This study aimed to examine the differences between mothers of preterm multiples and mothers of preterm singletons regarding perceived stress and maternal psychological symptoms, and to explore the putative adverse amplified effect of socioeconomic disadvantage.
MethodNinety-five mothers of 1-year-olds born preterm participated in this cross-sectional study. Data collection was carried out in two public hospitals from Northern Portugal. To assess maternal perceived daily stress and psychological symptoms, mothers completed two questionnaires. Mothers reported on socioeconomic factors, including family poverty, parent unemployment, and low education, and two groups of family socioeconomic disadvantage were created. A child medical risk index was calculated.
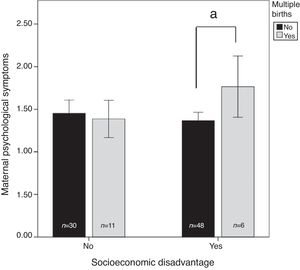
ResultsResults indicated that mothers of preterm multiples reported higher levels of stress than mothers of preterm singletons. Moreover, and specifically regarding psychological functioning, mothers of preterm multiples reported more symptoms than mothers of preterm singletons, but only when living in a context of socioeconomic adversity.
ConclusionsThe results of the present study have important implications for practice. Mothers of preterm multiples are at higher risk to present mental health difficulties, in comparison to mothers of singletons, especially when exposed to socioeconomic adversities. The development of psychosocial intervention programs and public policies are of decisive importance in helping mothers of multiples adjust to parenthood.
Examinar as diferenças entre mães de múltiplos prematuros e mães de filhos únicos prematuros a respeito de estresse percebido e sintomas psicológicos maternos e explorar o efeito adverso amplificado putativo da desvantagem socioeconômica.
MétodoParticiparam deste estudo transversal 95 mães de crianças de um ano nascidas prematuras. A coleta de dados foi feita em dois hospitais públicos do norte de Portugal. Para avaliar o estresse diário percebido e os sintomas psicológicos maternos, as mães responderam dois questionários. As mães relataram fatores socioeconômicos, incluindo pobreza familiar, desemprego dos pais e baixo nível de escolaridade, e foram criados dois grupos de desvantagem socioeconômica familiar. Foi calculado um índice de risco médico infantil.
ResultadosOs resultados indicaram que as mães de múltiplos prematuros relataram maiores níveis de estresse do que as mães de filhos únicos prematuros. Além disso e especificamente com relação ao funcionamento psicológico, as mães de múltiplos prematuros relataram mais sintomas do que as mães de filhos únicos prematuros, porém apenas quando moravam em um contexto de adversidade socioeconômica.
ConclusõesOs resultados deste estudo possuem importantes implicações para a prática. As mães de múltiplos prematuros apresentam maior risco de dificuldades de saúde mental, em comparação a mães de filhos únicos, principalmente quando expostas a adversidades socioeconômicas. O desenvolvimento de programas de intervenção psicossocial e políticas públicas é de importância decisiva ao ajudar as mães de filhos múltiplos a se ajustarem à maternidade.
Every year, an estimated 15 million babies are born preterm worldwide (<37 gestational weeks) and this number is rising. In Portugal, where this study was conducted, approximately 7.7% of children were born prior to term in 2014, while in 2001 it was about 5.6%.1 Such significant increase constitutes an important public health issue. Indeed, younger and more fragile infants are surviving their neonatal intensive care unit (NICU) stays, with many of them exhibiting high rates of special needs as they grow older.2 Several mental health problems have also been reported for parents. Evidence has revealed that mothers of preterm infants often show elevated stress levels and psychological difficulties, which, in turn, seem to compromise their parenting abilities and, consequently, child development.3 Therefore, more research focused on the impact of medical and social risk factors on parental adjustment is crucial in the field of prematurity.
