Oxidative stress has been shown to contribute to the pathogenesis of acute and chronic lung inflammatory diseases. This article aimed to evaluate the oxidant/antioxidant status of children with acute bronchiolitis through the measurement of plasma total antioxidant capacity, total oxidant status, and oxidative stress index.
MethodsChildren with acute bronchiolitis admitted to the pediatric emergency department of a university hospital between January and April of 2012 were compared with age-matched healthy controls. Patients with acute bronchiolitis were classified as mild and moderate bronchiolitis. Oxidative and antioxidative status were assessed by measurement of plasma total antioxidant capacity, total oxidant status, and oxidative stress index.
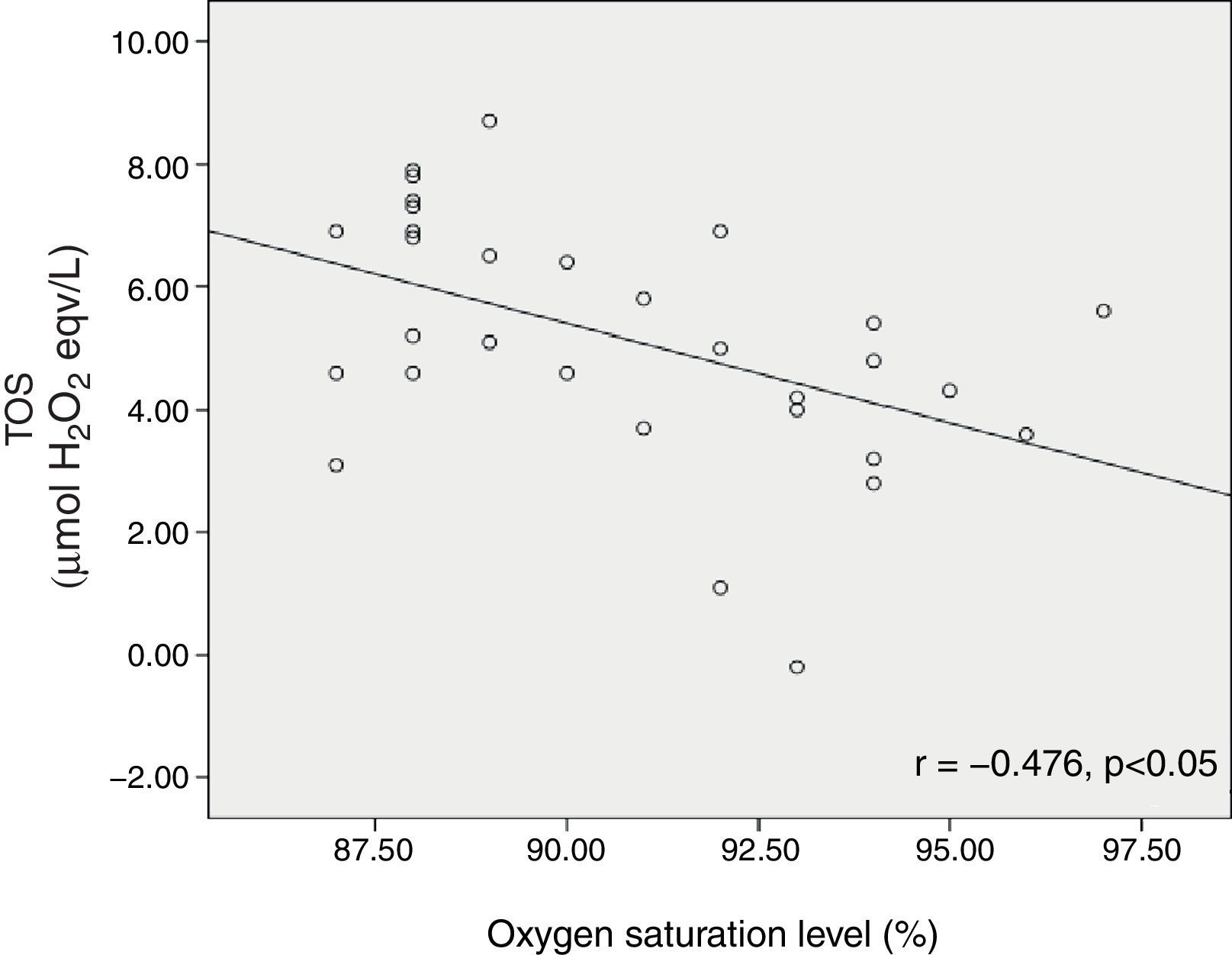
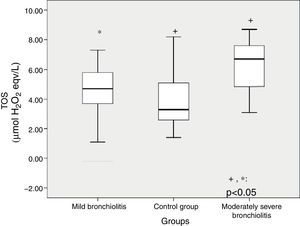
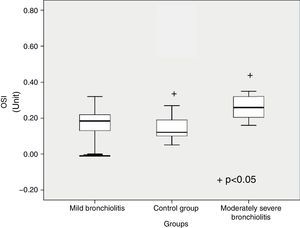
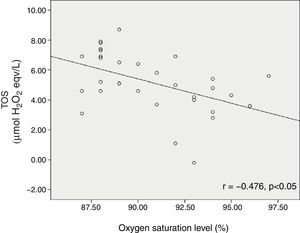
ResultsThirty-one children with acute bronchiolitis aged between 3 months and 2 years, and 39 healthy children were included. Total oxidative status (TOS) was higher in patients with acute bronchiolitis than the control group (5.16±1.99μmol H2O2versus 3.78±1.78μmol H2O2 [p=0.004]). Total antioxidant capacity (TAC) was lower in children with bronchiolitis than the control group (2.51±0.37μmol Trolox eqv/L versus 2.75±0.39μmol Trolox eqv/L [p=0.013]). Patients with moderate bronchiolitis presented higher TOS levels than those with mild bronchiolitis and the control group (p=0.03, p<0.001, respectively). Patients with moderate bronchiolitis had higher oxidative stress index levels than the control group (p=0.015). Oxygen saturation level of bronchiolitis patients was inversely correlated with TOS (r=−0.476, p<0.05).
ConclusionThe balance between oxidant and antioxidant systems is disrupted in children with moderate bronchiolitis, which indicates that this stress factor may have a role in the pathogenesis of the disease.
O estresse oxidativo demonstrou contribuir para a patogênese de doenças pulmonares inflamatórias agudas e crônicas. Nosso objetivo foi avaliar o estado oxidante/antioxidante de crianças com bronquiolite aguda por meio de mensuração da capacidade antioxidante total do plasma, estado oxidante total e índice de estresse oxidativo.
MétodosAs crianças com bronquiolite aguda encaminhadas para o Departamento de Emergência Pediátrica do hospital universitário entre janeiro e abril 2012 foram comparadas a controles saudáveis de mesma idade. Os pacientes com bronquiolite aguda tiveram essa doença classificada como leve e moderada. O estado oxidante e antioxidante foi avaliado pela mensuração da capacidade antioxidante total do plasma, estado oxidante total e índice de estresse oxidativo.
