To investigate ApoB/ApoA1 ratio and its association with cardiovascular risk factors in children.
MethodsCross-sectional study with 258 children aged 8 and 9 years old, enrolled in all urban schools in the city of Viçosa-MG. Anthropometric and body composition assessment, as well as biochemical profile of the children was performed. Socioeconomic variables and sedentary lifestyle were evaluated through a semi-structured questionnaire.
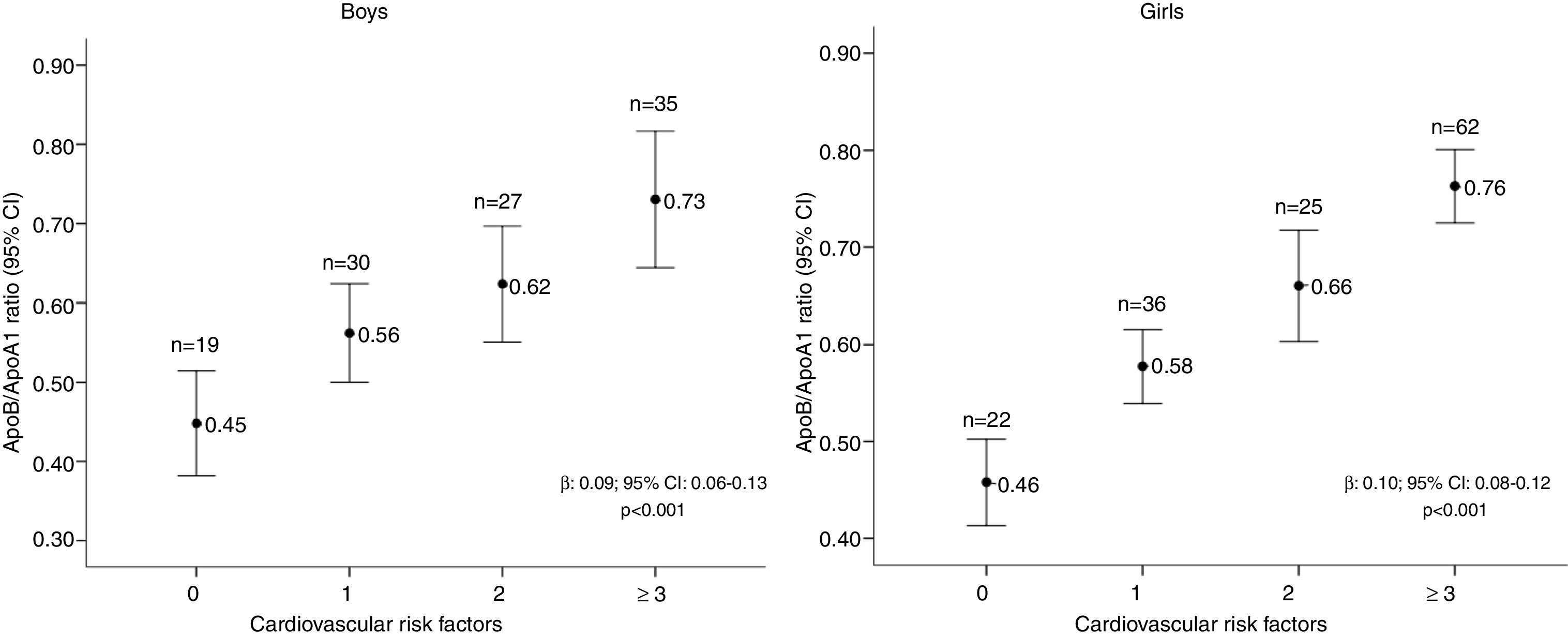
ResultsMany children had excess weight (35.2%), abdominal adiposity (10.5%), and body fat (15.6%), as well as increased ApoB/ApoA1 ratio (14.7%), total cholesterol (51.8%), and triglycerides (19.8%). Children with excess weight and total and central fat had a higher prevalence of having a higher ApoB/ApoA1 ratio, as well as those with atherogenic lipid profile (increased LDL-c and triglycerides and low HDL-c). A direct association was found between the number of cardiovascular risk factors and the ApoB/ApoA1 ratio (p=0.001), regardless of age and income.
ConclusionThe increased ApoB/ApoA1 ratio was associated with excess weight, body adiposity (total and central), and altered lipid profile in children. Children with a higher number of cardiovascular risk factors had higher ApoB/ApoA1 ratio, in both genders.
Investigar a razão ApoB/ApoA1 e sua relação com fatores de risco cardiovascular em crianças.
MétodosEstudo transversal com 258 crianças de 8 e 9 anos, matriculadas em todas as escolas urbanas de Viçosa-MG. Foi feita avaliação antropométrica, da composição corporal e bioquímica das crianças. As variáveis socioeconômicas e o sedentarismo foram avaliados por questionário semiestruturado.
