to determine the frequency, complications and seasonality at which respiratory syncytial virus (RSV) infection of the lower respiratory tract causes hospitalization in infants of age 1 year or less in 6 cities of Colombia.
Methodsone-year prospective multicentric observational study that included 717 patients presenting to the emergency department with respiratory symptoms in 6 cities of Colombia. Hospitalized children were tested for RSV with an immunofluorescence rapid test in nasopharyngeal secretions. Descriptive and statistical analyses of the population were conducted.
Resultsthe study population included 717 patients with a mean age of 3.6 months (SD 3.25), 4:3 male: female ratio and a positive RSV LRTI prevalence of 30.0% (216 infants/City, range 26.0 - 49.0%). Risk factors for RSV LRTI were found in 8.2% of the population, of which 28.8% were RSV positive. RSV positive and negative groups were compared using a two-tailed t test with 95.0%CI, p < 0.05. No statistically significant differences were found. All cities presented specific year trimesters in the occurrence of RSV LRTI.
Conclusionsthe RSV caused 1 in 3 LRTI hospitalizations in the population, with an incidence of 30.0%. This confirms a continuous circulation of RSV in Colombia varying by geographic location.
determinar a frequência, as complicações e a sazonalidade com que a infecção pelo vírus sincicial respiratório (VSR) do trato respiratório inferior causa hospitalização em neonatos com um ano de idade ou menos, em seis cidades da Colômbia.
Métodosestudo observacional prospectivo multicêntrico de um ano que incluiu 717 pacientes, que compareceram ao serviço de emergência com sintomas respiratórios em seis cidades da Colômbia. As crianças hospitalizadas foram testadas para verificar a existência de VSR com teste de imunofluorescência das secreções nasofaríngeas. Foram realizadas análises descritivas e estatísticas da população.
Resultadosa população estudada incluiu 717 pacientes com uma idade média de 3,6 meses (DP 3,25), na proporção de 4:3 do sexo masculino para o sexo feminino e uma prevalência de ITRI por VSR de 30% (216 neonatos/cidade, faixa 26-49%). Os fatores de risco para ITRI por VSR foram encontrados em 8,2% da população, dos quais 28,8% foram positivos para VSR. Os grupos positivo e negativo para VSR foram comparados utilizando um teste t bicaudal com IC de 95%, p < 0,05. Não foram constatadas diferenças estatisticamente significativas. Todas as cidades apresentaram trimestres anuais específicos para ocorrência de ITRI por VSR.
Conclusõeso VSR causou uma em três internações de ITRI na população, com uma incidência de 30%. Isso confirma uma circulação contínua do VSR na Colômbia, que varia pela localização geográfica.
The Respiratory Syncytial Virus (RSV) infection is a global public health problem and is the leading cause of lower respiratory tract infection (LRTI) in the pediatric population.1,2
In Latin America, respiratory infections remain the second leading cause of death in children under 5 years of age with RSV as the causative agent in 70.0% of these infections.3,4
RSV infection produces hospitalization in 2.0% of the pediatric population and causes a more severe clinical course with up to 20.0% of hospitalization in premature infants (<36 weeks of gestational age), and children with bronchopulmonary dysplasia, congenital heart disease, or neuromuscular and immune diseases.1,5–7Studies of RSV infection in Latin American countries have shown a range of RSV presence from 21.6% to 60.0% in children with LRTI and a range in hospitalized children for LRTI from 41.8% to 78.7%.3 In Colombia, some studies have reported an incidence of hospitalization for RSV in LRTI between 41.7% and 48.0%.6,8,9
In relation to seasonality, the incidence of RSV infection varies according to latitude, altitude, and weather of each of the regions.10 In countries with seasons, RSV occurs in an epidemic form in the winter season. In tropical and subtropical areas, endemic patterns have been described, with interspersed epidemic periods, although not clear in different geographic areas.3,11
It is known that RSV epidemics were recorded in the months of greatest rainfalls and colder temperatures. However, other reports suggest that in the equatorial regions, RSV infection is evenly distributed throughout the year, with some variable increases.9,11
In Colombia, there are records of RSV infection in different cities.9,11 However, local studies about the seasonality of infection are limited.
