Describe the epidemiology of deaths in children not submitted to CPR, compare to a CPR group and evaluate patients’ medical records of those not submitted to CPR.
MethodsObservational cross-sectional study assessing deaths between 2015 and 2018 in a pediatric tertiary hospital, divided into two groups: CPR and no- CPR. The source of data included the cardiorespiratory arrest register, based on Utstein style. Children's medical records in no-CPR group were researched by hand.
Results241 deaths were included, 162 in CPR group and 79 in the no-CPR group. Preexisting diseases were observed in 98.3% of patients and prior advanced intervention in 78%. Of the 241 deaths, 212 (88%) occurred in the PICU, being 138/162 (85.2%) in CPR group and 74/79 (93.7%) in no-CPR group (p = 0.018). Bradycardia as the initial rhythm was five times more frequent in the CPR group (OR 5.06, 95% CI 1.94–13,19). There was no statistically significant difference regarding age, gender, preexisting diseases, and period of the day of the occurrence of death. Medical records revealed factors related to the family decision-making process or the suitability of therapeutic effort. Discrepancies between the practice of CPR and medical records were identified in 9/79 (11,4%) records allocated to the no-CPR group.
ConclusionMost deaths with CPR and with the no-CPR occurred in the PICU. Bradycardia as the initial rhythm was five times more frequent in the CPR group. Medical records reflected the complexity of the decision not to perform CPR. Discrepancies were identified between practice and medical records in the no-CPR group.
The decision of “do not attempt cardiopulmonary resuscitation (no-CPR)” is complex and difficult to approach and can be quite challenging, especially when dealing with pediatric patients.1,2 The choice must consider several factors, including science, technology, respect, and ethics, in addition to the interests of the child and the family.3 The term “do not resuscitate (DNR)” was first used in 1974 and, in 1976, the discussion was taken a step further in hospitals in order to develop guidelines to guide the decision-making process.4
In specialized pediatric hospitals that treat a significant number of children with severe complex diseases, it is imperative to discuss the end of life issues and how to approach them, however, there are no criteria and protocols to guide this decision-making process 5 properly. The biggest challenge involves establishing which patients will benefit from technological support.6,7
Some authors study local and context of deaths in children with complex chronic diseases in an attempt to establish a patient and family profile capable of adding quality in care in end of life cases.7–11
Several authors also take into consideration historical, legal, ethical, and religious aspects and in defending the importance of caregiver/family participation and a good relationship between family members and health professionals, especially during the end of life.9–14 Other authors also add another aspect: the individuality of each child.15
Most publications on life support limitations are concentrated in developed countries and tend to be limited in Brazil. Life support therapies have undergone changes as the technological advances in medicine grow and new challenges emerge.9–11,16,17
Previous studies at the Instituto da Criança do Hospital de Clínicas da Faculdade de Medicina da Universidade de São Paulo (ICr-HCFMUSP) have established the presence of discrepancies between medical practice and what is actually included in the patient's medical records at the time of death.18–20 Currently, the decision of no-CPR is considered useful to prevent unnecessary and invasive treatments during the end of life. Ethical and legal factors are implicit when a decision is made not to resuscitate.21–23
Collecting experiences from the Brazilian territory, identifying no-CPR patients and determining available resources are important steps to further the discussion on life support during conflicting situations.6,9–11,16,17
This study aims to contribute to the data regarding epidemiological factors involved in do not resuscitate decisions in pediatrics – a subject still little explored in current literature –, and thus further the discussion on this theme, spread awareness on current guidelines and identify criteria used in cases of no-CPR. This study also aims to establish a comparison with previous publications carried out in this same institution, seeking possible changes in the medical record associated with no-CPR.
MethodsThe study was conducted at the ICr-HCFMUSP, a public academic hospital, reference in the treatment of tertiary/quaternary pediatric patients. For the purposes of this analysis, the authors included all patients aged 0–20 years who died at this hospital in the established period. All cardiorespiratory arrest events that occurred outside the hospital were excluded.
