To systematically revise the literature in search of data about the prevalence of constipation in patients with cystic fibrosis according to the publications in this field, which partly refer to guidelines defined in 2010 by the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition.
SourcesSystematic review selecting articles based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses, including Cystic Fibrosis patients of all ages. Sources of information were selected to identify the articles without period limitation: CADTH – Canadian Agency for Drugs and Technologies in Health, CINAHL Complete, Clinical Trials US NIH, Cochrane Library, Embase, MEDLINE via Ovid, Scopus, Web Of Science, PubMed, SciELO, MEDLINE and LILACS , Health Systems Evidence, PDQ Evidence, CRD Canadian Agency for Drugs and Technologies in Health, INAHTA – International Network of Agencies for Health Technology Assessment, and PEDro.
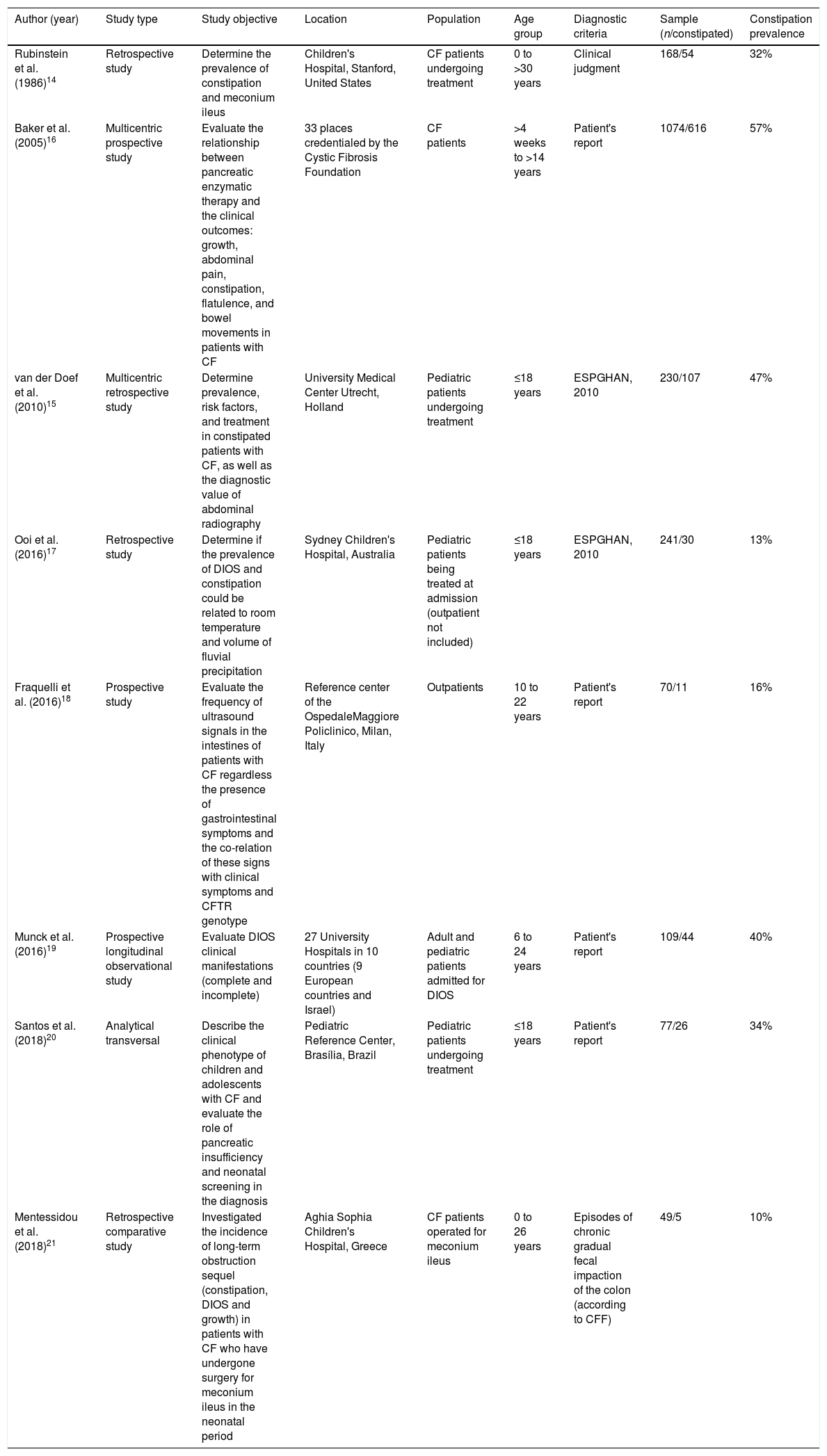
FindingsThe prevalence of constipation was reported in eight observational studies. Only two studies assessed the frequency of constipation as a primary objective; in the others, constipation was quoted along with the prevalence of the spectrum of gastrointestinal manifestations. Altogether, the publications included 2,018 patients, the reported prevalence varied from 10% to 57%. Only two of the six articles published after 2010 followed the definition recommended by the European Society.