Research conducted during the last decades has provided a growing body of evidence on the adverse effects of child health risks for parents’ psychological functioning.4 Recently, researchers have been particularly interested in the putative aggravating role of being a mother of multiples. Adding to the stresses of being a parent of a preterm (more fragile) infant, families of preterm multiples are often exposed to additional health and emotional demands, including prolonged hospitalization, child cerebral palsy, hemorrhage, and developmental delays.5,6 Moreover, mothers with multiple gestation pregnancies and their partners have to care for and relate to more than one baby, to whom they may have been separated during their first days after delivery. Such parents often experience more financial pressures, fatigue, social isolation, and practical difficulties that emerge from the need of looking after for more than one infant at once.7 Not surprisingly, researchers have recently revealed that mothers of preterm multiples are more likely to be depressed, to present elevated anxiety, and to experience more parenting stress.8–11
Despite the importance of the findings described above, the research in this field is still characterized by a lack of studies focused on the identification of environmental factors that may buffer the negative effects of multiple births on the psychological well-being of mothers of preterm infants. This gap in the literature is notable, given years of research highlighting the negative impact of family psychosocial adversities on women's psychological functioning. For instance, Goyal et al.12 showed that first time mothers exposed to low socioeconomic status were 11 times more likely than mothers with no socioeconomic risk factors to have clinically elevated depression scores. Although not focused on the role of multiple births, also of note is the work of Wormald et al.13 These investigators analyzed the levels of stress of parents of very low birth weight (VLBW) infants, finding that the mothers of VLBW infants who exhibited significantly higher stress levels were the ones who were exposed, not only to medical complications, but also to more socioeconomic adversities (e.g., lower education, unemployment).
The current studyTaken together, these findings clearly suggest that it is worthwhile to further examine the links between family socioeconomic risks and the adjustment of mothers of preterm multiples. Therefore, this study aimed to investigate the differences between mothers of preterm multiples and mothers of preterm singletons regarding maternal perceived stress and psychological symptoms, and to explore the adverse amplified effect of socioeconomic disadvantage, while controlling for the putative effect of child medical risks. It was hypothesized that mothers of preterm multiples would be at increased risk for higher stress levels and psychological symptoms, in comparison to mothers of preterm singletons, especially (or even exclusively) when living in a context of socioeconomic disadvantage. In other words, the authors expected that the impact of multiple births on the psychological well-being of mothers of preterm infants would be amplified by the adverse effects of socioeconomic disadvantage.
MethodsParticipants and procedureNinety-five mothers of 1-year-old preterm infants participated in this cross-sectional study. Data collection was carried out in two public hospitals from Northern Portugal. This research was previously approved by the Portuguese National Commission for Data Protection, and by the ethical boards of the participating hospitals and of the university involved in the coordination of the study. Mothers were asked to complete two questionnaires to assess maternal psychological symptoms and perceived stress, and reported on socioeconomic factors, child medical risks, and whether or not they had delivered multiples. Mothers signed a written informed consent, permitting their own participation in the study.
MeasuresMaternal perceived stressMothers completed the Portuguese version of the Daily Hassles Questionnaire.14,15 This measure includes 43 items, rated on a 5-point scale (0=no hassle to 4=big hassle), assessing stressors related to daily life and to the activities of parenthood. Items were summed to obtain a final score. In the present study, the internal consistency score for the scale was α=0.94.
Maternal psychological problemsMothers completed the Brief Symptom Inventory (BSI).16,17 The BSI includes 53 items rated on a 5-point scale (0=not at all to 4=extremely), measuring the presence of various symptoms experienced by the mother in the past week. The questionnaire assesses nine psychopathological dimensions and three global scores. The Positive Symptoms Distress Index, one of the global scores, was used in the study, as a measure of symptom intensity corrected for the number of symptoms.