This observational, retrospective, cross-sectional study contemplates all deaths that occurred from January 1, 2015, to December 31, 2018. The data source was the cardiorespiratory arrest registration records, which follow the Utstein style recommended by the International Liaison Committee on Resuscitation (ILCOR), as per Supplementary material.19
The authors also conducted an active search of all medical records not included in the cardiorespiratory arrest registration, thus ensuring that all deaths that occurred within this period were contemplated in this study.19
The sample was chosen for convenience without a sample calculation. The project was approved by the Research Ethics Committee (CEP) of the Hospital das Clínicas of the University of São Paulo (HCFMUSP), and the necessity of Free and Informed Consent (FIC) was waivered since it is a retrospective study that analyzed a database of preexisting records.
The dependent variable was whether or not CPR was performed, which determined two study groups: CPR and no-CPR. Independent variables consisted of age, gender, time of death, preexisting diseases, location, interventions prior to the event, immediate causes, and an initial cardiac rhythm at the moment of cardiorespiratory arrest.
The time of death was classified according to the period of the day the death occurred: day (from 7 a.m. to 06 h59 p.m.) and night (from 7 p.m. to 06 h59 a.m.). Preexisting diseases were classified in accordance with prevalence. Location of death included: emergency room (ER), intensive care unit (ICU), operating room, outpatient clinics, wards and not defined.
The evaluation of physiological instability prior to cardiorespiratory arrest, which is directly related to the patient's severity, was identified according to the level of intervention required: (1) no intervention; (2) basic intervention (oxygen supplementation, cardiac monitor, assisted ventilation and venous access without vasoactive drugs); and (3) advanced intervention (advanced airway management and/or use of vasoactive drugs). The immediate cause of death, was classified as hypotension/shock, respiratory and metabolic.
Initial rhythm at the time of CPR arrest was divided into (1) bradycardia (symptomatic bradycardia determined by the Pediatric Advanced Life Support (PALS);24 (2) no-shockable rhythm (Pulseless electrical activity (PEA) and Asystole); and (3) shockable rhythm (Ventricular Fibrillation (VF) and Pulseless Ventricular Tachycardia (VT)).
A medical record in the no-CPR group was also analyzed regarding data related to the CPR arrest and death. These notes were reviewed and grouped according to patient severity and exhaustion of therapeutic measures. The authors also aimed to identify possible discrepancies between notations and medical practice.
Statistical analysisA descriptive analysis of the data was undertaken, with qualitative variables, distribution of absolute (n) and relative (%) frequencies and a summary of the main factors, such as position and dispersion for quantitative variables.
To assess the possible connection between qualitative variables and the use of CPR measures, the authors applied the independence test (Fisher's Exact Test or the Chi- Square Test). To carry out the comparison between mean age and the CPR variable, the authors used the parametric Student t-test for independent samples.
The simple and multiple logistic regression model was adjusted to the data in order to identify possible independent factors (gender, age, etc.) for the occurrence of CPR, that is, whether there were any factors that influenced the outcome variable (CPR). The results were presented in odds ratio (OR) and the respective 95% confidence interval (95% CI).
For the multiple model adjustment, the authors considered those independent variables with p-value lower than 0.2 in the simple logistic regression model. The stepwise (backward) method was employed to obtain the final model. The quality of the adjusted model was assessed using the Hosmer-Lemeshow test.
The significance level adopted was 5%. Free R software, version 3.5, was used in all analyzes.