ResultadosForam incluídas 31 crianças com bronquiolite aguda com idade de três meses a dois anos e 37 crianças saudáveis. O estado oxidante total (EOT) foi maior em pacientes com bronquiolite aguda do que no grupo de controle (5,16±1,99μmol H2O2 em comparação a 3,78±1,78μmol H2O2 [p=0,004]). A capacidade antioxidante total (CAT) foi significativamente menor em crianças com bronquiolite que no grupo de controle (2,51±0,37μmol Trolox equivalente/L em comparação a 2,75±0,39μmol Trolox Eqv/L) (p=0,013). Os pacientes com bronquiolite moderada apresentaram níveis de EOT mais elevados que os com bronquiolite leve e os do grupo de controle (p=0,03, p<0,001). Os pacientes com bronquiolite moderada apresentaram níveis de IEO mais elevados que os do grupo de controle (p=0,015). O nível de saturação de oxigênio de pacientes com bronquiolite foi inversamente correlacionado ao nível de EOT (r=-0,476, p<0,05).
ConclusãoO equilíbrio entre os sistemas oxidante e antioxidante é interrompido em crianças com bronquiolite moderada, indicando que o fator de estresse poderá ter um papel na patogênese da doença.
Acute respiratory tract infections are important causes of morbidity and mortality in children, with a disease burden estimated at 112,900,000 disability-adjusted life years (DALYs), and 3.5 million deaths worldwide.1 In Turkey, respiratory tract infections were found to be the second most common cause of mortality among children between 0 and14 years of age.2 Due to its environmental interface, the lung is a major target organ for injury by exogenous oxidants such as environmental pollutants and endogenous reactive oxygen species (ROS) generated by inflammatory cells.3 The organism has enzymatic and non-enzymatic antioxidant systems to neutralize the harmful effects of the endogenous ROS products. Under certain conditions, the oxidative and anti-oxidative balance shifts towards the oxidative status, leading to a condition termed oxidative stress. Increased oxidative stress has been shown to contribute in the pathogenesis of many conditions, including acute and chronic airway diseases.4,5 Measurement of individual oxidant and antioxidant molecules have been used by researchers in several diseases including respiratory tract infections, but this requires a complex and costly procedure. Total oxidative status (TOS) and total antioxidative capacity (TAC) have more value than assessment of one part of these systems, and have shown good correlation with other oxidant stress markers.6,7 The present study aimed to define the oxidative and antioxidative status of children with acute bronchitis by measuring plasma TAC, TOS, and oxidative stress index (OSI).