ResultadosMuitas crianças apresentaram excesso de peso (35,2%), de adiposidade abdominal (10,5%) e de gordura corporal (15,6%), bem como a razão ApoB/ApoA1 (14,7%), colesterol-total (51,8%) e triglicerídeos (19,8%) aumentados. Crianças com excesso de peso e de gordura total e central apresentaram maiores prevalências de maior razão ApoB/ApoA1, bem como as com perfil lipídico aterogênico (LDL-c e triglicerídeos aumentados e baixo HDL-c). Foi encontrada associação direta entre o número de fatores de risco cardiovascular e a razão ApoB/ApoA1 (p=0,001), independente da idade e renda.
ConclusãoA razão ApoB/ApoA1 aumentada esteve associada ao excesso de peso, de adiposidade corporal (total e central) e ao perfil lipídico alterado nas crianças. As crianças com maior número de fatores de risco cardiovascular apresentaram maior razão ApoB/ApoA1, em ambos os sexos.
Exposure to the atherogenic lipid profile may induce changes in the arteries and contribute to atherosclerosis development, which may start in childhood.1 Studies have shown that elevated LDL cholesterol levels in children predict an increase in the intima-media layer thickness of the arteries in adults.2 Considering this fact, it is important to measure serum lipid levels in childhood as a strategy aimed to prevent cardiovascular diseases and atherosclerosis.
The ratio between pro-atherogenic (containing ApoB) and anti-atherogenic particles (containing ApoA1) may be associated with cardiovascular diseases.3 ApoA1 is the main protein of the HDL-c particle, responsible for stimulating reverse cholesterol transport, removing excess from the tissues and redirecting it to the liver. Moreover, it can inhibit LDL-c oxidation, helps in the removal of toxic products, and it has anti-inflammatory properties.4 In turn, ApoB is part of the atherogenic lipid fractions, including LDL-c, an intermediate-density lipoprotein (IDL), very low-density lipoprotein (VLDL), and lipoprotein (a).5
Thus, the ApoB/ApoA1 ratio has been investigated as a possible cardiometabolic predictor for atherosclerosis in adults.6 In children, studies have shown that the ApoB/ApoA1 ratio is associated with metabolic syndrome components, such as increased waist circumference and blood pressure, low HDL-c, and high triglycerides.7,8 Additionally, lifestyle changes in obese children, such as sedentary lifestyle, seem to influence the higher ApoB/ApoA1 ratio.9
However, there is a gap in the knowledge on the association between the ApoB/ApoA1 ratio and cardiovascular risk factors in children, with this subject being scarcely studied in Brazil10 and in other countries in this age group.7,8
As the increased ApoB/ApoA1 ratio may contribute to the occurrence of atherosclerotic events in adult life, the aim of this study was to investigate the ApoB/ApoA1 ratio and its association with cardiovascular risk factors in children enrolled in urban schools in the municipality of Viçosa, state of Minas Gerais, Brazil.
MethodsStudy population and sampling processThis is a cross-sectional study conducted between May and December of 2015, with a sample of 258 children aged 8 and 9 years, enrolled in all public (n=17) and private (n=7) schools in the urban area of the municipality of Viçosa, Minas Gerais, Brazil. This study is part of a larger project entitled “Vitamin D in childhood: intake, serum levels, and association with cardiovascular risk factors,” from the Schoolchildren's Health Assessment Survey (Pesquisa de Avaliação da Saúde do Escolar – PASE).
The sample was calculated using the OpenEpi statistical program (Open Source Epidemiologic Statistics for Public Health, version 3.01), considering the prevalence of 50% for multiple outcomes, tolerable error of 5%, plus 10% losses and 10% confounding factors, totaling a sample size of 366 children.
For the evaluation of the ApoB/ApoA1 ratio, a subsample of 258 children was used, since the blood volume collected was not enough for the ApoB and ApoA1 measurement in all the children from the original project. It is worth mentioning that the final sample did not differ from the original sample in relation to gender, age, and cardiovascular risk factors.
A stratified random sampling process was performed on the schoolchildren, in which the number of children to be sampled in each school was related to the weighting by school, according to its size. Subsequently, the children were selected by drawing lots from a random number table, until the number of students needed per school was completed.
After contacting the parents, the children were invited to participate in the study. Those who used medications that interfered with glucose and/or lipid metabolism were not included in the study.
