulties. The outcomes of the PAY test and CPET are shown in Table 2. Except for the VO2peak, the participants had a statistically significant lower heart rate and minute ventilation during the PAY test compared to the CPET (p < .04).
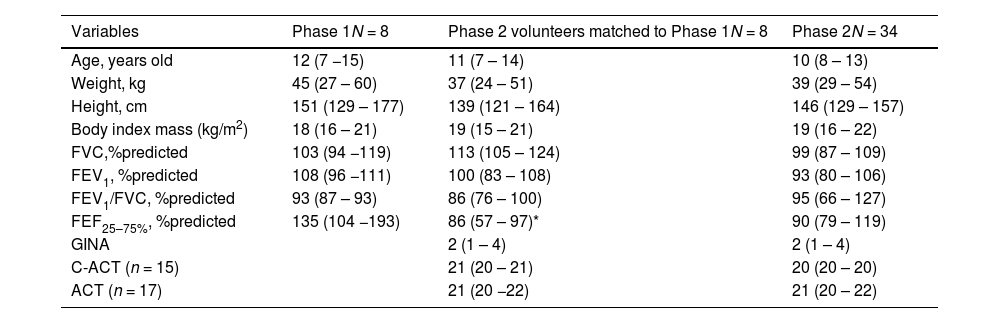
Characteristics of the studied participants. Variables described as median (IQ 25–75%).
| Variables | Phase 1N = 8 | Phase 2 volunteers matched to Phase 1N = 8 | Phase 2N = 34 |
|---|---|---|---|
| Age, years old | 12 (7 −15) | 11 (7 – 14) | 10 (8 – 13) |
| Weight, kg | 45 (27 – 60) | 37 (24 – 51) | 39 (29 – 54) |
| Height, cm | 151 (129 – 177) | 139 (121 – 164) | 146 (129 – 157) |
| Body index mass (kg/m2) | 18 (16 – 21) | 19 (15 – 21) | 19 (16 – 22) |
| FVC,%predicted | 103 (94 −119) | 113 (105 – 124) | 99 (87 – 109) |
| FEV1, %predicted | 108 (96 −111) | 100 (83 – 108) | 93 (80 – 106) |
| FEV1/FVC, %predicted | 93 (87 – 93) | 86 (76 – 100) | 95 (66 – 127) |
| FEF25–75%, %predicted | 135 (104 −193) | 86 (57 – 97)* | 90 (79 – 119) |
| GINA | 2 (1 – 4) | 2 (1 – 4) | |
| C-ACT (n = 15) | 21 (20 – 21) | 20 (20 – 20) | |
| ACT (n = 17) | 21 (20 −22) | 21 (20 – 22) |
GINA, Global Initiative for Asthma. Each step of GINA describes the amount of medication taken for asthma treatment. Step 1: low dose of inhaled corticosteroid (ICS) whenever SABA is taken; Step 2. low dose ICS + short-acting beta2-agonist (SABA) as needed; Step 3: low dose of ICS and long-acting beta2-agonist (LABA) + SABA as needed; Step 4: Medium dose of ICS and LABA + SABA as needed; Step 5: High dose of ICS and LABA or add-on therapy e.g. anti-IgE. Low/medium and high dose depends on the product.
C-ACT: Childhood Asthma Control Test; ACT: Asthma Control Test.
Comparison of outcomes at the peak of exercise between tests PAY test (Performance Activity in Youth) and cardiopulmonary exercise test (CPET) in healthy participants (n = 8). Variables described as median (IQ 25–75%).
| PAY test | CPET | p | |
|---|---|---|---|
| Heart rate, bpm | 145 (139– 153) | 188 (187– 191) | 0.012 |
| VO2 peak, mL/kg | 33.7 (30.0 – 39.7) | 40.1 (29.4– 44.1) | 0.012 |
| VE peak, L/min | 25.0 (17.2 – 36.7) | 52.5 (32.7 – 72.6) | 0.017 |
VO2peak, peak oxygen uptake; VE, minute ventilation.
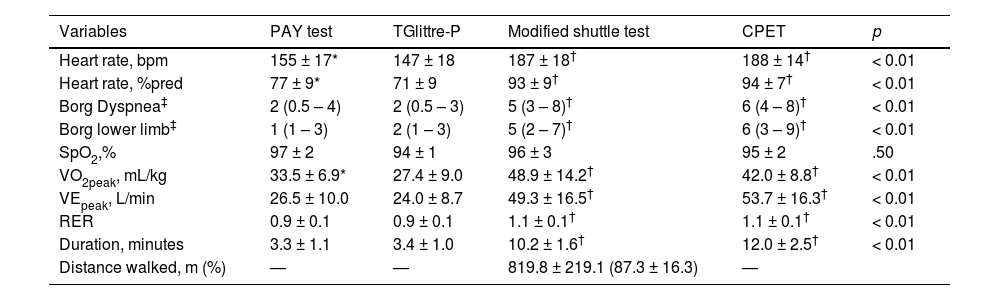
A total of 34 (21 males) participants had been diagnosed with mild to moderate asthma, without impairment in asthma control (ACT or C-ACT > 20) (Table 1). In general, their lung function was normal (Table 1). Eight of these participantes were matched to the healthy participants to study the descriminative validity (Table 1). The participants with asthma had higher HR and VO2peak in the PAY test than in TGlittre-P (p < .01). However, as expected, participants with asthma showed lower HR, Borg, VO2peak, and VEpeak in the PAY test than in MST and CPET (p < .01, Table 3).
