To identify the risk factors for the development of acute kidney injury and for short and long-term mortality of patients with acute kidney injury after admission to the Pediatric Intensive Care Unit.
Materials and methodsRetrospective analysis of patients admitted to the Pediatric Intensive Care Unit from January 2004 to December 2008. Acute kidney injury was defined by the KDIGO criterion. Risk factors for acute kidney injury, in-hospital, and long-term mortality were obtained through multivariate logistic regression analysis. Long-term mortality (up to 2011) was obtained by searching the institution’s database and by telephone contact with patients’ family members.
ResultsA total of 434 patients were evaluated and the incidence of acute kidney injury was 64%. Most acute kidney injury episodes (78%) occurred within the first 24hours after admission to the Pediatric Intensive Care Unit. The risk factors for the development of acute kidney injury were: low volume of diuresis, younger age, mechanical ventilation, vasoactive drugs, diuretics, and amphotericin. Lower weight, positive fluid balance, acute kidney injury, dopamine use and mechanical ventilation were independent risk factors for in-hospital mortality. Long-term mortality was 17.8%. Systolic blood pressure, PRISM score, low volume of diuresis, and mechanical ventilation were independent risk factors associated with long-term mortality after admission to the Pediatric Intensive Care Unit.
ConclusionAcute kidney injury was a frequent, early event, and was associated with in-hospital mortality and long-term mortality after admission to the Pediatric Intensive Care Unit.
Identificar os fatores de risco para o desenvolvimento de lesão renal aguda, mortalidade a curto e em longo prazo de pacientes com lesão renal aguda após internação em Unidade de Terapia Intensiva Pediátrica.
Materiais e métodosAnálise retrospectiva de pacientes internados em unidade de terapia intensiva pediátrica de janeiro de 2004 a dezembro de 2008. Lesão renal aguda foi definida pelo critério KDIGO. Fatores de risco para lesão renal aguda, mortalidade hospitalar e em longo prazo foram obtidos através de análise multivariada por regressão logística. Mortalidade em longo prazo (até 2011) foi obtida através de busca no banco de dados da instituição e contato telefônico com parentes dos pacientes.
ResultadosForam avaliados 434 pacientes e a incidência de lesão renal aguda foi de 64%. A maioria dos episódios de lesão renal aguda (78%) ocorreu nas primeiras 24 horas após internação na Unidade de Terapia Intensiva Pediátrica. Os fatores de risco para o desenvolvimento de lesão renal aguda encontrados foram: baixo volume de diurese, menoridade, uso de ventilação mecânica, droga vasoativa, diurético e anfotericina. Menor peso, balanço hídrico positivo, lesão renal aguda, uso de dopamina e ventilação mecânica foram fatores de risco independentes para mortalidade hospitalar. A mortalidade em longo prazo foi de 17,8%. Pressão arterial sistólica, escore PRISM, baixo volume de diurese e ventilação mecânica foram fatores de risco independentes associados à mortalidade em longo prazo após internação na Unidade de Terapia Intensiva Pediátrica.
ConclusãoLesão renal aguda foi um evento frequente, precoce e esteve associada à mortalidade hospitalar e em longo prazo após internação na Unidade de Terapia Intensiva Pediátrica.
The advances in intensive care have reduced the mortality of critically-ill adult and pediatric patients. Thus, Acute Kidney Injury (AKI) is becoming increasingly frequent in patients admitted to a Pediatric Intensive Care Unit (PICU). Its incidence varies from 5% to 82% and depends on the definition of AKI used.1–5 For many years, it was not possible to compare studies because of the diversity of AKI definitions. With the emergence of the RIFLE (Risk, Injury, Failure, Loss, and End-Stage Renal Failure) criteria, modified RIFLE for Pediatric patients (pRIFLE), AKIN (Acute Kidney Injury Network) and, more recently, the KDIGO (Kidney Disease: Improving Global Outcomes) classification, there has been a standardization of the definition of AKI, making it possible to compare the results obtained in different medical centers.4,6–8
As a result of the increased incidence of AKI in intensive care units, several authors have evaluated the impact of this disease in the short, medium, and long term.1,3,9–11 In adults, AKI increases the morbidity and mortality rate in the short and long term. Moreover, in this population, patients surviving an AKI episode are more likely to progress to chronic kidney dysfunction, and to eventually need permanent dialysis.12–15
Long-term prognostic studies in the pediatric population are still scarce, but they already suggest that, similarly to adults, there is an impact from AKI on late outcomes.10,11 The aim of this study was to evaluate the short-and long-term prognosis of children who developed AKI during PICU admission.