MethodsStudy groupsThe study population comprised 31 children aged between 3 months and 2 years diagnosed with acute bronchiolitis at the pediatric emergency department of the Bezmialem Vakıf University between January and April of 2012. Acute bronchiolitis was defined as first episode of acute wheezing or rhonchi, tachypnoea, and chest retraction, preceded by or associated with cough, coryza, rhinorrhoea, and axillary temperature > 37.5°C.8 Patients were excluded from the study if they had an underlying disease that might affect the cardiopulmonary status (e.g. bronchopulmonary dysplasia, prematurity, assisted ventilation during the neonatal period, congenital heart disease, or immunodefficiency); asthma diagnosed by a physician; wheezing or cough previously treated with bronchodilators or corticosteroids within the preceding two weeks; or recurrent wheezing or history of chronic lung disease. A clinical illness grading scale for acute bronchiolitis patients was used to establish the severity of infection (scores 0 to 12 calculated according to general appearance, wheezing, retraction, and respiratory rate).9 13 (42%) patients were classified as mild, and 18 (58%) patients were classified as moderately severe.
Oxygen saturation of patients was also assessed by pulse oximetry at the time of admission. The control group included 39 age-matched healthy children recruited during routine follow-up at pediatric outpatient clinics who had no signs of septicemia, pulmonary, metabolic, rheumatologic, or autoimmune diseases.
The study was approved by local ethics committee (December 13, 2011, No. 5,172).
SamplesSerum samples collected from patients and control group were immediately separated from the cells by centrifugation at 3,000g for 10min, and then stored at −80°C until further analysis of TOS, TAC, and OSI.
Measurement of total antioxidant statusTotal oxidant status (TOS) was measured with the assay based on the oxidation of ferrous ion to ferric ion in the presence of various oxidant species in acidic medium, and the measurement of ferric ion by xylenol orange. The assay was calibrated with hydrogen peroxide, and the results were expressed in terms of micromolar hydrogen peroxide equivalents per liter (μmol H2O2 eqv/L).10
Measurement of TAC of plasmaTAC was measured through a method developed by Erel.11 In this method, the antioxidative effect of the sample against potent free radical reactions that are initiated by the hydroxyl radical produced are measured. The results are expressed as μmol Trolox eqv/L.
Measurement of plasma oxidative stress indexOxidative stress index (OSI) was determined by the ratio of TOS to TAC.12
OSI (arbitrary unit)=TOS (μmol H2O2 eqv/L)/TAC (μmol Trolox eqv/L).
Statistical analysisThe statistical analysis was performed using the Statistical Package for Social Sciences (SPSS) 15.0 for Windows. Student's t-test was used for comparing mean values of age among acute bronchiolitis and control groups. Plasma TAC, TOS, and OSI levels were compared with one-way ANOVA test among mild bronchiolitis, moderate bronchiolitis, and control subjects. Multiple comparisons were analysed through Tukey's HSD post hoc test. Correlation analysis was performed between oxygen saturation and oxidative state.
ResultsThe male to female ratio was 1.2 in patients with bronchiolitis (17 male and 14 female) and 0.94 in the control group (18 male and 19 female) (p=0.61). Mean ages of patients with bronchiolitis and the control group were 9.93±3.96 and 9.83±4.51, respectively (p=0.92). Total oxidative status was higher in patients with bronchiolitis than the control group (5.16±1.99μmol H2O2 eqv/L versus 3.78±1.78μmol H2O2 eqv/L [p=0.004]). Total antioxidant capacity was significantly lower in children with acute bronchiolitis than the control group (2.51±0.37μmol Trolox eqv/L versus 2.75±0.39μmol Trolox eqv/L [p=0.013]). Oxidative stress index of patients with bronchiolitis was higher than control group, but the difference was not statistically significant (0.20±0.88 units versus 0.15±0.12 units [p=0.085]).