In Bogotá (the capital of Colombia), an endemic pattern of RSV infection has been reported primarily, with a peak occurrence of bronchiolitis in the first half of the year, correlated with the rainy season (April-June).11 Ministry of Health in its epidemiologic monitoring report of Bogotá has confirmed that most of the deaths that occur annually during the respiratory epidemic of the first half of the year are attributed to RSV, and occur especially in infants under one year of age.12
In other cities of Colombia the seasonality as well as the reports of RSV infection and frequent complications in specific pediatric age groups is few. Due to this lack of information, the objective of this study is to determine the seasonality, frequency and high-risk patient complications of RSV LRTI in children less or equal to one year of age requiring hospitalization in six selected institutions in different cities of Colombia.
Materials and methodsThe design was a prospective multicentric observational study, including medical institutions located in six cities of Colombia (Bogotá, Cali, Medellín, Barranquilla, Bucaramanga and Pereira), lasting one calendar year (April 2005–April 2006).
The selected institutions were characterized by reporting between 1000-2000 pediatric visits monthly and 100-200 hospitalizations for LRTI in infants of one year of age or less.
Given previous reports of RSV positivity on around 50.0% of patients hospitalized for LRTI in Colombia, we calculated a minimum sample size of 500 patients of one year or less hospitalized with suspicion of RSV LRTI.
The total number of patients included in the study was 717 and met the following inclusion criteria: 1) to be one year of age or less 2) to have visited the emergency department and been hospitalized for suspicion of LRTI (diagnosis of bronchiolitis, pneumonia, or bronchopneumonia).
After the patients were hospitalized, the presence or absence of RSV was confirmed by performing a rapid immunofluorescence test in nasopharyngeal secretion (Clearview RSV antigen detection test). The reported test sensitivity was 95.2%, specificity 99.3%, PPV 95.2% and NPV of 99.3%.13 The results of the test were verified through an enzyme immunoassay (Directigen RSV), performed in one of the institutions participating in the study (Clinic of the Americas, Medellín).13
Risk factors such as gestational age less than 32 weeks at birth, and chronic lung disease were determined. Clinical outcomes such as average hospital stay, admission to the pediatric intensive care unit, mechanical ventilation requirement, and mortality were assessed in high-risk patients. RSV positive and negative groups were compared.
All the protocols and informed consent were reviewed and approved by the ethics committee of each institution.
Statistical analysisA descriptive analysis of the population was conducted. Incidence of patients with confirmed RSV LRTI was calculated by trimester and city. RSV positive and negative groups were compared using a two-tailed t test with 95% CI, p < 0.05. The results were compared between cities. The statistical software SAS 9.0 was used.
ResultsThe total number of patients included in the study was 717 infants that met the inclusion criteria.
The average age of the patients was 3.6 months (SD 3.25), with a male/female ratio of 4:3. The primary diagnoses of the patients included: bronchiolitis in 67.0%, pneumonia in 23.0%, bronchopneumonia in 9.8%, and other in 0.3%.