MethodThis study retrospectively studied all children and adolescents aged between 1 month and 13 years who were admitted to the PICU from January 2004 to December 2008. Patients in the postoperative period of cardiac surgery were excluded, as well as those with hemolyticuremic syndrome, chronic kidney disease, renal transplantation and those who did not have two serum creatinine measurements within a 7 day period or less. For patients with more than one AKI episode, only the first episode was considered in the statistical analysis. This study was approved by the research ethics committee of the institution.
AKI was defined through the KDIGO classification.8 In children who did not have serum creatinine prior to PICU admission, the serum creatinine expected for the age was considered as the baseline value.16
The clinical (age, weight, fluid balance, diuresis, heart and respiratory rate, blood pressure, Glasgow scale, PRISM II (Pediatric Risk of Mortality) score, vasoactive drug use, and mechanical ventilation) and laboratory (electrolytes, creatinine, blood gas, complete blood count, transaminases, cultures) data were collected from the electronic medical records at hospital/PICU admission and at hospital/PICU discharge. In patients who developed kidney dysfunction, clinical and laboratory data were also collected at the beginning and end of AKI. To evaluate the long-term mortality, a search was conducted in the institution’s database and by telephone contact with patients’ family members during the year 2011.
The statistical analysis was performed using the software SPSS, v.14 (SPSS Inc., Chicago, IL, United States). Continuous variables were expressed as mean ± standard deviation or median and interquartile range. Categorical variables were presented as a percentage of the number of cases. Continuous variables were assessed by Student's t-test or Mann–Whitney test, as needed. Categorical variables were assessed using the chi-squared test. The logistic regression multivariate analysis was performed to obtain independent prognostic factors for the development of AKI, and in-hospital and long-term mortality was carried out including the variables with p < 0.1 in the univariate analysis. Results were expressed as Odds Ratio (OR) and 95% Confidence Interval (95% CI). A p-value < 0.05 was considered significant.
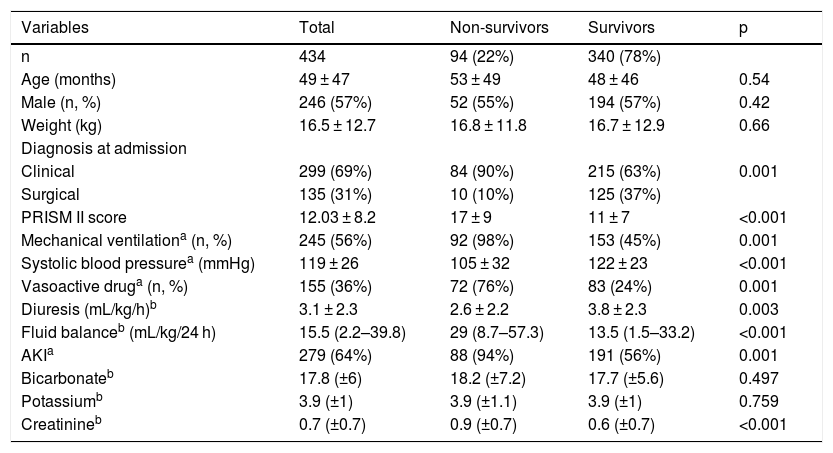
ResultsDuring the study period, 723 children were admitted to the PICU. Of these, 434 children met the inclusion criteria. The reasons for exclusion were: postoperative cardiac surgery period (147); fewer than two creatinine level measurements in 7 days (109); chronic kidney disease (21) and hemolytic uremic syndrome (12). There was a predominance of male patients (57%) and the mean age was 49 ± 47 months. Clinical causes were the main reasons for hospitalization, with pulmonary diseases (30.6%), central nervous system diseases (20.9%) and sepsis (18.9%) being the most frequent. There were no significant differences between surviving and non-surviving children in relation to gender, age and weight (Table 1).