Data collectionWeight and height were measured using an electronic digital scale (Tanita®, model BC 553, IL, USA), with a capacity of 150 kilograms and a sensitivity of 100 grams. Weight was measured with the individuals in the orthostatic position, barefoot, and wearing light clothing. Height was measured using a portable vertical stadiometer (Alturexata®, MG, Brazil), measuring 2 meters, graduated in centimeters and subdivided into millimeters. Body mass index (BMI) was calculated based on the obtained values. Nutritional status was evaluated based on BMI/age, and children with z-score ≥−2 and <1 were considered as having normal weight, whereas those with z-score ≥1 were considered as having excess weight (overweight or obesity).11
Waist circumference (WC) was measured at the midpoint between the iliac crest and the last rib using a flexible, inelastic measuring tape, graduated in centimeters and subdivided into millimeters. Excessive abdominal adiposity was considered in the presence of values above the 90th percentile according to age and gender.12 The waist-to-height ratio (WHtR) was calculated by dividing the waist measurement (cm) by height (cm), and values ≥ 0.5 were used to classify excess abdominal adiposity.13
The total and central body fat (android fat [AF] and gynoid fat [GF]) was evaluated in the supine position, using the dual-energy X-ray absorptiometry (DXA) method in the Diagnostic Imaging Sector of the Health Division of Universidade Federal de Viçosa. The AF comprises the region between the ribs and the pelvis, with the upper marking being made at 20% of the distance from the iliac crest and neck, and the lower marking being made above the pelvis. The gynoid region measurements included the hip, thighs, and overlaps of the leg and trunk regions, with the upper marking being made below the iliac crest at a distance of 1.5 times the android height.14 Excess body fat was classified with values ≥85th percentile for age and gender, according to McCarthy et al.15
The neck circumference (NC) was assessed in the Frankfurt horizontal plane, with the child standing erect, using an inextensible measuring tape (TBW®, SP, Brazil), just below the laryngeal prominence in the neck, perpendicular to the largest axis of the neck. Minimal pressure was exerted to allow full contact of the tape with the skin. The increased values were classified according to the cutoff points proposed by Nafieu et al.16
Waist circumference (WC), waist-to-height ratio (WHtR), neck circumference, and android/gynoid fat ratio were considered indicators of central adiposity, whereas BMI was the indicator of total adiposity.
Blood pressure (BP) was measured three times, with the child in the sitting position with five-minute intervals, considering the mean value for BP classification according to the 7th Brazilian Guideline of Arterial Hypertension. High blood pressure was classified as systolic (SBP) and/or diastolic (DBP) blood pressure above the 95th percentile, according to age, gender, height percentile, on at least three different occasions.17 BP was measured using the automatic device (Omron®, HEM 907, IL, USA).
Venous blood samples were collected between eight and ten a.m., after overnight fasting, and centrifuged at 1000×g for 10min at 4°C. Levels of total cholesterol (TC), HDL-c, LDL-c, triglycerides (TG), and C-reactive protein (CRP) were measured using the colorimetric enzymatic method using a commercial kit (Bioclin®, MG, Brazil) in an automated analyzer (BS-200 Mindray®, China) at the Laboratory of Clinical Analyses (LAC) of the Nutrition and Health Department of Universidade Federal de Viçosa (UFV). Non-HDL-cholesterol was estimated by the formula: Non-HDL-c=TC-HDL-c. The lipid profile classification was performed according to the Brazilian Society of Cardiology.18 The serum levels of leptin, ApoA1, ApoB and homocysteine were analyzed through commercial ELISA kits, nephelometry (Beckman Coulter, CA, USA), and chemiluminescence (standardized protocols from Diagnóstico Brasil), respectively. Intra-assay variations were 4% for both ApoA1 and ApoB. Because there were no cutoff points for the classification of the ultra-sensitive C-reactive protein, leptin, homocysteine, ApoA1 and ApoB in the studied age group, values ≥85th percentile were considered at risk.
A semi-structured questionnaire was applied personally by trained interviewers to parents or guardians to assess sociodemographic variables, such as gender and family income per capita, and total time of physical activity (TPA). The children were classified as active when they performed 300minutes or more of moderate or vigorous physical activity weekly and were considered inactive when they performed less than 300minutes, as classified by the National School Health Survey.19 It is important to mention that none of the girls had experienced menarche at the time of this study.
Statistical analysisThe normality of the data was verified by the Kolmogorov–Smirnov test. Pearson's chi-squared test and Fisher's exact test were used to compare the prevalence of cardiovascular risk factors between genders and ApoB/ApoA1 values.
Poisson regression was performed with crude and adjusted robust variance to analyze the associations between ApoB/ApoA1 ratio and age, time of physical activity, anthropometric variables, body composition, and clinical and biochemical variables. Variables with a significance level ≤0.20 were included in the regression model. According with the linear regression analysis, the ApoB/ApoA1 ratio was also evaluated according to the number of cardiovascular risk factors (TPA, WHtR, CT, HDL-c, LDL-c, TG, non-HDL cholesterol, AF/GF, excess weight). Statistical analyses were performed using the software SPSS® (SPSS for Windows, Version 16.0., Chicago, USA) and Stata (Stata Statistical Software: Release 10, College Station, TX, USA). Values of p<0.05 were considered statistically significant.
Ethical aspectsThis study was carried out in accordance with the guidelines defined in the Declaration of Helsinki and all procedures involving human subjects were approved by the Human Research Ethics Committee of Universidade Federal de Viçosa (UFV; Opinion No. 663.171/2014). Informed consent was obtained from all parents or legal guardians, after they were informed about the study objectives.