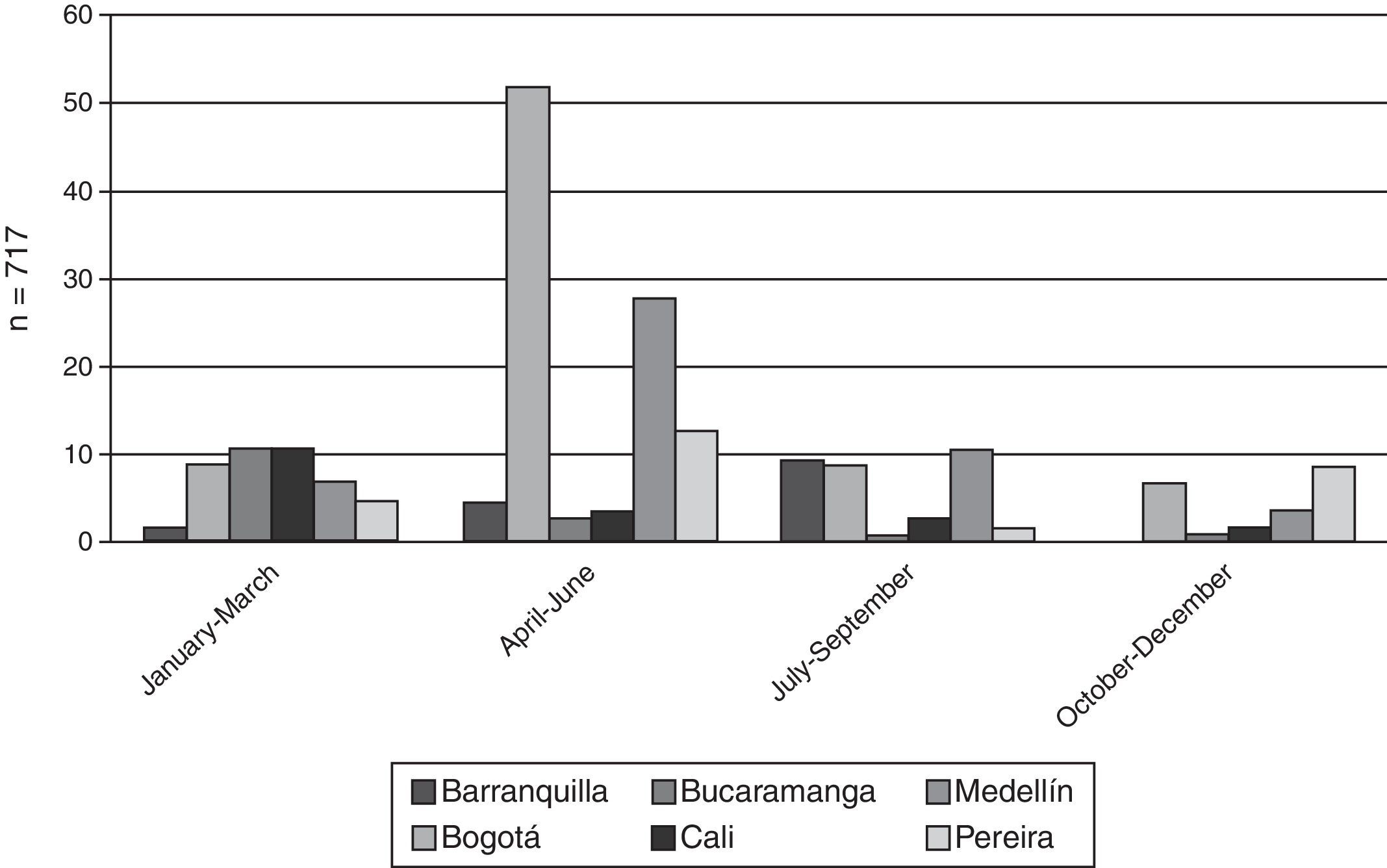
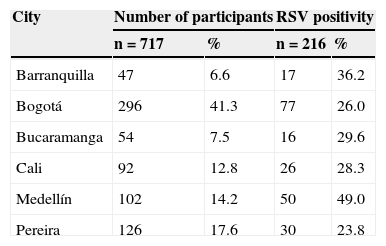
The RSV test was positive in 216 patients, which corresponds to an incidence of 30.0% in the general study population (Table 1). In the other cities the range of variability of RSV positivity was 23.8% to 49.0% (Table 1).
In relation to presenting risk factors for RSV LRTI, 59 patients (8.2%) had risk factors such as gestational age less than 32 weeks at birth, or chronic lung disease. The RSV test was positive in 28.8% of these patients, which suggests that in the high-risk patients the infection proportion is similar to the general population.