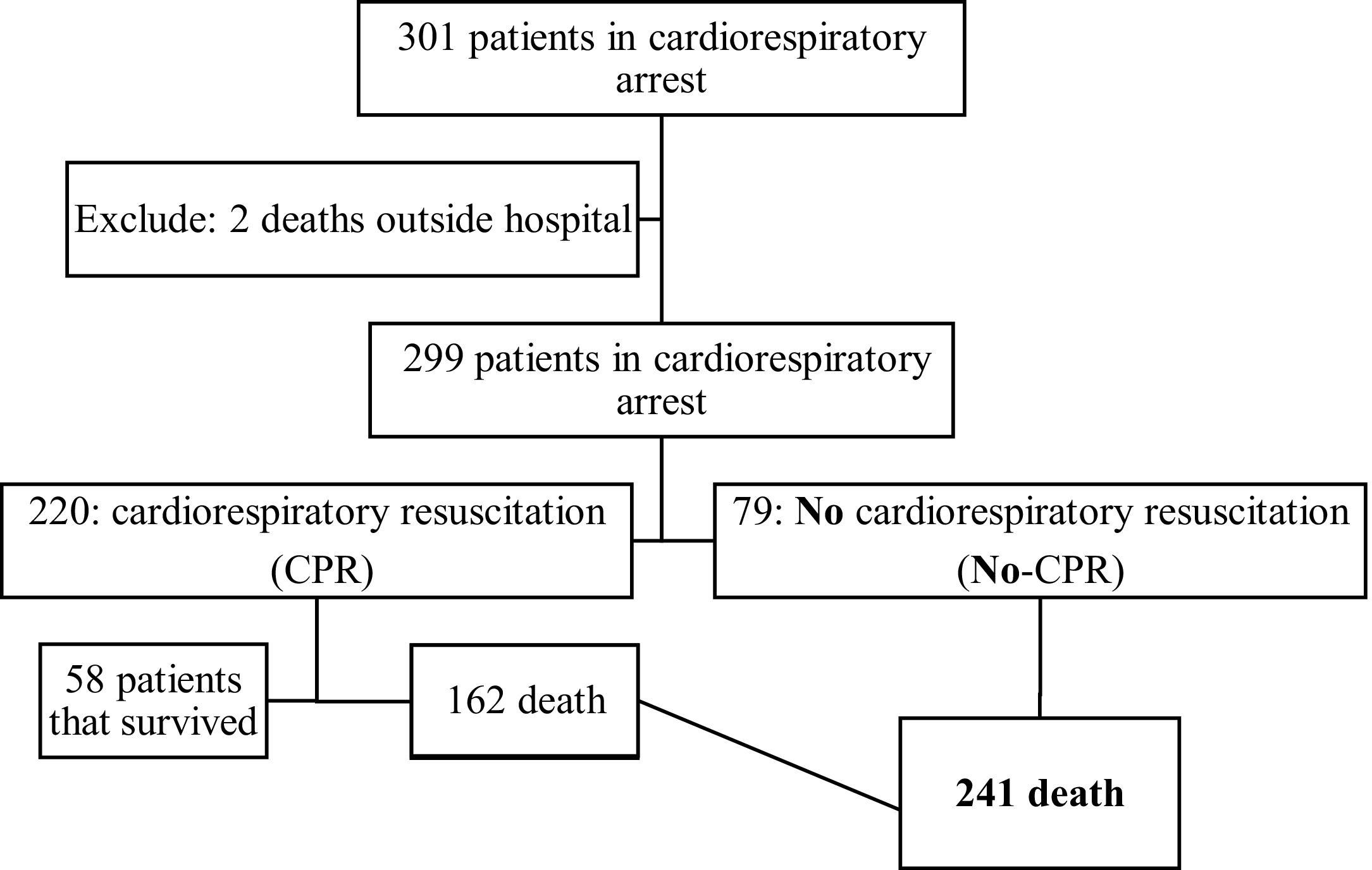
ResultsThe authors identified 301 CPR arrest events over a 4-year period, among whom 241 ended in death. Of these, 162 (67.2%) were submitted to CPR maneuvers (CPR group), and 79 (32.8%) were not (no-CPR group), according to the Figure 1. In the observed period, the in-hospital mortality rate was 80% (241/301), and brain death occurred in 15 of the 79 (18.8%) patients not submitted to CPR.