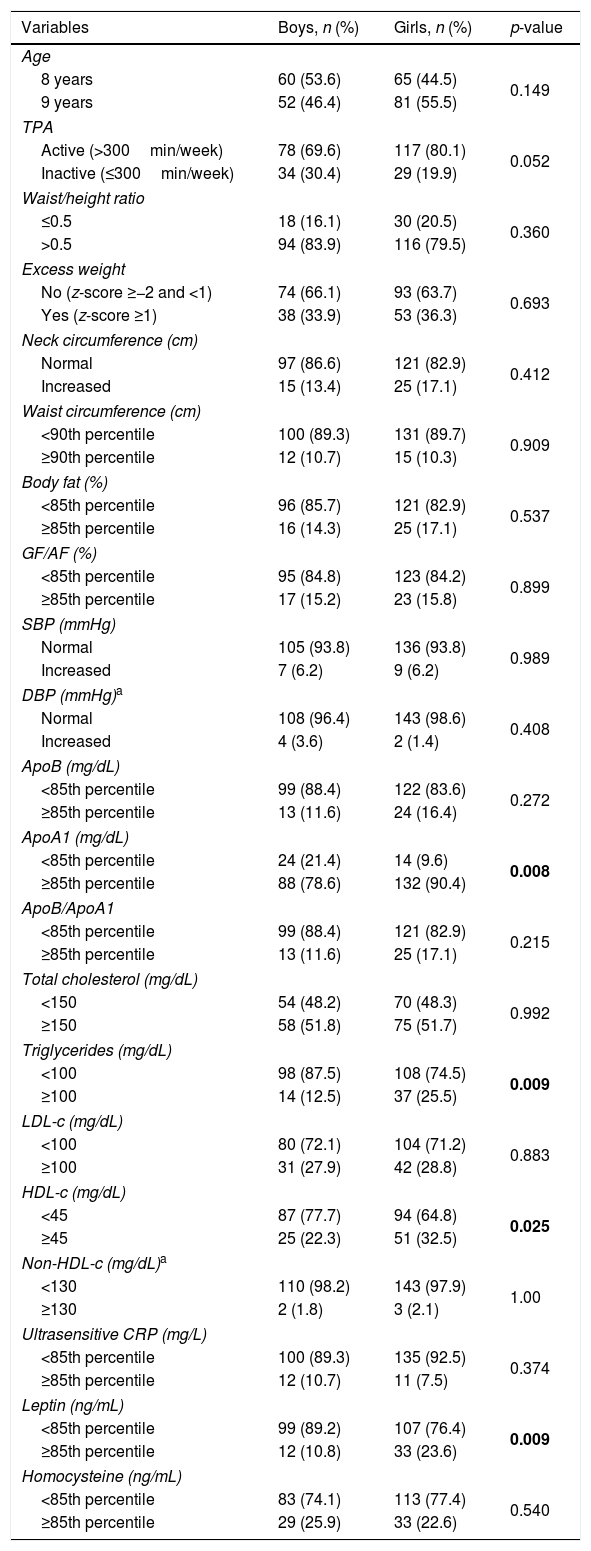
ResultsA total of 258 children were evaluated, 56% females. Many children had excess weight (35.2%), abdominal adiposity (10.5%), and body fat (15.6%), as well as increased ApoB/ApoA1 ratio (14.7%), serum levels of total cholesterol (51.8%), and triglycerides (19.8%). Additionally, 8.9%, 17.9%, and 24% of the children had increased serum levels of ultrasensitive CRP, leptin, and homocysteine, respectively. The prevalence of reduced serum ApoA1 and HDL-c levels was higher in boys than in girls. In turn, girls had a higher prevalence of increased serum levels of triglycerides and leptin (Table 1).
Distribution of the children's age, physical activity time, anthropometric, body composition, and biochemical variables, according to gender; Viçosa, MG, Brazil, 2015.