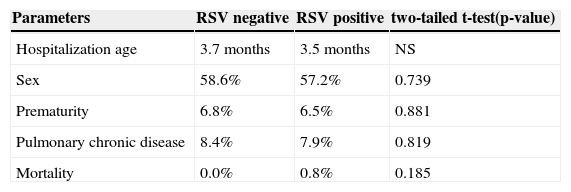
In the RSV positive high-risk patients, the average hospital stay was 8.6 days per patient, and 52.9% were admitted to the Pediatric Intensive Care Unit (PICU) with an average stay of 8.3 days per patient. Of these patients, 41.2% required mechanical ventilation for 3.8 days on average. Mortality was 5.8% (Table 2).
Comparison between positive and negative respiratory syncytial virus patients.
| Parameters | RSV negative | RSV positive | two-tailed t-test(p-value) |
|---|---|---|---|
| Hospitalization age | 3.7 months | 3.5 months | NS |
| Sex | 58.6% | 57.2% | 0.739 |
| Prematurity | 6.8% | 6.5% | 0.881 |
| Pulmonary chronic disease | 8.4% | 7.9% | 0.819 |
| Mortality | 0.0% | 0.8% | 0.185 |
RSV, respiratory syncytial virus.
After comparing the group of RSV positive and negative patients, there were no statistically significant differences between the analyzed parameters such as hospitalization age, sex, prematurity, chronic lung disease and mortality (Table 2).
Fig. 1 shows the incidence of RSV positive cases detected by trimesters in different cities. In general the RSV LRTI incidence among cities was not statistically different. At most, there is an epidemic trend of RSV occurrence during the April-June trimester of the year with the highest percentage of RSV positive cases in the cities of Bogotá and Medellín. The other cities had similar incidences of RSV positive cases throughout the year.
Discussion and conclusionsThis study confirms that the Respiratory Syncytial Virus is a frequent cause of hospitalization for LRTI in infants of one year of age or less in Colombia, with an incidence of 30.0%, not only in the general population but also in high-risk patients, which is comparable with previous local studies.8,9,11,12,14 In the city of Cali.14 findings showed that in a cohort of 340 infants followed for 18 months, RSV was the most common causative agent of RTI with 13.0% RSV positivity of the viral isolated and known to occur endemically throughout the year.8 In Medellín a 44.0% RSV positivity was reported in the overall monitoring of pediatric patients with LRTI, from which 77.0% of patients were under one year of age.6,8 Another study in Medellín showed a 41.7% incidence of RSV in children of less than one year of age hospitalized for LRTI. Infants with confirmed RSV infection had an average age of 3.2 months (SD +/- 2.9), with 82.2% of the cases appearing before six months of age and 62.8% presenting cases before two months of age with an average RSV positive case hospitalization of 6.1 days (SD +/- 3.4).13 Our study findings are consistent with these previous local reports, and also with international reports of 7.8% of patients with risk factors (prematurity or chronic lung disease).3,6 In these hospitalized high-risk patients RSV was confirmed in 1 out of 3 patients, and complications and mortality were high.
Most patients of one year of age or less were hospitalized for RSV LRTI before six months of age, which means that they could benefit from RSV prophylaxis.1,6
Overall RSV can occur in Colombia throughout the year in an endemic pattern with some peaks of increased hospitalization. These periods do not necessarily coincide between cities, which can be partly explained by climatic differences given by periods of rainfall, relative humidity, height above sea level and daily temperature variability.
In addition to the above results, longitudinal studies are recommended to assess RSV incidence and prophylaxis implementation across the country to prevent RSV infection, and to decrease complications and mortality in infants.
The limitations in our study include the small sample sizes per city (irrespective of a good total sample size of 717), the total duration time of one calendar year, since some similar studies last longer periods, and the fact that RSV prophylaxis implementation was not assessed, which could have provided information on the course of the disease in these populations.
FundingThis study was financed by Abbott Laboratories in Colombia 2004.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Piñeros JG, Baquero H, Bastidas J, García J, Ovalle O, Patiño CM, et al. Respiratory syncytial virus infection as a cause of hospitalization in population under 1 year in Colombia. J Pediatr (Rio J). 2013;89:544–548.