Clinical characteristics of patients admitted to the Pediatric Intensive Care Unit (PICU).
| Variables | Total | Non-survivors | Survivors | p |
|---|---|---|---|---|
| n | 434 | 94 (22%) | 340 (78%) | |
| Age (months) | 49 ± 47 | 53 ± 49 | 48 ± 46 | 0.54 |
| Male (n, %) | 246 (57%) | 52 (55%) | 194 (57%) | 0.42 |
| Weight (kg) | 16.5 ± 12.7 | 16.8 ± 11.8 | 16.7 ± 12.9 | 0.66 |
| Diagnosis at admission | ||||
| Clinical | 299 (69%) | 84 (90%) | 215 (63%) | 0.001 |
| Surgical | 135 (31%) | 10 (10%) | 125 (37%) | |
| PRISM II score | 12.03 ± 8.2 | 17 ± 9 | 11 ± 7 | <0.001 |
| Mechanical ventilationa (n, %) | 245 (56%) | 92 (98%) | 153 (45%) | 0.001 |
| Systolic blood pressurea (mmHg) | 119 ± 26 | 105 ± 32 | 122 ± 23 | <0.001 |
| Vasoactive druga (n, %) | 155 (36%) | 72 (76%) | 83 (24%) | 0.001 |
| Diuresis (mL/kg/h)b | 3.1 ± 2.3 | 2.6 ± 2.2 | 3.8 ± 2.3 | 0.003 |
| Fluid balanceb (mL/kg/24 h) | 15.5 (2.2–39.8) | 29 (8.7–57.3) | 13.5 (1.5–33.2) | <0.001 |
| AKIa | 279 (64%) | 88 (94%) | 191 (56%) | 0.001 |
| Bicarbonateb | 17.8 (±6) | 18.2 (±7.2) | 17.7 (±5.6) | 0.497 |
| Potassiumb | 3.9 (±1) | 3.9 (±1.1) | 3.9 (±1) | 0.759 |
| Creatinineb | 0.7 (±0.7) | 0.9 (±0.7) | 0.6 (±0.7) | <0.001 |
Data are expressed as mean ± SD or median and 95% CI. SD, Standard Deviation; CI, Confidence Interval.
Non-survivors were already severely ill at PICU admission, as demonstrated by the PRISM score, need for mechanical ventilation, and vasoactive drug use. In the first 24 h of PICU stay, the children who did not survive had a significantly higher fluid balance and lower diuresis than the surviving children (Table 1). Serum creatinine and the proportion of patients with AKI were higher in the group of non-surviving patients.
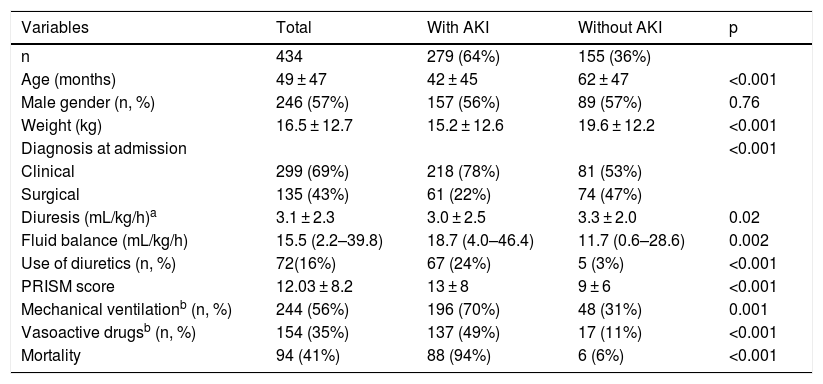
AKI occurred in 279 (64%) children, classified as Stage I in 106 (38%), Stage II in 113 (40.5%) and Stage III in 60 (21.5%) children. Of the 279 patients with AKI, 217 (78%) had AKI within the first 24 h of PICU admission. Patients with AKI were younger, had a higher PRISM score, greater positive fluid balance, and lower diuresis than children who did not develop the disease (Table 2).
Characteristics of patients with Acute Kidney Injury (AKI) in the Pediatric Intensive Care Unit (PICU).
