To examine if the substitution of different screen time intervals with light physical activity (LPA), moderate to vigorous physical activity (MVPA) and sleep is associated with cardiovascular indicators and inflammatory markers in children.
MethodsThis is a cross-sectional study developed with 186 children aged between six and 11 years old from public schools in southern Brazil. CRF was measured with the 6-minute running and walking test, following the Brazil Sports Project procedures. The percentage of fat was evaluated through DXA. LPA and MVPA were measured using accelerometers. Sleep and screen time were assessed by questionnaires answered by parents. Leptin and C-reactive protein were measured by fasting blood collection. Systolic and diastolic blood pressure were determined through a digital sphygmomanometer. Isotemporal substitution models were used for statistical analysis.
ResultsReplacing 1 h of screen time with MVPA was associated with lower BMI, systolic and diastolic blood pressure, fat percentage, leptin, and C-reactive protein. When screen time was substituted for sleep time, lower waist circumference was observed. Regarding the substitution of 1 h of screen time with LPA, significant values were found only for leptin.
ConclusionThe replacement of screen time with physical activities of different intensities and sleep time was associated with benefits in cardiovascular indicators and inflammatory markers in childhood.
The benefit of daily movement behaviors such as sufficient physical activity, low screen time exposure, and adequate sleep time in childhood is scientifically evidenced.1 Also, long time spent in front of screens, combined with inadequate sleep for age and insufficient time in moderate- to vigorous-intensity physical activity (MVPA), is associated with cardiometabolic risk factors,2 including increased frequency of overweight and obesity.3
Despite the recommendation that children aged between 6 and 18 years should spend at least 60 min a day in MVPA, have between 9 and 11 h of quality sleep, and not exceed 2 h a day in front of screens,1,4 the number of children who comply with the recommendations is low. In Brazil, 25 % meet the screen time guideline, 44 % the physical activity guideline, and 30 % the guideline for sleep.5 Studies have shown that non-compliance with any of the 24-h movement behavior recommendations is associated with higher body mass index (BMI), waist circumference, blood pressure, and lower cardiorespiratory fitness (CRF). Conversely, meeting the 24-h movement guidelines is associated with better overall health.6,7
Tremblay et al.1 suggest that children should, as far as possible, replace behaviors that are harmful to health, such as screen time with physical activity at different intensities, and also with adequate sleep. The excess time spend in front of screens is related to adverse effects on health, including higher adiposity and clustered cardiometabolic risk scorers, and lower CRF.7,8 Although there is consistent knowledge about the relationship between the breaks in sedentary behavior and light-intensity physical activity (LPA) in adults, there is little evidence about this relationship in children.9,10 Despite some knowledge about the relationship of isotemporal replacement models with obesity and with some cardiometabolic risk factors,2 there is a gap in the literature on the reallocation of time between 24-h movement behaviors in children living in low- and middle-income countries. Bridging this gap is crucial, and could be achieved by a multifaceted approach, as demonstrated in a study developed in Ecuador. The study developed a combination of implemented individual and environment-based strategies, resulting in a reduction in screen time.11 Such knowledge is fundamental to developing effective public health interventions, such as reducing the sitting time during school hours and encouraging more active classes, recess, and commuting, as observed in previous studies that implemented school-based interventions, and smartphone app intervention to increase physical activity and decreasing screen time.12,13 Therefore, this study aimed to examine if the substitution of different screen time intervals with LPA, MVPA, and sleep was associated with cardiovascular indicators and inflammatory markers in children.
MethodsThis study was part of the “School Sports and Health Project” approved by the Ethics and Research Committee of the Federal University of Rio Grande do Sul (register 2571,198), which aimed to verify the effect of an intervention with MVPA and eating habits on various health outcomes. Participants were 186 students (92 boys) from two public schools in a southern Brazilian city, between the 1st and 5th grades of elementary school, aged between six and 11 years old (Mean = 8.57 ± 1.56). The study used schools with pre-existing university agreements and a convenience sample. It began with a meeting to inform parents and guardians about the research. All school community members were invited, and those who agreed provided informed consent.