The characteristics of the studied population are listed in Table 1. There was a predominance of infants, equivalent distribution of genders, discrete predominance of daytime events compared to overnight events. Most of the patients (98.3%) had preexisting illnesses, and the deaths occurred most often in the ICU (88.0%), while most patients received the prior advanced intervention (78%).
Characteristics of the population: deaths that occurred at the ICr-FMUSP in the study period.
ER, emergency room; PICU, pediatric intensive care unit.
As for the immediate causes that led to the cardiorespiratory arrest and subsequent death, the authors observed a predominance of circulatory causes in 48.1% and initial rhythm as bradycardia in 43.2%. Preexisting diseases are listed in Table 2.
Preexisting conditions in patients who died during the study period.
CPR, cardiorespiratory resuscitation.
Table 3 includes the distribution of variables within the CPR and the no-CPR groups. No significant statistical difference was observed for the variables age, gender, period of the day and preexisting diseases. There was a statistically significant difference regarding the place of death between the two groups (p = 0.018), suggesting that the decision not to perform CPR occurred more frequently in the ICU. In the ER, the trend ran opposite, with 8.6% in the CPR group and 1.3% in the no-CPR group. CPR was performed in all cases that lead to death in the operating room.
Distribution of variables between the study groups.
| Variable | Category | CPR (%) | No-CPR (%) | p value |
|---|---|---|---|---|
| Age (years) | Mean (SD) | 3 (4.7) | 4 (4.8) | 0.29a |
| Gender | F | 78 (48.1) | 41 (51.9) | 0.682b |
| M | 84 (51.9) | 38 (48.1) | ||
| Period | Day | 77 (49.4) | 43 (58.1) | 0.272b |
| Night | 79 (50.6) | 31 (41.9) | ||
| Preexisting disease | Transplantation/hepatopathy | 44 (27.2) | 30 (38) | 0.224c |
| Genetic syndrome/ Malformation | 50 (30.9) | 18 (22.8) | ||
| Others | 66 (40.7) | 29 (36.7) | ||
| None | 2 (1.2) | 2 (2.5) | ||
| Local | ER | 14 (8.6) | 1 (1.3) | 0.018c |
| Wards | 4 (2.5) | 4 (5.1) | ||
| PICU | 138 (85.2) | 74 (93.7) | ||
| Operating room (OR) | 6 (3.7) | 0 (0) | ||
| Local excluding OR | ER | 14 (8.6) | 1 (1.3) | 0.0497d |
| Wards | 4 (2.5) | 4 (5.1) | ||
| PICU | 138 (85.2) | 74 (93.7) | ||
| Prior intervention | None | 15 (9.3) | 4 (5.1) | 0.441d |
| Basic | 24 (14.8) | 10 (12.7) | ||
| Advanced | 123 (75.9) | 65 (82.3) | ||
| Causes | Hypotension/shock | 71 (44.9) | 43 (54.4) | 0.132d |
| Respiratory | 54 (34.2) | 17 (21.5) | ||
| Others | 33 (20.9) | 19 (24.1) | ||
| Rhythm | Bradycardia | 79 (48.8) | 25 (31.6) | 0.013d |
| Non-shockable | 70 (43.2) | 40 (50.6) | ||
| Shockable | 13 (8) | 14 (17.7) |
ER, emergency room; PICU, pediatric intensive care unit.
The prior advanced intervention was noted in most cases and, although there is a higher prevalence in the no-CPR group, suggesting greater severity, there was no statistical significance.
The respiratory cause was more frequent in the CPR group compared to the no- CPR group (34.2 and 21.5%, respectively), but this difference was not statistically significant. The inverse was observed in cardiorespiratory arrest caused by shock (54.4 and 44.9%, respectively).