| Variables | Boys, n (%) | Girls, n (%) | p-value |
|---|---|---|---|
| Age | |||
| 8 years | 60 (53.6) | 65 (44.5) | 0.149 |
| 9 years | 52 (46.4) | 81 (55.5) | |
| TPA | |||
| Active (>300min/week) | 78 (69.6) | 117 (80.1) | 0.052 |
| Inactive (≤300min/week) | 34 (30.4) | 29 (19.9) | |
| Waist/height ratio | |||
| ≤0.5 | 18 (16.1) | 30 (20.5) | 0.360 |
| >0.5 | 94 (83.9) | 116 (79.5) | |
| Excess weight | |||
| No (z-score ≥−2 and <1) | 74 (66.1) | 93 (63.7) | 0.693 |
| Yes (z-score ≥1) | 38 (33.9) | 53 (36.3) | |
| Neck circumference (cm) | |||
| Normal | 97 (86.6) | 121 (82.9) | 0.412 |
| Increased | 15 (13.4) | 25 (17.1) | |
| Waist circumference (cm) | |||
| <90th percentile | 100 (89.3) | 131 (89.7) | 0.909 |
| ≥90th percentile | 12 (10.7) | 15 (10.3) | |
| Body fat (%) | |||
| <85th percentile | 96 (85.7) | 121 (82.9) | 0.537 |
| ≥85th percentile | 16 (14.3) | 25 (17.1) | |
| GF/AF (%) | |||
| <85th percentile | 95 (84.8) | 123 (84.2) | 0.899 |
| ≥85th percentile | 17 (15.2) | 23 (15.8) | |
| SBP (mmHg) | |||
| Normal | 105 (93.8) | 136 (93.8) | 0.989 |
| Increased | 7 (6.2) | 9 (6.2) | |
| DBP (mmHg)a | |||
| Normal | 108 (96.4) | 143 (98.6) | 0.408 |
| Increased | 4 (3.6) | 2 (1.4) | |
| ApoB (mg/dL) | |||
| <85th percentile | 99 (88.4) | 122 (83.6) | 0.272 |
| ≥85th percentile | 13 (11.6) | 24 (16.4) | |
| ApoA1 (mg/dL) | |||
| <85th percentile | 24 (21.4) | 14 (9.6) | 0.008 |
| ≥85th percentile | 88 (78.6) | 132 (90.4) | |
| ApoB/ApoA1 | |||
| <85th percentile | 99 (88.4) | 121 (82.9) | 0.215 |
| ≥85th percentile | 13 (11.6) | 25 (17.1) | |
| Total cholesterol (mg/dL) | |||
| <150 | 54 (48.2) | 70 (48.3) | 0.992 |
| ≥150 | 58 (51.8) | 75 (51.7) | |
| Triglycerides (mg/dL) | |||
| <100 | 98 (87.5) | 108 (74.5) | 0.009 |
| ≥100 | 14 (12.5) | 37 (25.5) | |
| LDL-c (mg/dL) | |||
| <100 | 80 (72.1) | 104 (71.2) | 0.883 |
| ≥100 | 31 (27.9) | 42 (28.8) | |
| HDL-c (mg/dL) | |||
| <45 | 87 (77.7) | 94 (64.8) | 0.025 |
| ≥45 | 25 (22.3) | 51 (32.5) | |
| Non-HDL-c (mg/dL)a | |||
| <130 | 110 (98.2) | 143 (97.9) | 1.00 |
| ≥130 | 2 (1.8) | 3 (2.1) | |
| Ultrasensitive CRP (mg/L) | |||
| <85th percentile | 100 (89.3) | 135 (92.5) | 0.374 |
| ≥85th percentile | 12 (10.7) | 11 (7.5) | |
| Leptin (ng/mL) | |||
| <85th percentile | 99 (89.2) | 107 (76.4) | 0.009 |
| ≥85th percentile | 12 (10.8) | 33 (23.6) | |
| Homocysteine (ng/mL) | |||
| <85th percentile | 83 (74.1) | 113 (77.4) | 0.540 |
| ≥85th percentile | 29 (25.9) | 33 (22.6) | |
TPA, total time of physical activity; BMI, body mass index; GF, gynoid body fat; AF, android body fat; SBP, systolic blood pressure; DBP, diastolic blood pressure; ApoB, apolipoprotein B; ApoA1, apolipoprotein A1; LDL-c, low-density lipoprotein; HDL-c, high-density lipoprotein; CRP, C-reactive protein.
Pearson's chi-squared test.
Bold values represent p<0.05.