A posteriori sample calculation was performed using the G*Power software (v 3.1.9.2). The resulting statistical power was 0.82, considering a minimum sample size of 71 children, an average effect (F2 = 0.25), an alpha of 0.05, and eight predictors for generalized linear regression models.
MeasuresThe assessments were carried out by physical education teachers and nurses or nursing technicians over two months in their respective schools and at the Exercise Research laboratory. Physical fitness, anthropometry, blood collection, and dual-energy x-ray absorptiometry (DXA) assessments were performed in the initial two weeks.
Blood collection, accelerometer usage, and body fat assessment (DXA) procedures were prearranged with the parents/guardians. Meetings were conducted to instruct them on accelerometer usage and questionnaire completion. Accelerometers were placed and removed in schools and attending parents/guardians filled out the questionnaires. For those who didn't attend, the questionnaires were sent and collected via the children.
The procedures for blood collection, use of accelerometers, and assessment of the percentage of fat (DXA) were previously scheduled with the parents/guardians of each child. Meetings were held with parents/guardians on how to use the accelerometers and fill out questionnaires. Thus, the placement and removal of accelerometers took place in the schools, and the parents/guardians who attended the meetings filled out the questionnaires. The questionnaires were sent and collected through the children for those who did not attend.
Fat percentageFat percentage assessment was conducted using a GE Healthcare DXA machine (Lunar Prodigy model). The device was calibrated daily before assessments. During evaluations, children removed metallic items and wore fastener-free clothing. Positioned in a supine manner, they remained still for about five minutes as the equipment's arm passed over their body from head to foot. The measurements were automatically calculated by the equipment's software.
Anthropometry and physical fitnessChildren were asked to be barefoot and in light-weight clothing. Waist circumference was measured using a flexible tape (1 mm resolution). Body mass was verified on a digital scale (kg). Both height and sitting height were evaluated using a measuring tape with a precision of 2 mm, in centimeters. Subsequently, BMI was calculated.
The 6-min run and walk test, following Proesp-Br criteria,14 assessed CRF on school courts. The test featured demarcations every two meters and cones for clear guidance. Children worked in small groups, maintaining a consistent pace (running or walking). At the 6-min mark, they ceased running and stayed in place for distance recording, calculated as meters (laps multiplied by court size plus meters of the last lap).
24-h movement behaviorPhysical activity levels (LPA and MVPA) were assessed using an accelerometer Actigraph (wActiSleep-BT Monitor) placed at the waist. The device was worn for seven consecutive days, removing it only for aquatic activities. For data analyses, a minimum use of five days (including at least one weekday and one weekend), with at least 10 h/day of use was needed for inclusion in the analyses. Data were collected at a sampling rate of 80 Hz, downloaded in one-second epochs, and aggregated for 15-s periods. Regarding the classification of physical activity levels, counts were used for the accelerometer cut-off points proposed by Evenson (2008).15 Data were analyzed using Actilife software (ActiGraph®, version 5.6, USA).
For the assessment of screen and sleep time, questionnaires were sent to be answered by parents/guardians. The screen time question was: "On average, how much time does your child watch TV, play video games, or spend on the computer or cell phone daily?" As for sleep time, the questions were: "On average, what time does your child go to bed?" and "On average, what time does your child get up?" Then, the child's hours of sleep were calculated.
Systolic and diastolic blood pressureA digital sphygmomanometer (Omron – Model HEM 7200, Kyoto, Japan) was used on the right arm with a proper size cuff for each participant's arm circumference. The child remained seated for at least five minutes for their blood pressure to be measured.16
Leptin, a C-Reactive proteinBlood collection was performed in the schools after a minimum of 12 h of fasting. The blood samples were transferred to the Exercise Research laboratory of the School of Physical Education, Physiotherapy, and Dance in thermal boxes to maintain the appropriate temperature. Afterward, they were centrifuged at 3500 rpm for 15 min. Then, plasma and serum were aliquoted and frozen at −20 °C until measurement. Leptin and C-Reactive protein were evaluated from a specific human kit, using the ELISA technique, performed in a microplate reader (Multiskan Go, Thermo Scientific, Waltham, USA).