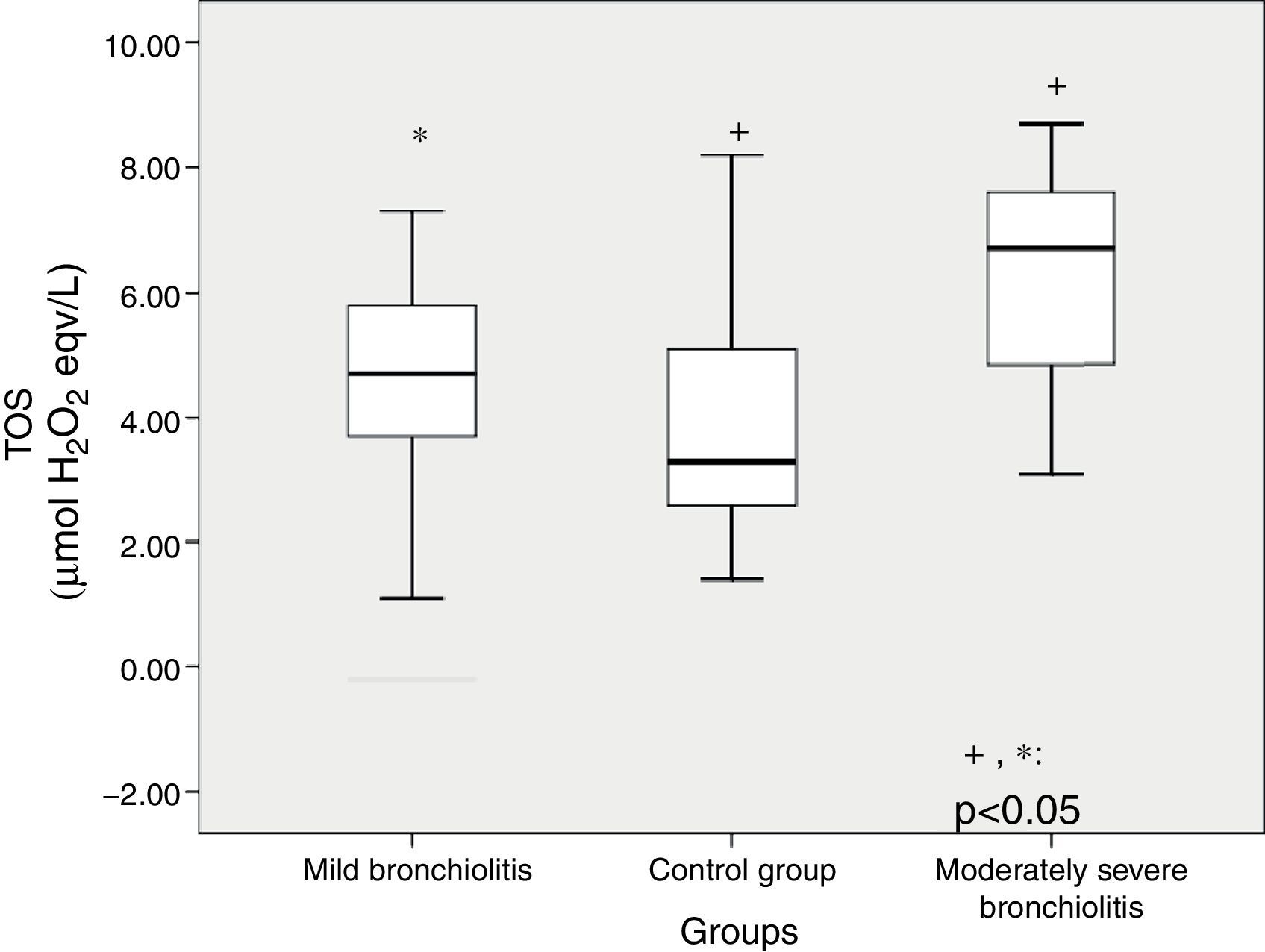
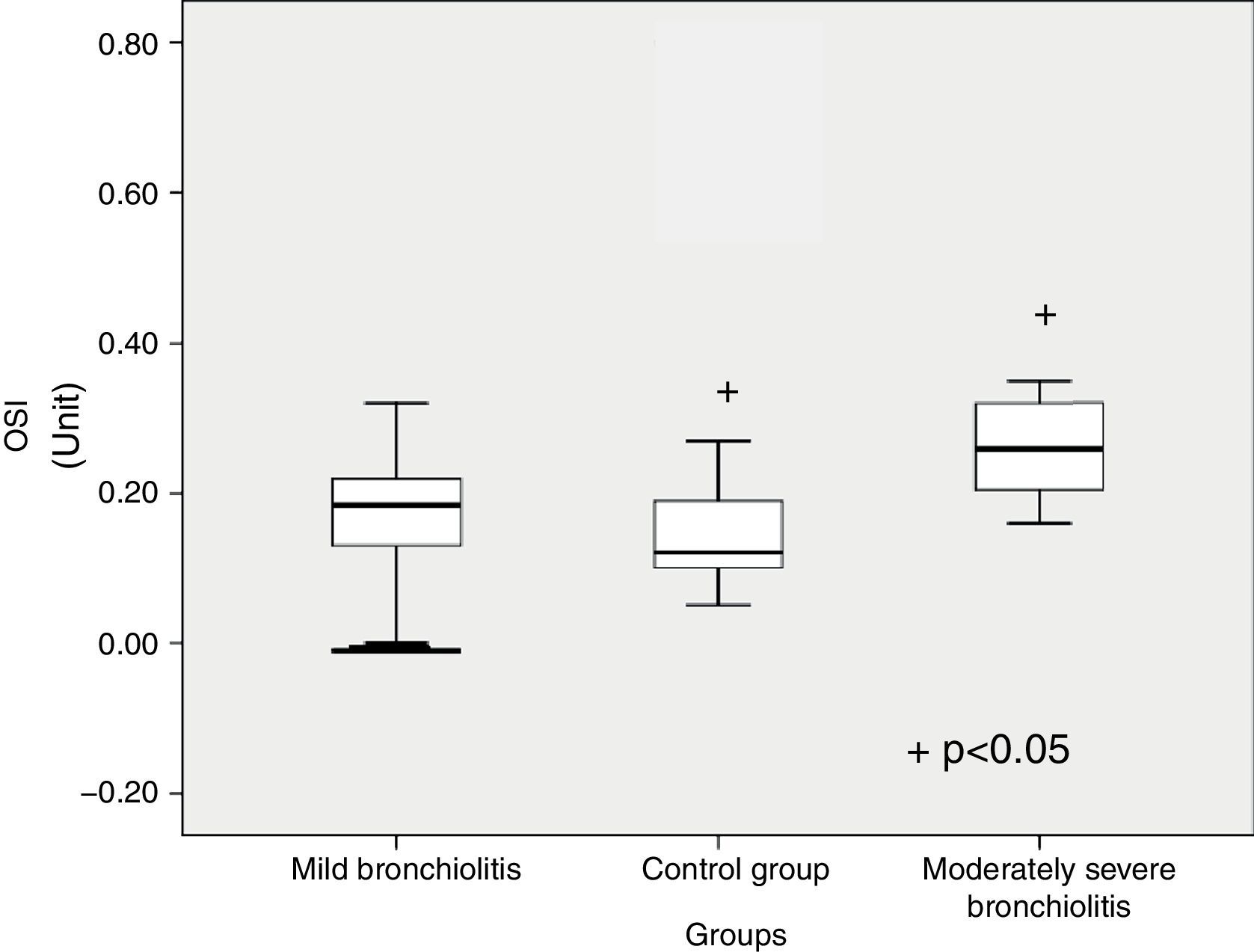
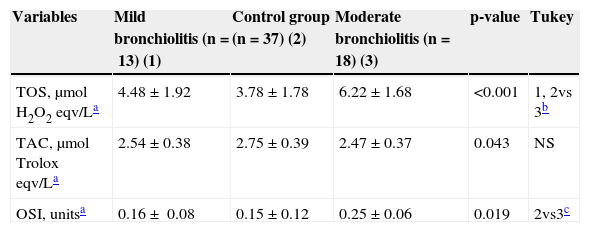
TOS level significantly differed between subgroups (p<0.001) (Table 1). Patients with moderate bronchiolitis had higher TOS levels than mild bronchiolitis and control group (p=0.03, p<0.001, respectively) (Fig. 1). Although the TAC level was higher in patients with moderate bronchiolitis than in those with mild bronchiolitis and the control group, there was not a significant difference (p=0.88, p=0.08, respectively). OSI was significantly different between subgroups (p=0.019) (Fig. 2). Patients with moderate bronchiolitis had higher OSI levels than the control group (p=0.015).