| Variables | Total | With AKI | Without AKI | p |
|---|---|---|---|---|
| n | 434 | 279 (64%) | 155 (36%) | |
| Age (months) | 49 ± 47 | 42 ± 45 | 62 ± 47 | <0.001 |
| Male gender (n, %) | 246 (57%) | 157 (56%) | 89 (57%) | 0.76 |
| Weight (kg) | 16.5 ± 12.7 | 15.2 ± 12.6 | 19.6 ± 12.2 | <0.001 |
| Diagnosis at admission | <0.001 | |||
| Clinical | 299 (69%) | 218 (78%) | 81 (53%) | |
| Surgical | 135 (43%) | 61 (22%) | 74 (47%) | |
| Diuresis (mL/kg/h)a | 3.1 ± 2.3 | 3.0 ± 2.5 | 3.3 ± 2.0 | 0.02 |
| Fluid balance (mL/kg/h) | 15.5 (2.2–39.8) | 18.7 (4.0–46.4) | 11.7 (0.6–28.6) | 0.002 |
| Use of diuretics (n, %) | 72(16%) | 67 (24%) | 5 (3%) | <0.001 |
| PRISM score | 12.03 ± 8.2 | 13 ± 8 | 9 ± 6 | <0.001 |
| Mechanical ventilationb (n, %) | 244 (56%) | 196 (70%) | 48 (31%) | 0.001 |
| Vasoactive drugsb (n, %) | 154 (35%) | 137 (49%) | 17 (11%) | <0.001 |
| Mortality | 94 (41%) | 88 (94%) | 6 (6%) | <0.001 |
Data expressed as mean ± SD or median and 95% CI.
During hospitalization in the PICU, mechanical ventilation and vasoactive drug use were more frequent in children who developed AKI (Table 2). Time of mechanical ventilation was also higher in children who developed AKI (6.0 [2.0–16] vs. 3.0 [2.0–5.75] days, p = 0.0003). The length of hospital stay (41.8 ± 5.4 vs. 25.3 ± 4.5 days) and the percentage of children who required readmission (79.2% vs. 20.8%, p = 0.004) at the PICU were higher in children who developed AKI. Renal replacement therapy was required in 16 children. The mortality of patients with AKI was higher than in those who did not develop the disease. Of the 88 in-hospital deaths in patients with AKI, 66 (75%) had acute kidney injury within the first 24 h of hospital admission.
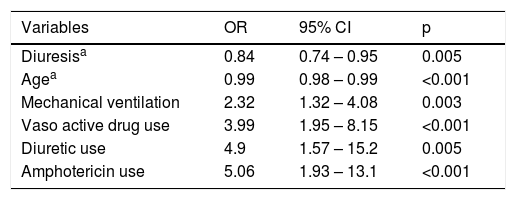
After the logistic regression, the following risk factors were identified for AKI development: use of mechanical ventilation, vasoactive drugs, diuretics, and amphotericin. Older age and greater volume of diuresis were protective factors against the development of AKI (Table 3). Weight, positive fluid balance, AKI, dopamine use, and mechanical ventilation were independent risk factors for in-hospital mortality (Table 4).
Risk factors for Acute Kidney Injury (AKI) after Pediatric Intensive Care Unit (PICU) admission.
| Variables | OR | 95% CI | p |
|---|---|---|---|
| Diuresisa | 0.84 | 0.74 – 0.95 | 0.005 |
| Agea | 0.99 | 0.98 – 0.99 | <0.001 |
| Mechanical ventilation | 2.32 | 1.32 – 4.08 | 0.003 |
| Vaso active drug use | 3.99 | 1.95 – 8.15 | <0.001 |
| Diuretic use | 4.9 | 1.57 – 15.2 | 0.005 |
| Amphotericin use | 5.06 | 1.93 – 13.1 | <0.001 |
OR, odds ratio.
Risk factors for mortality after Pediatric Intensive Care Unit (PICU) admission.
| Hospital mortality | |||
|---|---|---|---|
| Variables | OR | 95%CI | p |
| Weighta | 1.2 | 1.02–2.1 | 0.002 |
| Fluid overloadb | 2.3 | 1.2–3.01 | 0.036 |
| AKI | 3.3 | 1.09–13.43 | 0.011 |
| Dopamine | 4.85 | 1.59–14.77 | 0.005 |
| Mechanical ventilation | 19.1 | 2.14–17.05 | 0.008 |
| Long-term mortality | |||
|---|---|---|---|
| Variables | OR | 95%CI | p |
| Systolic blood pressurea | 1.09 | 1.04–1.14 | 0.001 |
| PRISMb score | 1.11 | 1.04–1.18 | 0.001 |
| Diuresisa | 2.21 | 1.2–4.07 | 0.011 |
| Mechanical ventilation | 4.61 | 2.36–9.02 | 0.012 |
AKI, Acute Kidney Injury.