Somatic maturationSomatic maturation was assessed by determining the difference in years from the peak of growth velocity, using a regression equation that considered chronological age, height, body mass, sitting height, and lower limb length. The procedures of a prior study were followed for this assessment. To calculate lower limb length, height and sitting height values were used, and sex-specific equations were applied.17
Statistical analysisMeans, standard deviations, frequencies, and minimum and maximum values were used to characterize the sample. For the effects of relocation between screen time, LPA, MVPA, and sleep, and its relation to cardiovascular indicators and inflammatory markers, the authors used isotemporal substitution. For the reallocation time of 1 h, the variables screen time, LPA, MVPA, and sleep were calculated in hours, as was the analysis of 1 min, organizing the variables in min. For the 20-minute analysis, variables were divided by a constant of 20, so the regression coefficients consistently represented the reallocation of 20 min/day. First, the authors examined the association between each exposure variable (screen time, LPA, MVPA, sleep) with the cardiovascular indicators and individual inflammatory markers using a unique linear regression model to examine the total effect for each behavior.
Second, the authors examined the associations of each exposure variable, considering the control of the other exposure variables. The authors omitted the total time, as it is the sum of the four behaviors of the 24-hour movement (screen, LPA, MVPA, sleep). Finally, the authors used isotemporal substitution models to examine the estimated effects of replacing time spent on one behavior with an equal amount of time spent on another while keeping the total time constant by removing the behavior of interest (screen time) from the model. With this approach, the regression coefficient for the domains maintained in the model (LPA, MVP, and sleep) represents the theoretical effect of reallocating an equal amount of time spent in this domain with the same amount of time of the domain excluded from the model (screen time). None of the isotemporal models compromised the linear regression assumptions. All models adjusted for gender and somatic maturation and later for gender, somatic maturation, and CRF. All variables were tested for high collinearity. The statistical level was set at p < 0.05. All analyses were performed using the statistical program SPSS v. 22.0.
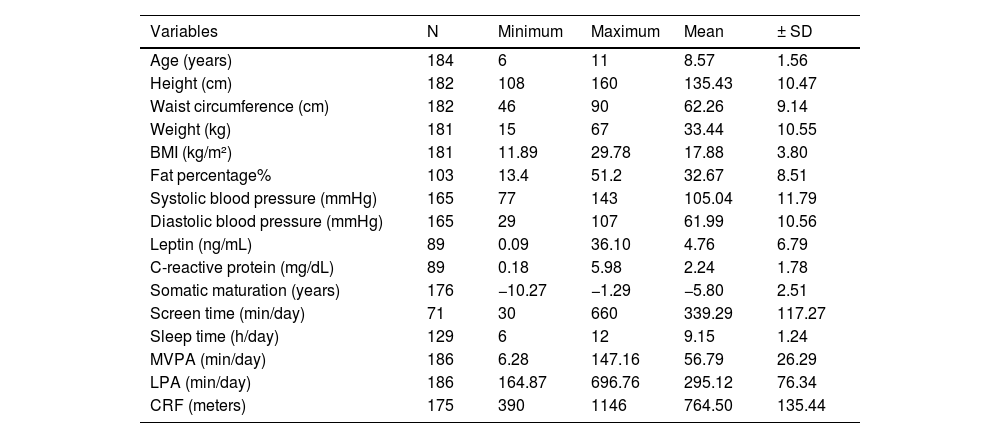
ResultsTable 1 presents the characterization of the sample. Although the mean MVPA was close to the daily recommendation for age (56.79 ± 26.294 min/day), it was not the best indicator for this outcome due to the wide range of values observed (6.18 to 147.16 min/day). The authors noticed a high daily mean of minutes in front of the screens (339.29 ± 117.27 min/day). The sleep time ranged between six and twelve hours per night (9.15 ± 1.24).
Sample characteristics.