Comparison of outcomes at the peak of exercise between tests: PAY test (Performance Activity in Youth), Pediatric Glittre test (TGlittre-P), modified shuttle test and cardiopulmonary exercise test (CPET) in participants with asthma, n = 34. Variables described as mean ± SD.
| Variables | PAY test | TGlittre-P | Modified shuttle test | CPET | p |
|---|---|---|---|---|---|
| Heart rate, bpm | 155 ± 17* | 147 ± 18 | 187 ± 18† | 188 ± 14† | < 0.01 |
| Heart rate, %pred | 77 ± 9* | 71 ± 9 | 93 ± 9† | 94 ± 7† | < 0.01 |
| Borg Dyspnea‡ | 2 (0.5 – 4) | 2 (0.5 – 3) | 5 (3 – 8)† | 6 (4 – 8)† | < 0.01 |
| Borg lower limb‡ | 1 (1 – 3) | 2 (1 – 3) | 5 (2 – 7)† | 6 (3 – 9)† | < 0.01 |
| SpO2,% | 97 ± 2 | 94 ± 1 | 96 ± 3 | 95 ± 2 | .50 |
| VO2peak, mL/kg | 33.5 ± 6.9* | 27.4 ± 9.0 | 48.9 ± 14.2† | 42.0 ± 8.8† | < 0.01 |
| VEpeak, L/min | 26.5 ± 10.0 | 24.0 ± 8.7 | 49.3 ± 16.5† | 53.7 ± 16.3† | < 0.01 |
| RER | 0.9 ± 0.1 | 0.9 ± 0.1 | 1.1 ± 0.1† | 1.1 ± 0.1† | < 0.01 |
| Duration, minutes | 3.3 ± 1.1 | 3.4 ± 1.0 | 10.2 ± 1.6† | 12.0 ± 2.5† | < 0.01 |
| Distance walked, m (%) | — | — | 819.8 ± 219.1 (87.3 ± 16.3) | — |
VO2peak, peak oxygen uptake; VE, minute ventilation; RER, respiratory exchange ratio.
There was a moderate to strong correlation among the PAY test time, TGlittre-P time, and distance walked in the MST. All other correlations among the PAY test time, MST, and CPET were only weak to moderate (Table 1 Supplementary).
The PAY test time was longer in participants with asthma (3.1 min, range: 3.0–3.4 min) than in healthy participants (2.3 min, range: 2.2–2.4 min) (p < .001). The heart rate and minute ventilation were higher among participants with asthma in the PAY test (HRpeak: 163 bpm [153–180 bpm]; VEpeak: 43 L/min [32–52 L/min]) compared to the healthy participants (HRpeak: 145 bpm [139–153 bpm]; VEpeak: 25 L/min [17–37 L/min]) (p < .02). The VO2peak was lower among those with asthma (29 mL/kg [27–30 mL/Kg]) compared to the healthy participants (VO2peak: 34 [30–40 mL/kg]) (p 0.028) during the PAY test. The charactersitics of the healthy and asthma participants, macthed by age and sex, are in Table 1.
The PAY test showed significant reproducibility for all outcomes, except VO2peak (p < .01, Table 2 Supplementary). Using a Bland–Altman plot analysis, a bias regarding the PAY test time of −0.22 s (CI95% −0.9–0.43 s) (Fig. 3 - Supplementary online file).
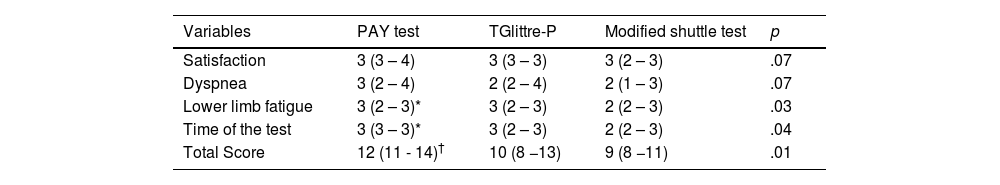
A comparison of the participant's satisfaction with the PAY and other tests is shown in Table 4. The participants expressed greater satisfaction when performing the PAY test compared to the TGlittre-P or MST (p < .01).