ConclusionsConstipation is a frequent but still insufficiently assessed complaint of Cystic Fibrosis patients. The use of diverse diagnostic criteria restricts comparison and epidemiological conclusions, future studies should compulsorily apply the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition definition.
Revisar sistematicamente a literatura em busca de dados sobre a prevalência de constipação em pacientes com fibrose cística (FC), de acordo com as publicações nesse campo, que se referem parcialmente às diretrizes definidas pela European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN, 2010).
Fontes de dadosRevisão sistemática, selecionaram-se artigos com base no Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA), incluindo todos os pacientes com FC de todas as faixas etárias. As fontes de informação foram selecionadas para identificar os artigos sem limitação de período para a pesquisa: CADTH (Canadian Agency for Drugs and Technologies in Health), CINAHL Complete, Clinical Trials US NIH, Cochrane Library, Embase, Medline via Ovid, Scopus, Web of Science, PubMed, SciELO, Medline e Lilacs por meio da Biblioteca Virtual em Saúde (BVS), Health Systems Evidence, PDQ Evidence, CRD Canadian Agency for Drugs and Technologies in Health, INAHTA International Network of Agencies for Health Technology Assessment e PEDRO.
AchadosA prevalência de constipação em pacientes com FC foi relatada em oito estudos observacionais. Apenas dois estudos avaliaram a frequência de constipação como objetivo primário; nos outros, a constipação foi citada juntamente com a prevalência do espectro de manifestações gastrointestinais. No total, as publicações incluíram 2.018 pacientes e a prevalência relatada variou amplamente, de 10 a 57%. Apenas dois dos seis artigos publicados após 2010 seguiram a definição recomendada pela ESPGHAN.
ConclusõesA constipação é uma queixa frequente, mas ainda insuficientemente avaliada, dos pacientes com FC. O uso de diversos critérios diagnósticos restringe as comparações e declarações epidemiológicas, de modo que futuros estudos deveriam aplicar a definição ESPGHAN de maneira compulsória.
For many decades, pancreatic insufficiency – resulting in chronic diarrhea secondary to maldigestion and malabsorption of nutrients, and failure to thrive – was the focus of gastrointestinal manifestations in patients with cystic fibrosis (CF). With improved enzyme replacement therapy, the introduction of neonatal screening, and increased survival, other gastrointestinal (GI) manifestations deserve clinical and scientific attention. GI symptoms are frequent in patients with CF, as shown in a recent publication including a cohort of 131 patients with CF of all ages: with the use of a new CF-specific questionnaire (CFAbd-Score) for identification and quantification of the multi-organ abdominal complaints, 80% of the patients were found to have suffered abdominal pain and flatulence in the preceding three months. About 50% reported pain during evacuation and hard stools, and 30% were identified as constipated.1–3
Constipation was found to be prevalent in all reviews regarding gastrointestinal manifestations in patients with CF.4–11 Thus, the diagnosis of constipation was mentioned as requiring attention, as it either can be a single symptom or it may be an antecedent to development of the critical condition of a distal intestinal obstruction syndrome (DIOS).8,11 Because of the simultaneous occurrence of constipation and DIOS in patients with CF and their symptoms similarity, in 2010, the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) proposed a consensus definition for each of these morbidities. Constipation was defined as presence of pain and/or abdominal distention or decrease in spontaneous bowel movement frequency, or the increase in stool consistency lasting from a few weeks to months. Additionally, any of the mentioned symptoms should be relieved by the use of laxatives.12 The complete DIOS definition included (1) complete intestinal obstruction, recognized by vomiting of bilious material and/or abdominal radiography showing fluid in small intestine and (2) a fecal mass in the ileocaecum, and (3) abdominal pain or distension or both. Incomplete DIOS definition included (1) a short history (days) of abdominal pain or distension or both and (2) a fecal mass in the ileocaecum, absence of signs indicating intestinal obstruction.12
Despite the deductible importance of constipation in patients with CF, this matter has not received adequate attention, and systematically verified data about the prevalence, physiopathology, and treatment of this condition are scarce.9
The objective of this study was to systematically revise the literature in search for data about the prevalence of constipation in patients with CF, justifying the need to support professionals in the diagnostic decision-making and investigation during the assistance of these patients.