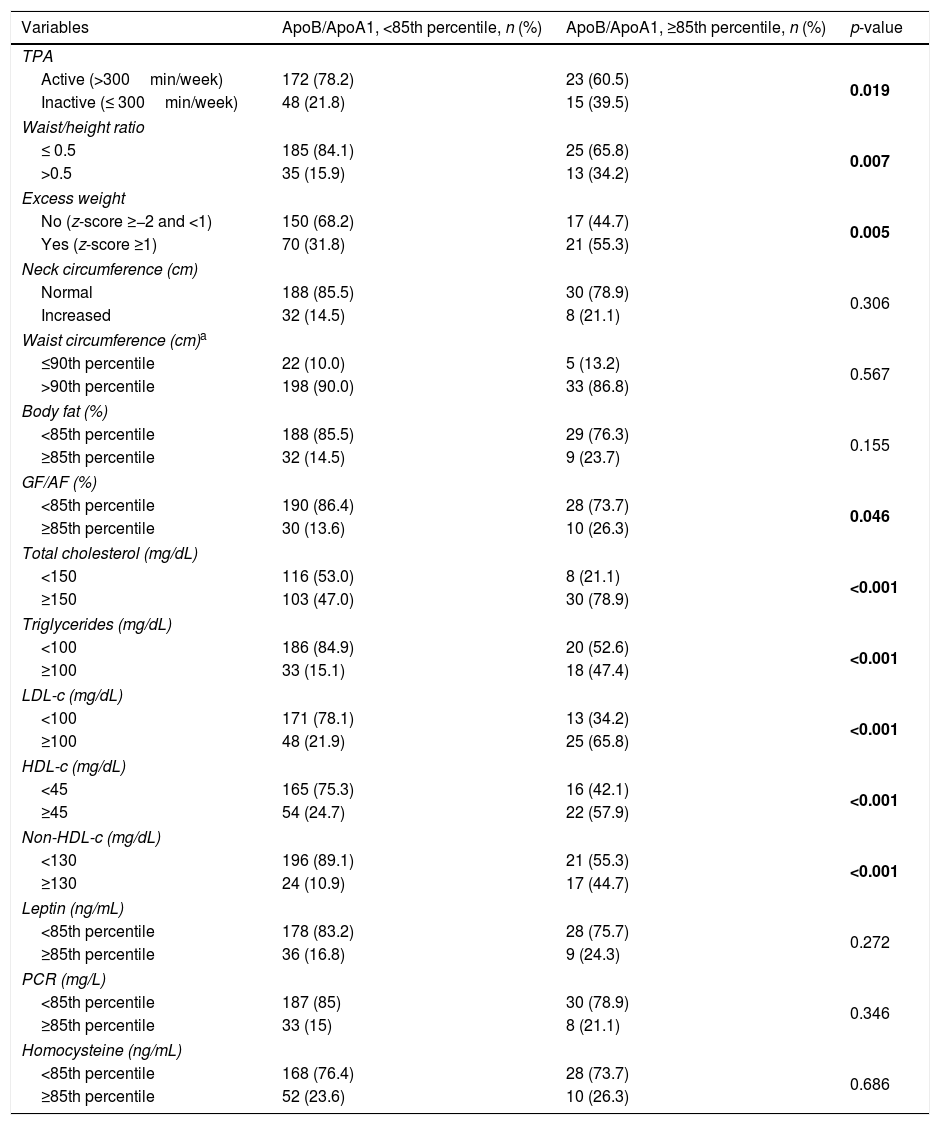
Children with a higher ApoB/ApoA1 ratio were more inactive, had increased WHtR, excess weight, and altered lipid profile (Table 2).
Distribution of children's physical activity time, anthropometric, body composition, and biochemistry variables, according to ApoB/ApoA1 ratio; Viçosa, MG, Brazil, 2015.
| Variables | ApoB/ApoA1, <85th percentile, n (%) | ApoB/ApoA1, ≥85th percentile, n (%) | p-value |
|---|---|---|---|
| TPA | |||
| Active (>300min/week) | 172 (78.2) | 23 (60.5) | 0.019 |
| Inactive (≤ 300min/week) | 48 (21.8) | 15 (39.5) | |
| Waist/height ratio | |||
| ≤ 0.5 | 185 (84.1) | 25 (65.8) | 0.007 |
| >0.5 | 35 (15.9) | 13 (34.2) | |
| Excess weight | |||
| No (z-score ≥−2 and <1) | 150 (68.2) | 17 (44.7) | 0.005 |
| Yes (z-score ≥1) | 70 (31.8) | 21 (55.3) | |
| Neck circumference (cm) | |||
| Normal | 188 (85.5) | 30 (78.9) | 0.306 |
| Increased | 32 (14.5) | 8 (21.1) | |
| Waist circumference (cm)a | |||
| ≤90th percentile | 22 (10.0) | 5 (13.2) | 0.567 |
| >90th percentile | 198 (90.0) | 33 (86.8) | |
| Body fat (%) | |||
| <85th percentile | 188 (85.5) | 29 (76.3) | 0.155 |
| ≥85th percentile | 32 (14.5) | 9 (23.7) | |
| GF/AF (%) | |||
| <85th percentile | 190 (86.4) | 28 (73.7) | 0.046 |
| ≥85th percentile | 30 (13.6) | 10 (26.3) | |
| Total cholesterol (mg/dL) | |||
| <150 | 116 (53.0) | 8 (21.1) | <0.001 |
| ≥150 | 103 (47.0) | 30 (78.9) | |
| Triglycerides (mg/dL) | |||
| <100 | 186 (84.9) | 20 (52.6) | <0.001 |
| ≥100 | 33 (15.1) | 18 (47.4) | |
| LDL-c (mg/dL) | |||
| <100 | 171 (78.1) | 13 (34.2) | <0.001 |
| ≥100 | 48 (21.9) | 25 (65.8) | |
| HDL-c (mg/dL) | |||
| <45 | 165 (75.3) | 16 (42.1) | <0.001 |
| ≥45 | 54 (24.7) | 22 (57.9) | |
| Non-HDL-c (mg/dL) | |||
| <130 | 196 (89.1) | 21 (55.3) | <0.001 |
| ≥130 | 24 (10.9) | 17 (44.7) | |
| Leptin (ng/mL) | |||
| <85th percentile | 178 (83.2) | 28 (75.7) | 0.272 |
| ≥85th percentile | 36 (16.8) | 9 (24.3) | |
| PCR (mg/L) | |||
| <85th percentile | 187 (85) | 30 (78.9) | 0.346 |
| ≥85th percentile | 33 (15) | 8 (21.1) | |
| Homocysteine (ng/mL) | |||
| <85th percentile | 168 (76.4) | 28 (73.7) | 0.686 |
| ≥85th percentile | 52 (23.6) | 10 (26.3) | |
TPA, total time of physical activity; BMI, body mass index; GF, gynoid body fat; AF, android body fat; SBP, systolic blood pressure; DBP, diastolic blood pressure; ApoB, apolipoprotein B; ApoA1, apolipoprotein A1; LDL-c, low-density lipoprotein; HDL-c, high-density lipoprotein; CRP, C-reactive protein.