Satisfaction score to perform functional capacity tests. The higher score, the better satisfaction (n = 34). Variables described as median (IQ25–75).
| Variables | PAY test | TGlittre-P | Modified shuttle test | p |
|---|---|---|---|---|
| Satisfaction | 3 (3 – 4) | 3 (3 – 3) | 3 (2 – 3) | .07 |
| Dyspnea | 3 (2 – 4) | 2 (2 – 4) | 2 (1 – 3) | .07 |
| Lower limb fatigue | 3 (2 – 3)* | 3 (2 – 3) | 2 (2 – 3) | .03 |
| Time of the test | 3 (3 – 3)* | 3 (2 – 3) | 2 (2 – 3) | .04 |
| Total Score | 12 (11 - 14)† | 10 (8 −13) | 9 (8 −11) | .01 |
PAY test, Performance Activity in Youth.
The authors performed a post hoc power analysis, and the lower power observed was 79.8% (G*Power 3.1).
DiscussionThis study presents a new test to assess functional performance in children and adolescents with asthma. The PAY test was found to be feasible, valid, and reliable. The PAY test is straightforward and involves relevant activity participation for youth, as its activities involve the upper and lower limbs and reproduce their day-to-day routines.25 The test provides a standardized method for evaluating the functional performance of children and adolescents with chronic conditions.
As expected, the performance of the PAY test was more vigorous than that of the TGlittre-P test; additionally, the metabolic and cardiovascular demands of MST or CPET were higher than those of the PAY test. As known, the MST is a high-intensity exercise similar to CPET,26,27 differing from everyday activity (as observed in the PAY test).
A previous study found no differences between healthy and diseased (cystic fibrosis) in the pediatric population regarding the TGlittre-P test,14 which seems to lack sensitivity in determining functional capacity impairment.28 This outcome indicates that assessing the functional capacity of children with chronic pulmonary disease using tests developed for adults may present atypical results.29 The authors showed that the PAY test can effectively assess functional performance because it is not a high-intensity test, although it has higher metabolically, ventilatory, and cardiovascular responses than the TGlittre-P test.
The validation was confirmed by correlating the PAY test to TGlittre-P, MST, and CPET outcomes. The faster the PAY test time, the faster the TGlittre-P time, the longer the distance walked in the MST, and the higher the workload at the end of the CPET. Additionally, the faster the PAY test time, the higher the VO2peak at MST and CPET, with similar results for minute ventilation.
This study is the first field test in which the functional performance of children and adolescents with chronic lung disease was evaluated based on their own tasks. Thus, the authors compared the PAY test to TGlittre-P, which has ADL tools, MST, a functional capacity test, and CPET, the gold standard for exercise capacity. The discriminate validity of the test was confirmed because participants with asthma took more time to perform the PAY test than healthy participants. This result shows that it is possible to properly assess functional performance in youth by applying the PAY test.
No physiological differences were observed between the PAY test and the retest. This shows good reproducibility. However, the limits of agreement in the Bland–Altman analysis indicated that the second test was almost 1 min (0.54 s) shorter than the first one. The learning effects of field tests have been well-documented.13 Thus, the authors suggest performing the PAY test twice and using the best time test (the faster one) for analysis.
An interesting result was the satisfaction of the participants while performing the PAY test. The highest score was for the new test. This is relevant as enjoyment is an essential factor in motivating a child to perform a test.
An important clinical implication of this study is that the PAY test offers a new approach to assessing functional performance in the pediatric population. Additionally, the test is feasible, does not need specific and expensive equipment, can be administered by one professional, and is representative of children's and adolescents’ activities with moderate metabolic consumption. It was found to be enjoyable by the volunteers in this study. Further, the PAY test can be included as an evaluation of functional performance among the pediatric population.
This study has some limitations. The authors did not split the sample into children and adolescents, considering the number of tests performed on each volunteer. The sample size was based on the expected correlation between PAY test time and TGlittre-P test time. Further, the study was conducted in a single center. Other protocols that include different severities and lung diseases should be performed to determine the validity and reproducibility of the PAY test.
In conclusion, the findings of this study demonstrate the feasibility of the PAY test as a new approach to assessing the functional performance of children and adolescents. The test was found to be reproducible, enjoyable, easily performed by participants, and low-cost. The activities in the PAY test provide consistent physiological responses based on the gold standard and field tests. Thus, the test is a valid method for evaluating the functional performance of children and adolescents with asthma.
Funding/SupportNone.
Institution: Universidade Federal de Minas Gerais (UFMG) and Universidade Nove de Julho (UNINOVE).
This study was presented at: European Respiratory Society Congress, 2021, by Fernanda C. Lanza, as poster presentation.