MethodsThis research involved a systematic review of the literature based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)13 with a careful selection of articles about the prevalence of constipation in patients with CF including all age groups.
Fifteen sources of information were selected to identify the articles, among databases and health information resources: CADTH – Canadian Agency for Drugs and Technologies in Health (https://www.cadth.ca/), CINAHL Complete (https://www.ebscohost.com/nursing/products/cinahl-databases/cinahl-complete), Clinical Trials US NIH – a service of the U.S. National Institutes of Health (https://clinicaltrials.gov/), Cochrane Library (https://www.cochranelibrary.com/), Embase (www.elsevier.com/embase), MEDLINE via Ovid (http://ovid.com/site/catalog/databases/901.jsp), Scopus (https://www.scopus.com/), Web Of Science (https://clarivate.com/products/web-of-science/), PubMed (http://www.pubmed.gov), SciELO (http://www.scielo.br/), MEDLINE and LILACS through the Biblioteca Virtual em Saúde (BVS) (https://bvsalud.org), Health Systems Evidence (https://www.healthsystemsevidence.org/), PDQ Evidence (https://www.pdq-evidence.org/pt), CRD Canadian Agency for Drugs and Technologies in Health (https://www.cadth.ca/), INAHTA – International Network of Agencies for Health Technology Assessment (http://www.inahta.org/), and PEDro (https://www.pedro.org.au/portuguese/). Before the beginning of the search, the existence of a systematic review in a similar subject was consulted in the Cochrane Library (https://www.cochranelibrary.com) database and no records were found.
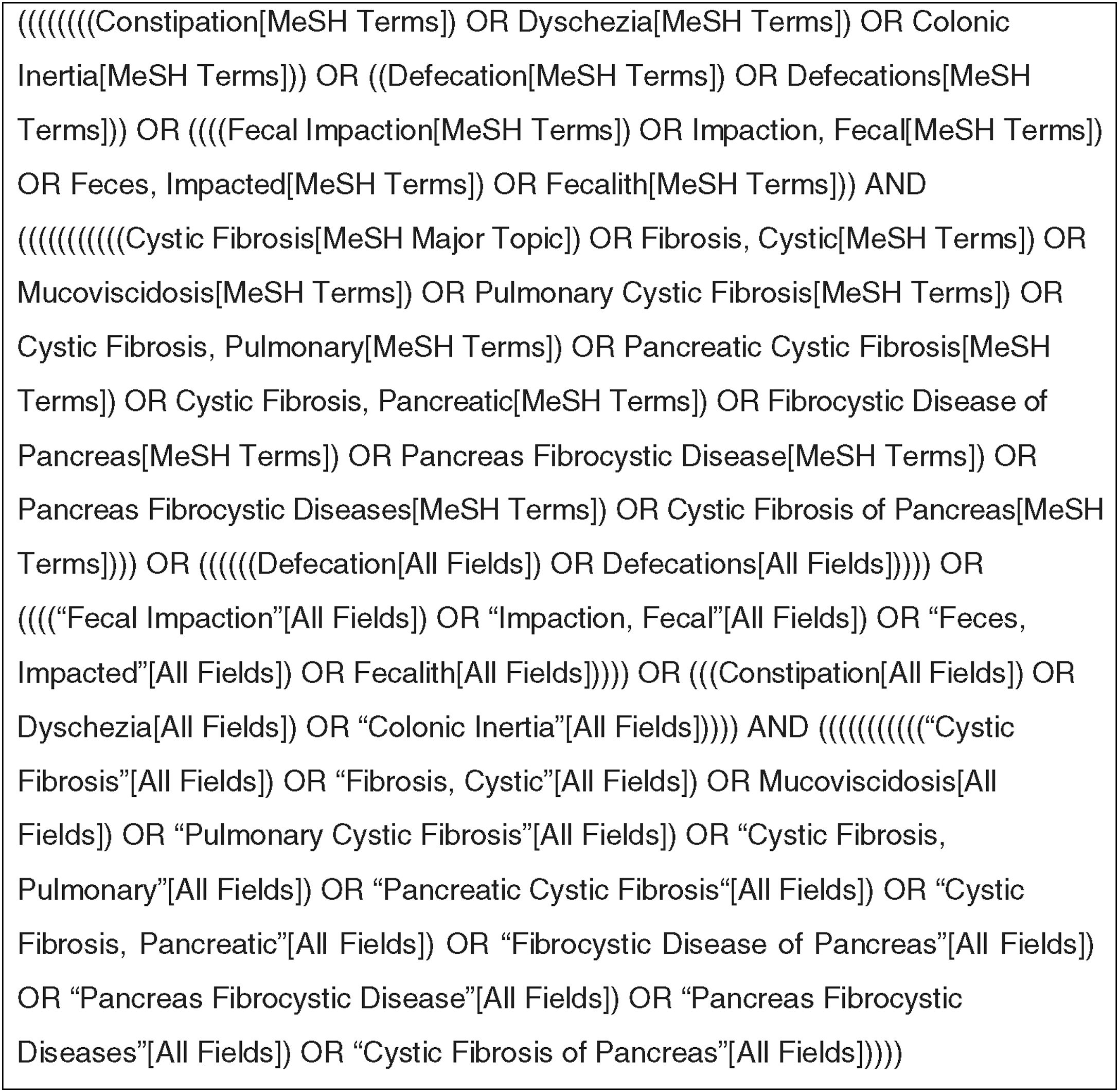
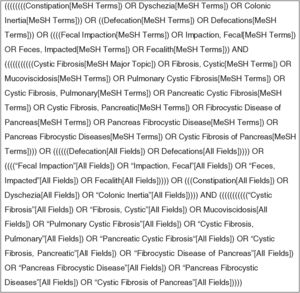
The descriptors used to elaborate the search strategies were defined by the Medical Subject Headings (MeSH), produced by the National Library of Medicine of the United States (https://www.ncbi.nlm.nih.gov/mesh) for publications in English and by the Descritores em Saúde (DeCS) (http://decs.bvs.br/) for publications in Portuguese. The selected descriptors were as follows: cystic fibrosis; constipation; defecation; fecal impaction – in English – and fibrose cística; constipação; defecação; impactação fecal – in Portuguese.
The search strategy for PubMed is described in Fig. 1. The search strategy was adapted to the other databases included in the research (Supplementary Material Appendix 1). There was no period limitation for the article search.
The inclusion criteria were patients with a CF diagnosis, and studies that reported constipation prevalence/incidence in patients from all age groups described in the literature.