Pearson's chi-squared test.
Bold values represent statistic significant values.
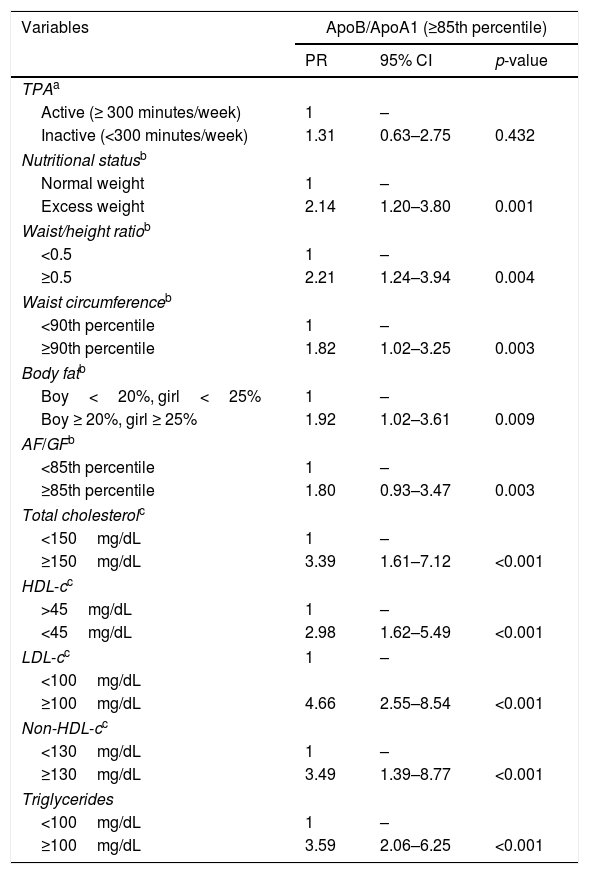
In regression models, children with excess of weight and indicators of total and central adiposity (WHtR, waist circumference, body fat, and AF/GF) had a higher prevalence of higher ApoB/ApoA1 ratio (≥85th percentile), regardless of gender, age, and income. Interestingly, children with an atherogenic lipid profile increased (total cholesterol, LDL-c, non-HDL-c, and triglycerides and low HDL-c) also had higher prevalence of a higher ApoB/ApoA 1 ratio, regardless of gender, age, income, and body fat (Table 3).
Association between the increased ApoB/ApoA1 ratio (dependent variable) and anthropometric, body composition, and biochemical variables in children; Viçosa, MG, Brazil, 2015.
| Variables | ApoB/ApoA1 (≥85th percentile) | ||
|---|---|---|---|
| PR | 95% CI | p-value | |
| TPAa | |||
| Active (≥ 300 minutes/week) | 1 | – | |
| Inactive (<300 minutes/week) | 1.31 | 0.63–2.75 | 0.432 |
| Nutritional statusb | |||
| Normal weight | 1 | – | |
| Excess weight | 2.14 | 1.20–3.80 | 0.001 |
| Waist/height ratiob | |||
| <0.5 | 1 | – | |
| ≥0.5 | 2.21 | 1.24–3.94 | 0.004 |
| Waist circumferenceb | |||
| <90th percentile | 1 | – | |
| ≥90th percentile | 1.82 | 1.02–3.25 | 0.003 |
| Body fatb | |||
| Boy<20%, girl<25% | 1 | – | |
| Boy ≥ 20%, girl ≥ 25% | 1.92 | 1.02–3.61 | 0.009 |
| AF/GFb | |||
| <85th percentile | 1 | – | |
| ≥85th percentile | 1.80 | 0.93–3.47 | 0.003 |
| Total cholesterolc | |||
| <150mg/dL | 1 | – | |
| ≥150mg/dL | 3.39 | 1.61–7.12 | <0.001 |
| HDL-cc | |||
| >45mg/dL | 1 | – | |
| <45mg/dL | 2.98 | 1.62–5.49 | <0.001 |
| LDL-cc | 1 | – | |
| <100mg/dL | |||
| ≥100mg/dL | 4.66 | 2.55–8.54 | <0.001 |
| Non-HDL-cc | |||
| <130mg/dL | 1 | – | |
| ≥130mg/dL | 3.49 | 1.39–8.77 | <0.001 |
| Triglycerides | |||
| <100mg/dL | 1 | – | |
| ≥100mg/dL | 3.59 | 2.06–6.25 | <0.001 |
TPA, time of physical activity; AF, android fat; GF, gynoid fat; HDL-c, high-density lipoprotein; BMI, body mass index; LDL-c, low density lipoprotein.