Significant statistical difference was observed in the initial rhythm between the two groups, with the initial rhythm as bradycardia present in 48.8% in the CPR group and 31.6% in the no-CPR group (p = 0.013). The presence of non-shockable rhythms were observed much less frequently in the CPR group (43.2%) than the no-CPR (50.6%), but such was not statistically significant.
Table 4 shows simple and multiple logistic regression of outcomes in the CPR group. When cardiorespiratory arrest occurred in the ICU, the likelihood of CPR was reduced, though the confidence interval remained very wide (OR: 0.119/CI 0.0150–0.936). Bradycardia was five times more likely to lead to CPR maneuvers than any other initial rhythm (OR: 5.06/CI 1.940–13.199).
Simple and multiple logistic regression model regarding outcomes in the CPR group.
ER, emergency room; PICU, pediatric intensive care unit.
The review of the medical record of all 79 patients in the no-CPR group revealed descriptions of the severity of each patient, mentions of the appropriate therapeutic measures, registration of the use of comfort measures, and the option of not employing invasive procedures. In 33, the authors noted mentions of conversations with family members regarding the case, identified by phrases such as: “talked to the mother...”, “talked to the parents...”, “talked to the family...”, “family is aware...”, “relatives consent...”, “parents agree not to perform CPR...”, “mother agreed to...”, “parents aware of the seriousness”, “agreed to limit intervention”, “agreed to stop life support measures”, “agreed to prioritize comfort measures”. Such observations suggest that medical therapies were shared with the family members and that they had some understanding of the no-CPR option.
Discrepancies between in the medical record and the medical practice regarding no-CPR was observed in 9 of the 79 deaths (11.4%), i.e., the notes in the medical records suggested CPR maneuvers were employed, but the cardiopulmonary arrest register identified the case as no-CPR. The description found in these medical records was “did not respond to CPR”. However, most records (88.6%) showed concordance between practice and notations, with good technical descriptions, including initial rhythms during CPR and the decision not to use drugs in resuscitation.
DiscussionThis study analyzed 241 deaths that occurred from January 2015 to December 2018, 162 that performed CPR (67.2%), and 79 no-CPR (32.8%). Among the variables associated with not performing CPR, the local of the event and initial rhythm of cardiopulmonary arrest was relevant.
The no-CPR rate observed in studies carried out at the same institution in 2000 and 2009 showed 26.7% and 36.2%, respectively,18,20 suggesting an increase in the no-CPR rate between these two periods and a stabilization in the current study. Data from other countries reveal higher rates, ranging from 48% to 95,8%.6,9–12,17 It is difficult to compare data among these studies since they were conducted in institutions of varying levels of complexity and not all had a bioethics committee.11,16
One of the main purposes of this study was the exploratory analysis of objective variables that could be associated with the no-CPR option. Age, gender, period of the day, therapeutic interventions, and immediate cause of cardiopulmonary arrest in patients that progressed to death are aspects already explored by other authors.3,6,9–12,16,17,25–28 Despite different rates among the studies, no significant statistical difference was observed in these variables between the CPR and no-CPR groups, the same as in the present study.
In this study, 98.3% of patients had a preexisting disease, with a similar prevalence among the analyzed groups. The current literature shows different percentages of preexisting diseases, ranging from 50%5 to 100%.27,28
Regarding the location of the event, the authors observed a statistical difference between the two groups; 85.2% of the patients in the CPR group and 93.7% in the no-CPR group died while in the ICU (p = 0.018). The decision not to resuscitate also occurred more frequently in the ICU than in other locations, something already pointed out in the Brazilian literature and previous studies carried out at the ICr- HCFMUSP.18,20 It is understandable that, in the ICU, a conversation with family members about the option not to resuscitate is more likely to occur, thus allowing this option to be used more frequently than in the ER.6,9–14,17,26,27
In this study, a statistically significant difference in the initial rhythm was observed between the two groups, with bradycardia being associated with five times more chance to perform CPR. No studies in the literature had previously analyzed the role of initial rhythm during cardiorespiratory arrest in patients who progressed to death and were not submitted to CPR.