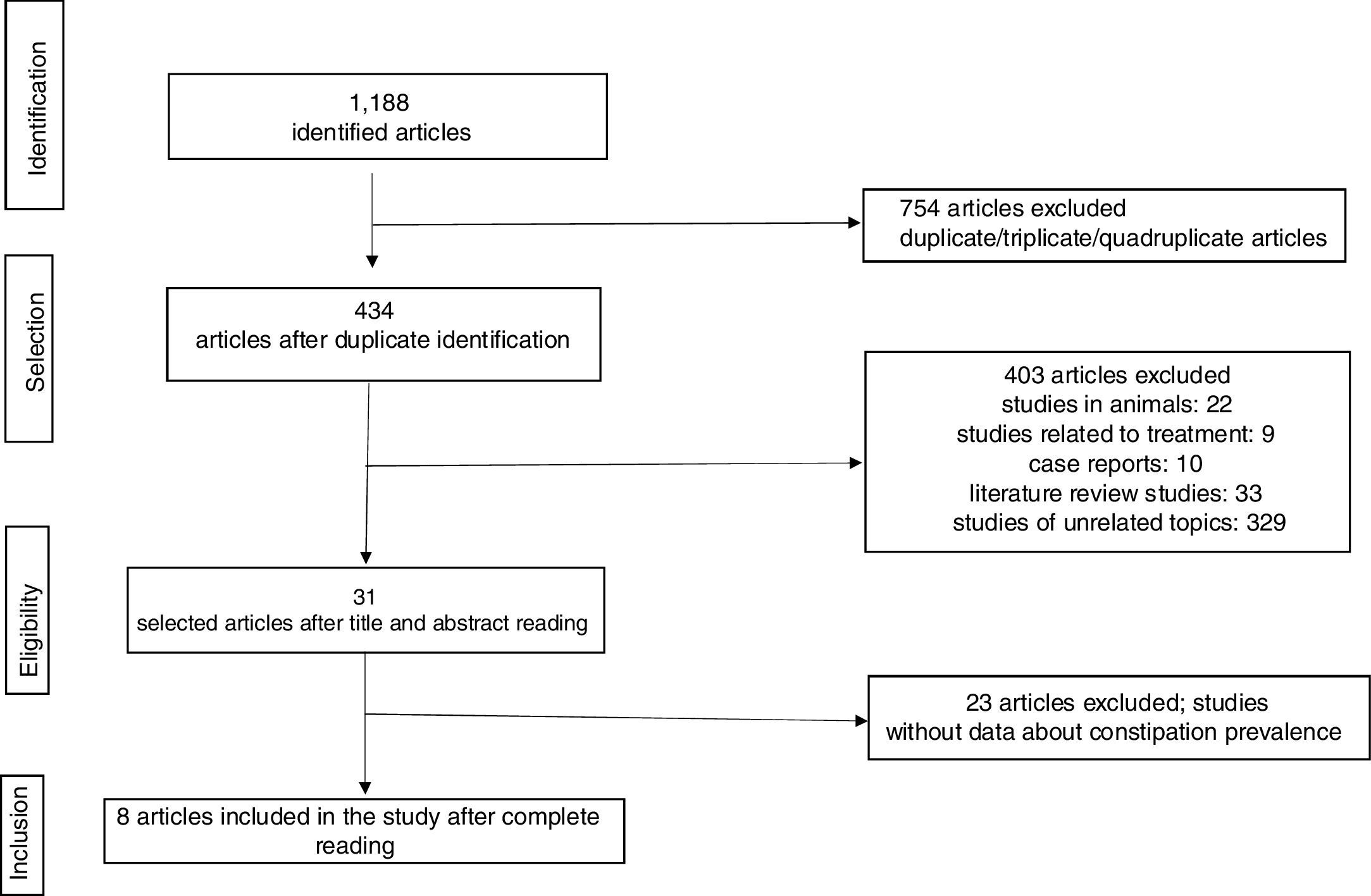
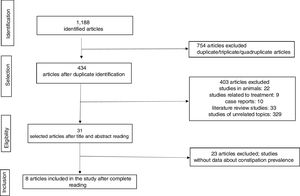
The article search was conducted from October 22nd to October 25th, 2018. In total, 1188 articles were identified. The selection of articles identified in the database was carried out in four stages and is detailed in Fig. 2.
In the initial stage, the article identification was conducted through searches combining the descriptor and the Boolean operators in the selected databases with posterior identification and exclusion of duplicated/triplicated/quadruplicated articles. The initial duplicate removal was conducted via End Note Web®, a reference manager program.
In the selection stage, the articles were excluded through the title and/or abstract based on the inclusion criteria previously mentioned. The titles and abstracts were read by two evaluators who determined their inclusion based on previously defined criteria.
Each evaluator independently opted for “inclusion” or “exclusion” and the discrepant results were evaluated by posterior consensus amongst the evaluators.
In the third stage, the articles considered eligible were selected for a complete read and posterior refinement of the selection. In the last stage, eight articles were included for the systematic review.