Adjusted Poisson regression:
Children with a higher number of cardiovascular risk factors had a higher ApoB/ApoA1 ratio, regardless of age and income, in both girls and boys (Fig. 1).
DiscussionIn the present study, a higher ApoB/ApoA1 ratio was associated with excess body weight and adiposity (total and central), as well as an altered lipid profile in children. There was a direct association between the number of cardiovascular risk factors and the ApoB/ApoA1 ratio, regardless of age and income.
In children and adolescents from Canada, an association was also found between the increased ApoB/ApoA1 ratio and excess weight.7 In a study carried out in the United States, children and adolescents with normal weight and abdominal obesity (WHtR≥0.5) had a higher number of cardiovascular risk factors, such as hypertension, increased levels of triglycerides, and LDL-c, as well as insulin resistance when compared to those without abdominal obesity.20 In Brazilian children and adolescents, the ApoB/ApoA1 ratio was associated with more than one cardiovascular risk factor (BMI, WC, WHtR, HDL-c, and triglycerides), corroborating the present findings.10
Excess central adiposity has been considered the main component of the metabolic syndrome and is strongly associated with dyslipidemia and an increase in the number of cardiovascular risk factors, both in adults21 and children.22 Excess central adiposity may lead to an increased ApoB/ApoA1 ratio through different mechanisms: (1) decreased hepatic LDL receptor and/or decreased lipoprotein lipase (LPL) activity, both important for the removal of remaining chylomicrons from the circulation containing ApoB molecules23,24; (2) increased adipokine secretion by adipose tissue in obese individuals; (3) reduction in serum HDL-c levels, the main characteristic of dyslipidemia associated with central obesity.25 In obese individuals, the low HDL-c level is a consequence of the increase in HDL-c catabolism, thus favoring a decrease in ApoA1 levels.26 Moreover, body fat accumulation is one of the main factors that can modify small-density LDL expression, because in both adults and children, abdominal obesity is associated with the lower density and the smaller particle size of LDL-c.27
It is worth mentioning that, in this study, children with three or more cardiovascular risk factors had higher ApoB/ApoA1 ratio values in both genders. This direct association suggests the possible influence of pro-atherogenic particles (containing ApoB) and anti-atherogenic particles (containing ApoA1) on cardiovascular diseases, as there is an increase in the number of risk factors. To date, no similar studies have been found, and thus, the results indicate the precocity of this association occurring as early as in childhood.
The present study showed no association between serum levels of leptin, CRP, and homocysteine with ApoB/ApoA1 ratio. One possible hypothesis is that these markers participate in the cardiometabolic risk through a pathway other than the ApoB/ApoA1 ratio, with these being recognized as important indicators of subclinical inflammation, while apolipoproteins are involved in lipid metabolism.28 However, to date, no other studies have been found that evaluated the association between a higher ApoB/ApoA1 ratio and these cardiometabolic markers, as well as the mechanisms involved.
One limitation of this study is the fact that it has a cross-sectional design, which does not allow for establishing cause-and-effect associations. It is important to emphasize that few Brazilian studies have evaluated non-classical cardiovascular markers, such as the ApoB/ApoA1 ratio, in healthy prepubertal children. As these alterations may contribute to the onset of atherosclerotic disease, early identification is crucial for the planning and implementation of public health policies, with actions directed at food and nutritional education and the stimulation of physical activity. These actions may contribute to reducing future mortality from cardiovascular diseases and other obesity-related diseases.
In summary, a higher ApoB/ApoA1 ratio was associated with excess weight, body adiposity (total and central), and altered lipid profile in children. Children with a higher number of cardiovascular risk factors had higher ApoB/ApoA1 ratio, regardless of age and income.
FundingConselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq – process n. 478910/2013-4).
Conflicts of interestThe authors declare no conflicts of interest.
The authors would like to thank the children and their parents for their participation in the study, to Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq – process No. 478910/2013-4) for the financial support, and for the HHM Hermsdorff's fellowship in Research Productivity, to Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) for the scholarships granted to graduate students, and to BioClin for the donation of kits for biochemical analyses.
Please cite this article as: Castro AP, Hermsdorff HH, Milagres LC, Albuquerque FM, Filgueiras MS, Rocha NP, et al. Increased ApoB/ApoA1 ratio is associated with excess weight, body adiposity, and altered lipid profile in children. J Pediatr. 2019;95:238–46.