Advanced life support protocols24 advocate early recognition and treatment of bradycardia in critically ill patients with indications for CPR. On the other hand, the use of life support in patients with little chance of survival who present with bradycardia may not be justified, only delaying death. A more careful analysis of the occurrence of bradycardia in relation to deaths, and not just CPR, should consider that other variables related to each patient might possibly interfere in the decision to perform CPR.
The criteria for choosing not to resuscitate are complex and may differ between institutions, which makes it difficult to compare studies. The analysis of these aspects as part of an attempt to determine variables that could interfere with the decision not to resuscitate, and, due to the complexity of this topic, it is understandable that the decision-making process must be influenced by factors other than those explored here. Future studies should expand the investigation.
A relevant aspect of this study was the analysis of medical record notes, also conducted by other authors in the same institution.18–20 The active search for pre-event notes presented in these medical records revealed factors related to family participation and adequacy of therapeutic effort.
Some phrases found in these medical records suggested that family participation seems to have been significant in the decision-making process. Other studies demonstrate the same trend, though a precise comparison between them was hampered by different methodologies.10 The authors highlight several points regarding shared decision-making in pediatrics, including less conflict with family members. Aspects related to the patient's culture and families and their influence during end-of-life decisions were also addressed by several authors.13,14,25,29
Discussion about the adequacy of therapeutic effort is also found in the current literature, and the authors reinforce the importance of carrying out comfort measures and/or therapeutic limitation, removing or not employing any life support measures in patients with little chance of survival.5,11,13,27 This concern was observed in the medical record notations analyzed in this study. Further analysis should be made in the future about this subject, with the use of structured interviews.
Some discrepancies between practice and notes in the medical records were found in 9 of the 79 (11.4%). These notes suggested that CPR maneuvers were performed in patients who progressed to death, though no such maneuvers occurred. This observation is of great ethical concern within an academic hospital. 23 Discussion of fundamental dilemmas in pediatric practice may reduce these divergences.
There was a progressive increase in concordance over time, as per data collected at three different times in the ICr-HCFMUSP: 27.5% in 2000; 86.5% in 2009; and 88.6% in this study, which may represent institutional changes and greater concern with approach and ethical-legal implications related to this subject.11,16,18,20
Studies since the 1990s have already indicated the inherent challenge of deciding not to resuscitate children due to several aspects, one of them being the lack of consensus and protocols to support this choice.5,15,17 The decision to perform CPR tends to be more automatic, linked to the instinct for survival and preservation of life, and thus may require less reflection. However, this doesn't mean that it is the best choice for all patients. The option of no-CPR is more complex and requires further analysis; this study attempted to delve into objective and subjective data that could possibly contribute to the decision-making process of no-CPR. The end-of-life debate is challenging and should be implemented in Brazilian pediatric hospitals, following the example of other countries where discussions about non-CPR and brain death are often used as quality metrics.30
This study has some limitations since it is retrospective, though it was capable of identifying important factors in the no-CPR scenario within the institution. The absence of a specific record of no-CPR and deaths and the absence of a structured interview with family members made it difficult to elucidate the decision-making process. On the other hand, the use of the international CPR registration proved to be a useful tool that allowed us to identify patients that were not submitted to CPR.19
ConclusionMost of the deaths with CPR and with no-CPR occurred in the ICU. Bradycardia as the initial rhythm was more likely in the group CPR. Medical records reflected the complexity of the decision not to perform CPR. Discrepancies are still being identified between practice and medical records in the no-CPR group; however, this observation has been decreasing over time.
Study conducted at the Universidade de São Paulo, Faculdade de Medicina, Hospital das Clínicas, Instituto da Criança, Departamento Emergência, São Paulo, SP, Brazil.