ResultsThe number of studies evaluated in every stage of the review is shown by the flowchart in Fig. 2
DiscussionData about constipation prevalence in CF patients were compiled in eight scientific publications. However, only two of these articles13,14 determined constipation prevalence as their main objective. In the other studies, constipation frequency was gathered along with the prevalence of other gastrointestinal manifestations. Abdominal symptoms were identified in cohorts including adults and children with CF, and also investigated in particular groups of CF patients, such as those with history of DIOS and meconium ileus. In the reports assessing different gastrointestinal complaints, constipation was considered relevant mainly for its main differential diagnoses: obstructive intestinal manifestations, including DIOS and acute fecal impaction.12,15–21
Currently, a high rate of severe abdominal conditions in CF patients deriving from pancreatic insufficiency are prevented and circumvented by the adequacy of the enzyme replacement therapy. Also, better attention to nutritional support and higher capacity to control the progression of the pulmonary disease contribute to reduction of abdominal complications. Therefore, the current scenario of CF patient care indicates the need to study co-morbidities that negatively interfere in the quality of life of patients.
In this review, most studies evaluated assessed the prevalence of symptomatic gastrointestinal manifestations in CF. No larger and/or multicentric clinical studies or clinical essays with the primary objective to systematically address constipation were identified.
ESPGHAN experts defined specific consensus conditions for diagnose of constipation in pediatric patients with CF in 201012; only two of the six eligible publications published posteriorly to the ESPGHAN definition declared to have followed the guidelines’ recommendations.18,20 One study, the most recent in this selection,20 defined constipation according to the Cystic Fibrosis Foundation (CFF) as the presence of large volumes of thick stools retained in the colon. The eligible publications’ findings on prevalence of constipation in CF patients varied widely between 10% and 57%. Relevant causes of this divergence are apparently the different definitions adopted, the diverging objectives, and the varying eligibility criteria to include the cases.14–21
Diagnostic criteria must be clearly defined in prevalence studies.22 Constipation, as a nosological entity, is defined by the presence of clinical manifestations.23 However, among the proposed definition of symptoms required to diagnose constipation, no definition or proposed set of criteria is comprehensive enough to identify all patients suffering from this condition in clinical practice. The lack of a comprehensive consensus definition impairs not only clinical practice, but also epidemiological conclusions or comparisons and, particularly, the inclusion of subjects into clinical studies. In patients with CF, clinical manifestations of constipation have scarcely been described. In general, in these patients constipation is referred to as the etiological basis of abdominal pain. While ESPGHAN defined a set of clinical criteria, Littlewood24 described abdominal pain as indicative of chronic colonic fecal retention, recognizable in abdomen radiographies, and, finally, according to the CFF, constipation is defined by the presence of large volumes of thick stools retained in the colon, even in patients whose bowel movements are daily.25
Since uncomplicated constipation seems to be very common in CF patients and as there is an apparent association of constipation and DIOS, as well as with acute symptomatic fecal impaction, a unanimous use of consensus definitions is essential.
Two of the articles included in this systematic review approached constipation prevalence in order to identify triggering circumstances of this condition.17,21 Ooi et al.17 recorded constipation frequency according to temperature in different seasons of the year. A retrospective analysis including a period of 12 years revealed that CF patients’ admissions for constipation were significantly more frequent in periods with elevated temperatures. Constipation occurred more often during seasons with a mean temperature of 27.9°C (standard deviation, 6.3) compared with the season with a mean temperature of 24.0°C (4.1); p<0.0001). This indicates that physiopathology of constipation in CF patients is associated with dehydration, which supposedly leads to further thickening of mucus secreted by the colonic glands. Furthermore, a follow-up for around 15 years of patients who underwent surgery in the neonatal period revealed an association between constipation and history of meconium ileus (MI) (p=0.038). Patients with a previous history of MI more frequently demanded medical treatment for constipation.21
According to Littlewood,23 in addition to history and physical exam, abdominal radiography would be useful not only for diagnosis, but also for evaluation of the therapeutic result. The ESPGHAN12 and CFF25 definitions agree with the presence of excessive fecal retention in the large intestine, but performing a simple abdominal radiography to diagnose and manage constipation and fecal retention is not a consensus recommendation among the authors. Van der Doef et al.15 evaluated a series of 214 patients with CF, identifying a 47% rate of constipation. There were 106 patients who received abdominal radiographies, but, according to those authors, the study was not very useful to proceed with the treatment, because it presented high inter- and intra-observer variability rates for the Barr and Leech scores, which qualitatively measure fecal retention. Furthermore, such a procedure should be avoided as far as possible for radiation exposure. Studies in patients with functional constipation (FC) present little correlation between clinical symptoms and fecal impaction (FI) observed in the abdominal radiographies.26–28 In FC, there is evidence that radiographic images indicating FI occur with similar frequency in children with clinical constipation and in asymptomatic children.27,28
The present authors consider that the timely definition proposed by ESPGHAN10 experts would become more practical by adding a Bristol Scale29 and/or a score/criterion to quantify the symptoms relieved by the laxatives.