Of the 340 surviving patients, information on long-term mortality was obtained from 238 (70%) children. Of these, 146 (61.3%) had AKI during their stay in the PICU. The long-term mortality rate was 17.8%. Of the 26 late deaths in AKI patients, 24 (92%) had AKI in the first 24 h of hospitalization. Low systolic blood pressure, PRISM score, low volume of diuresis, and mechanical ventilation were independent risk factors associated with long-term mortality after PICU stay (Table 4).
DiscussionThis study found a high incidence of AKI (64%), defined by the KDIGO classification. The incidence of AKI in the PICU depends, among many variables, on the applied definition and disease severity in the studied population. The few published studies using the KDIGO classification in pediatric patients have shown that this classification adequately identifies AKI and is correlated with disease severity and mortality.17 The pRIFLE score was not used in this study, because the height was not available in all children for the calculation of creatinine clearance estimated by the Schwartz formula.18
The patients’ disease severity in this study contributed to the high incidence of AKIfound. Up to 82% of severely ill children can have acute renal dysfunction.4 This severity may be demonstrated by the PRISM score, and high need for mechanical ventilation and vasoactive drugs, particularly among patients who developed AKI. Also, the fluid balance was higher in the first 24 h after PICU admission among children who died. A positive fluid balance is correlated with morbidity and mortality in critically ill patients, particularly in those with AKI.19–23 Volume of diuresis and age were identified as protective factors for the development of AKI in the multivariate analysis. Younger children are more prone to the development of AKI.2 Lower body surface area might contribute to the development of AKI after hypovolemia and exposure to nephrotoxic agents.24,25 This hypothesis could explain the association of diuretics and amphotericin as independent factors for the development of AKI. In addition to the patients’ disease severity (fluid overload, dopamine use, and mechanical ventilation) and low weight, AKI was an independent risk factor for in-hospital mortality.
AKI was an early event during PICU admission. Most patients developed AKI in the first 24 h of PICU hospitalization and mortality was higher in this group. Duzova et al. found AKI in 63% of patients within the first 24 h of admission. Therefore, AKI prevention should start as soon as PICU admission, with adequate hemodynamic stabilization and reduction of exposure to nephrotoxic drugs.2
Few studies have evaluated the impact of AKI on late mortality. Askenazi et al. reported late survival of 80% (3–5 years), and most deaths occurred within the first 12 months after hospital admission.10 In children with dialytic AKI after cardiac surgery for the correction of congenital defects, Mel et al. found a mortality rate of 20% after 3.5–10.5 years.26 Although the long-term evaluation was not performed in all patients, the mortality rate found in this study was similar to the previously published data.27,28
Another consequence of AKI is the potential for triggering hypertension, proteinuria, and chronic kidney disease. Madsen et al. demonstrated the impact of AKI on the development of chronic kidney disease in children undergoing cardiac surgery. AKI occurred in 33% of cases and the incidence of chronic renal disease in five years was 12% in patients who had AKI, compared to 3% in those who did not have post operative renal dysfunction.29 This should be considered in pediatric consultations and the pediatrician should be aware to recognize these outcomes.
Patients’ severity status and AKI influenced the late mortality found in this study. Systolic blood pressure, PRISM score, and mechanical ventilation were independent factors associated with late mortality. Lower volume of diuresis was a risk factor for long-term mortality. As diuresis is one of the criteria for AKI classification, it can be deduced that there is a correlation between AKI and higher mortality in the long term.
This study has some limitations. Despite being a single-center, retrospective study, the results did not disagree with those in the literature. Although late assessment was not performed in all patients, late survival was similar to that found by other authors. Long-term renal function assessment was not performed, but this was not one of the initial objectives of this study. However, this is one of the few studies that used the KDIGO classification in the pediatric population and it is the largest study in the national literature on pediatric AKI.30 The number of assessed patients was significant, and risk factors for early and late mortality were identified.
The frequent and early occurrence of AKI after PICU admission reinforces the need to monitor renal function and reduce exposure to risk factors, such as hypotension and nephrotoxic drug use, especially in younger patients. In conclusion, AKI prevention has the potential to reduce morbidity and mortality in the short and long term.
Study conducted at Hospital de Base, Faculdade de Medicina de São José do Rio Preto (Famerp), São José do Rio Preto, SP, Brazil.
Please cite this article as: Ferreira MC, Lima EQ. Impact of the development of acute kidney injury on patients admitted to the pediatric intensive care unit. J Pediatr (Rio J). 2020;96:576–81.