Comparisons of demographic characteristics and oxidative and antioxidative parameters among mild bronchiolitis, moderate bronchiolitis, and control group.
| Variables | Mild bronchiolitis (n=13) (1) | Control group (n=37) (2) | Moderate bronchiolitis (n=18) (3) | p-value | Tukey |
|---|---|---|---|---|---|
| TOS, μmol H2O2 eqv/La | 4.48±1.92 | 3.78±1.78 | 6.22±1.68 | <0.001 | 1, 2vs 3b |
| TAC, μmol Trolox eqv/La | 2.54±0.38 | 2.75±0.39 | 2.47±0.37 | 0.043 | NS |
| OSI, unitsa | 0.16± 0.08 | 0.15±0.12 | 0.25±0.06 | 0.019 | 2vs3c |
OSI, oxidative stress index; TAC, total antioxidant capacity; TOS, total oxidative status.
Oxygen saturation level of bronchiolitis patients was inversely correlated with TOS (r=−0.476, p<0.05) (Fig. 3).
DiscussionOxidative stress can contribute to the pathogenesis of several lung diseases in children, such as asthma, cystic fibrosis, and chronic neonatal lung disease.3,4,13–15 Increased oxidative stress has also been found in infants and preschool children passively exposed to tobacco smoke.16,17 Infections with viruses such as HIV, hepatitis B, influenza, and rhinovirus have been shown to stimulate ROS generation.18 In this study, the oxidative state of children during acute bronchiolitis, which is a common illness during childhood, was evaluated. To the best of the authors’ knowledge, there are no published reports on serum oxidative/antioxidative markers of TAC, TOS, and OSI in children with acute bronchiolitis. Various antioxidants in plasma have an additive effect, protecting the organism from free radicals.19 In this respect, measurement of TAC provides information about the antioxidant capacity of the organism.11 In addition, OSI, the ratio of total plasma TOS level to TAC, is an indicator of oxidative stress, reflecting the redox balance between oxidation and antioxidation.10,12 The present study demonstrated that TAC was lower in patients with acute bronchiolitis than the control group. TOS and OSI were increased in moderate bronchiolitis patients in comparison with the control group.
Reduction in antioxidant enzyme (AOE) expression has been observed in the lungs of mice previously infected with respiratory syncytial virus (RSV) and human metapneumovirus (hMPV).20,21 Impairment or decrease in the expression and/or activity of superoxide dismutase (SOD), catalase, glutathione S-tranferase, and glutathione peroxidase have been shown in nasopharyngeal secretions of children with severe RSV bronchiolitis.5 Recently, Mallol et al. measured the oxidant and antioxidant activity in bronchoalveolar fluid of 21 children with post-infectious bronchiolitis obliterans.22 They found an increased level of oxidative stress markers with a differential activity of antioxidant enzyme levels (normal catalase and increased glutathione peroxidase). Despite the marked airway narrowing found in all patients, their pulmonary function parameters were unrelated to oxidative stress markers suggesting that OS could be more related to airway inflammation and airway hyperresponsiveness (AHR) than to airway calibre.
The present study also investigated whether oxidative stress could play a role in bronchiolitis severity. TOS was increased in moderate bronchiolitis in comparison to mild cases. An increase in OSI was also significant in moderate bronchiolitis. Oxygen saturation levels of patients were inversely correlated with TOS. Zeyrek et al. investigated the association of oxidative stress with DNA damage in 42 children with asthma bronchiale.23 Plasma TAC, TOS, and total peroxide concentrations (LOOH) were higher in patients than in healthy controls, and DNA damage correlated with increased TOS.
Antioxidant treatment blocks transcription factor activation and chemokine gene expression in vitro.24,25 Castro et al. showed that antioxidant treatment reduced RSV-induced clinical illness and body weight loss in experimentally infected mice.20 In an animal model of influenza infection, inhibition of oxygen radicals through administration of antioxidants or increased lung superoxide dismutase levels significantly reduced lung injury and improved the survival rate of infected animals, suggesting that oxidative stress can play a significant role in the pathogenesis of viral pneumonia.26,27 Gurkan et al. investigated the relationship between serum malondialdehyde (MDA) and selenium (Se) levels and the occurrence and severity of acute bronchiolitis in children.28 Children with acute bronchiolitis showed increased MDA levels and impaired Se status in comparison to control subjects. They concluded that antioxidant supplementation with Se might provide a beneficial effect against bronchiolitis.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Dundaroz R, Erenberk U, Turel O, Demir AD, Ozkaya E, Erel O. Oxidative and antioxidative status of children with acute bronchiolitis. J Pediatr (Rio J). 2013;89:407–11.