Constipation prevalence in patients with CF still deserves more studies that consider the definition proposed in 2010.12 From a correct identification of constipated patients, randomized clinical studies should be conducted in order to consistently determine associations, improve constipation management, and improve the quality of life of patients with CF (Table 1).
Studies on constipation prevalence in patients with cystic fibrosis.
| Author (year) | Study type | Study objective | Location | Population | Age group | Diagnostic criteria | Sample (n/constipated) | Constipation prevalence |
|---|---|---|---|---|---|---|---|---|
| Rubinstein et al. (1986)14 | Retrospective study | Determine the prevalence of constipation and meconium ileus | Children's Hospital, Stanford, United States | CF patients undergoing treatment | 0 to >30 years | Clinical judgment | 168/54 | 32% |
| Baker et al. (2005)16 | Multicentric prospective study | Evaluate the relationship between pancreatic enzymatic therapy and the clinical outcomes: growth, abdominal pain, constipation, flatulence, and bowel movements in patients with CF | 33 places credentialed by the Cystic Fibrosis Foundation | CF patients | >4 weeks to >14 years | Patient's report | 1074/616 | 57% |
| van der Doef et al. (2010)15 | Multicentric retrospective study | Determine prevalence, risk factors, and treatment in constipated patients with CF, as well as the diagnostic value of abdominal radiography | University Medical Center Utrecht, Holland | Pediatric patients undergoing treatment | ≤18 years | ESPGHAN, 2010 | 230/107 | 47% |
| Ooi et al. (2016)17 | Retrospective study | Determine if the prevalence of DIOS and constipation could be related to room temperature and volume of fluvial precipitation | Sydney Children's Hospital, Australia | Pediatric patients being treated at admission (outpatient not included) | ≤18 years | ESPGHAN, 2010 | 241/30 | 13% |
| Fraquelli et al. (2016)18 | Prospective study | Evaluate the frequency of ultrasound signals in the intestines of patients with CF regardless the presence of gastrointestinal symptoms and the co-relation of these signs with clinical symptoms and CFTR genotype | Reference center of the OspedaleMaggiore Policlinico, Milan, Italy | Outpatients | 10 to 22 years | Patient's report | 70/11 | 16% |
| Munck et al. (2016)19 | Prospective longitudinal observational study | Evaluate DIOS clinical manifestations (complete and incomplete) | 27 University Hospitals in 10 countries (9 European countries and Israel) | Adult and pediatric patients admitted for DIOS | 6 to 24 years | Patient's report | 109/44 | 40% |
| Santos et al. (2018)20 | Analytical transversal | Describe the clinical phenotype of children and adolescents with CF and evaluate the role of pancreatic insufficiency and neonatal screening in the diagnosis | Pediatric Reference Center, Brasília, Brazil | Pediatric patients undergoing treatment | ≤18 years | Patient's report | 77/26 | 34% |
| Mentessidou et al. (2018)21 | Retrospective comparative study | Investigated the incidence of long-term obstruction sequel (constipation, DIOS and growth) in patients with CF who have undergone surgery for meconium ileus in the neonatal period | Aghia Sophia Children's Hospital, Greece | CF patients operated for meconium ileus | 0 to 26 years | Episodes of chronic gradual fecal impaction of the colon (according to CFF) | 49/5 | 10% |
DIOS, distal intestinal obstruction syndrome; CF, cystic fibrosis; CFF, Cystic Fibrosis Foundation; ESPGHAN, European Society for Pediatric Gastroenterology, Hepatology, and Nutrition; CFTR, cystic fibrosis trans membrane conductance regulator.
The author M.A.S. has received a master's scholarship from Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES) – Finance Code 001.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Stefano MA, Poderoso RE, Mainz JG, Ribeiro JD, Ribeiro AF, Lomazi EA. Prevalence of constipation in cystic fibrosis patients: a systematic review of observational studies. J Pediatr (Rio J). 2020;96:686–93.