BMI, Body mass index; MVPA, moderate to vigorous physical activity; LPA, light-intensity physical activity; CRF, cardiorespiratory fitness; SD, standard deviation.
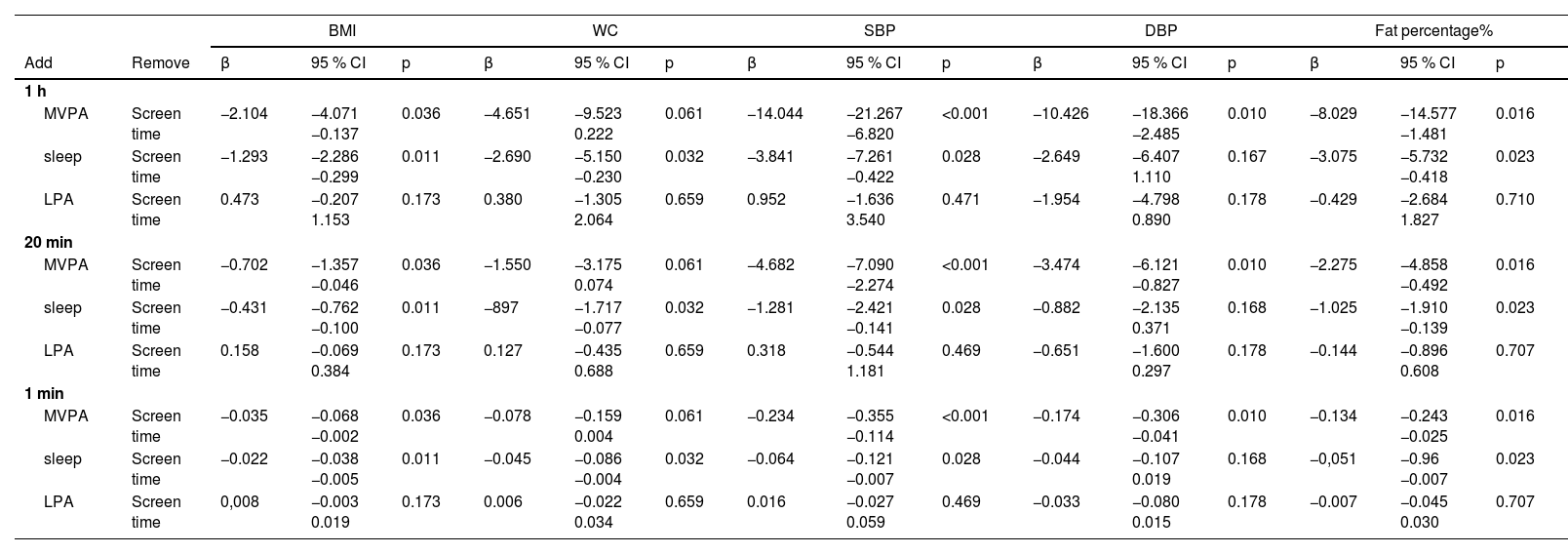
In the substitution of different screen time intervals with MVPA, LPA, and sleep time, cardiovascular indicators showed good improvement when adjusted for gender and somatic maturation (Table 2). BMI, systolic and diastolic blood pressure, and fat percentage underwent positive changes when MVPA replaced screen time (in all time intervals tested). Furthermore, waist circumference also showed significant improvement when screen time was replaced by sleep time. In the case of LPA replacement, the authors did not find any statistically significant differences.
Isotemporal substitution of movement behaviors on cardiovascular indicators.
Analyses adjusted for sex and somatic maturation.
MVPA, moderate to vigorous physical activity; BMI, body mass index; LPA, light-intensity physical activity; WC, waist circumference; SBP, systolic blood pressure; DBP, diastolic blood pressure.
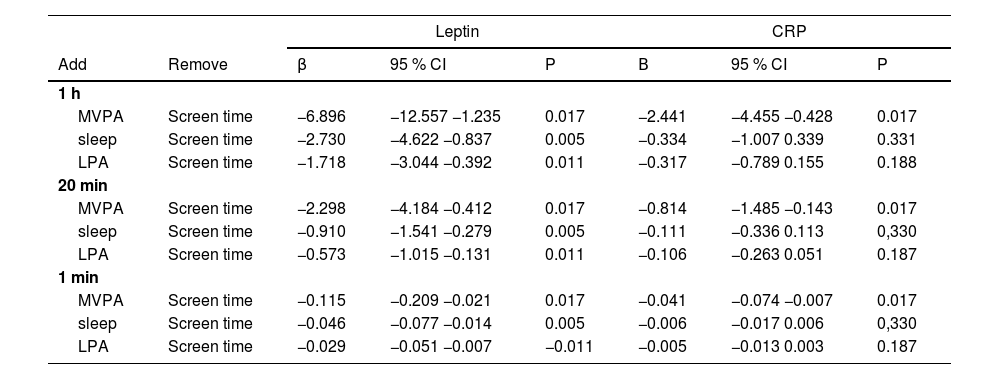
Table 3 shows the isotemporal substitution of sleep time, MVPA, and LPA for screen time in inflammatory markers (adjusted for sex and somatic maturation). For leptin, a beneficial behavior was perceived in the exchange of screen time for any other tested behavior. On the other hand, C-reactive protein presents positive changes only when the screen time is replaced by MVPA.
Isotemporal substitution of movement behaviors in the inflammatory markers.
Analyses adjusted for sex and somatic maturation.
MVPA: moderate to vigorous physical activity; LPA: light-intensity physical activity; CRP: C-Reactive protein.
When adjusted for gender, somatic maturation, and CRF, both in cardiovascular indicators and inflammatory markers (Supplementary material 1 and 2, respectively), the replacement of screen time by MVPA remained positive when associated with BMI, waist circumference, systolic and diastolic blood pressure, fat percentage and leptin. The substitution for sleep time was significant for BMI, waist circumference, systolic blood pressure, fat percentage, and leptin. The substitution for LPA maintained the same behavior when there was no adjustment for CRF. There was no change in C-reactive protein with this adjustment.
DiscussionThe authors aimed to examine the associations of replacing different 24-h movement behaviors with cardiovascular indicators and inflammatory markers in children. The authors found that the replacement of screen time with MVPA, even if only for 1 min, was associated with a reduction in the risk of different indicators of cardiovascular diseases. This reinforces the importance of reducing time spent in front of screens and the significance of moderate- to vigorous-intensity physical activity in line with global recommendations.4
Although previous studies have examined similar associations in preschool children,18,19 to the best of our knowledge, this is the first study conducted only with children from a middle-income country. This association has been examined among children from Norway, Sweden, Portugal, and the United Kingdom.20 In addition to the present study addressing the 24-hour movement behaviors associated with cardiovascular indicators, it should be noted that such associations occurred regardless of the CRF levels of the students. Therefore, children should be active and present healthy levels of physical fitness and also avoid excessive time in front of screens.4,1
These results showed that when replacing 1 hour, 20 min, or 1 min of screen time with the different intensities of physical activities and sleep time, it is possible to observe benefits in the cardiovascular indicators and inflammatory markers. Exchanging screen time intervals for MVPA showed significant improvements and interesting clinical effects on BMI, systolic and diastolic blood pressure, fat percentage, leptin, and C-reactive protein. Thus, adiposity parameters can be improved with an increase in MVPA when it replaces screen time.21 As for the exchange of screen time for sleep time, there would be a decrease in waist circumference and leptin when replaced with MVPA. In the substitution for LPA, there were only associations with a reduction of the average leptin values.
The reduction or break in the time that children spend in front of screens is associated with high inflammation values.22 Regarding leptin, the present results point to a protective association when considering substitution, including light-intensity physical activities, suggesting that even a “stand and sit” action may play a protective role against early cardiovascular risk, as has been mentioned in adults.3 Furthermore, the importance of sleep time as a moment of global physiological reorganization is impaired by excess screen time.23 Evidence has shown the relationship between sleep time and the risk of increased fat percentage in adults.3 Such evidence seems to extend to children, and these results suggest that sleep is being replaced by excessive screen time.
The present study suggests that behavioral changes throughout the day can be protective for body composition, especially obesity, which is high in prevalence in this population and is associated with early indicators of the development of cardiovascular diseases.20 The replacement of screen time with MVPA and sleep reduced fat percentage and BMI. However, the substitution of screen time for LPA did not show significant associations with variables related to adiposity.
The present findings agree with the literature suggesting the importance of replacing screen time with MVPA and its protective association with systolic and diastolic blood pressure levels. Wijndaele et al.24 indicated that replacing sedentary time with MVPA was beneficial for systolic and diastolic blood pressure, as well as waist circumference and clustered cardiometabolic risk. Additionally, when CRF was included in the model the authors observed that in MVPA substitution, the behavior was beneficial for BMI, waist circumference, systolic and diastolic blood pressure, fat percentage, and leptin. The substitution for sleep time also showed significant and positive associations with BMI, systolic blood pressure, and fat percentage. However, there were no differences in the substitutions for LPA. Regarding C-reactive protein, the authors did not observe benefits between the exchanges of different screen time intervals for any other behavior when there was an adjustment for CRF, indicating that this relationship may depend on this variable.
The authors found two studies that used isotemporal replacement of 24-hour movement behaviors and related them to inflammatory markers.7,25 Both found non-significant associations with C-reactive protein and insulin. Future studies are needed to strengthen the evidence on these associations in children, and also the need to explore the role of physical fitness in this relationship since these findings pointed to a change in associations when the model was adjusted for MVPA, especially in relation to sleep time.
Conversely, after the isotemporal replacement of screen time with different intensities of physical activity and sleep time, MVPA was the behavior that had the most significant positive impact on children's health This result highlights the importance of considering movement behaviors as a whole and not in isolation, covering the total 24 h of the day, and the need for health professionals, teachers, and parents to consider that the time spent on one behavior is directly affected by the choices of other behaviors throughout the day.1
The present study showed statistically significant results for cardiovascular indicators and inflammatory markers even at short time intervals of the substituted screen time (as little as one minute). This reinforces the importance of breaking up screen time ("breaks") with MVPA. Gaba et al.21 also found this association in replacing short sedentary episodes, standing, or breaks for activities more often. As this study focuses on children, this finding is important since sedentary behavior becomes substantially less fragmented as children age.26
Therefore, these findings emphasize the importance of limiting screen time, but acknowledge the challenges due to widespread screen use in modern society. Parents face a unique challenge given their own screen-dependent habits. Strategies like setting a positive example, creating screen-free areas, using parental controls, and encouraging a balanced mix of outdoor activities and family engagement can help children adhere to screen time guidelines.27 Additionally, the recommendation of less than 2 h of screen time per day may no longer be realistic due to increased screen-based school activities.28
Some limitations should be considered in this study, such as screen time and sleep time data evaluated by questions directed to parents/guardians. The study's cross-sectional design does not allow for establishing cause and effect relationships. The convenience sample from only two schools also requires caution for the generalization of the results. Finally, according to the WHO physical activity and sedentary behavior guidelines, among the existing research gaps are the different behavior curves between physical activity and sedentary behavior and several health outcomes.
The present results highlight the importance of promoting physical activity in children. It is suggested to rethink the time that children sit continuously in schools, highlighting the importance of active schools, and also the concern of teachers and guardians with the physical activity performed in their free time. Adequate sleep time and the role of physical fitness should also be part of health promotion activities.
In conclusion, the reallocation of different screen time intervals by MVPA and sleep time was associated with improving various cardiovascular indicators and inflammatory markers in children. These findings highlight the importance of children meeting the guidelines of all movement behaviors in the 24 h when promoting health. Emphasizing the need to reduce screen time, new approaches consider more time in MVPA, in addition to care with sleep hygiene during school ages.
Coordenação de Aperfeiçoamento de Pessoal de Nível Superior.
Institution: Universidade Federal do Rio Grande do Sul.