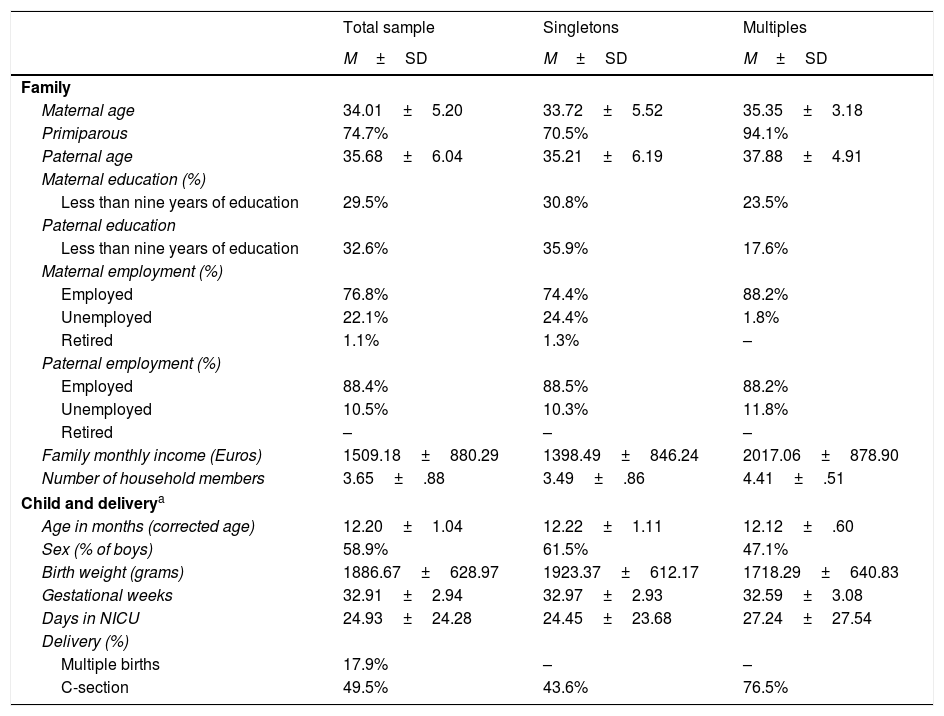
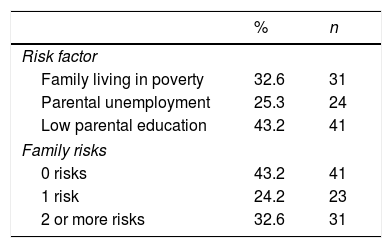
Family socioeconomic disadvantageMothers reported on three socioeconomic risks, namely: (i) family living in poverty (family monthly income, adjusted for family size, below national income levels), (ii) parental unemployment (i.e., one of the parents was unemployed at the time of the study), and (iii) low parental educational level (i.e., one of the parents had under nine years of education). Each risk factor was scored as absent (0) or present (1). Then, the sample was split into two groups of socioeconomic disadvantage: (1) families exposed (to one or more risks, 58.8%), and (2) families not exposed (no risks, 43.2%) to socioeconomic adversities (see Tables 1 and 2 for descriptive statistics on family risks).
Sample characteristics: means±standard deviations.
| Total sample | Singletons | Multiples | |
|---|---|---|---|
| M±SD | M±SD | M±SD | |
| Family | |||
| Maternal age | 34.01±5.20 | 33.72±5.52 | 35.35±3.18 |
| Primiparous | 74.7% | 70.5% | 94.1% |
| Paternal age | 35.68±6.04 | 35.21±6.19 | 37.88±4.91 |
| Maternal education (%) | |||
| Less than nine years of education | 29.5% | 30.8% | 23.5% |
| Paternal education | |||
| Less than nine years of education | 32.6% | 35.9% | 17.6% |
| Maternal employment (%) | |||
| Employed | 76.8% | 74.4% | 88.2% |
| Unemployed | 22.1% | 24.4% | 1.8% |
| Retired | 1.1% | 1.3% | – |
| Paternal employment (%) | |||
| Employed | 88.4% | 88.5% | 88.2% |
| Unemployed | 10.5% | 10.3% | 11.8% |
| Retired | – | – | – |
| Family monthly income (Euros) | 1509.18±880.29 | 1398.49±846.24 | 2017.06±878.90 |
| Number of household members | 3.65±.88 | 3.49±.86 | 4.41±.51 |
| Child and deliverya | |||
| Age in months (corrected age) | 12.20±1.04 | 12.22±1.11 | 12.12±.60 |
| Sex (% of boys) | 58.9% | 61.5% | 47.1% |
| Birth weight (grams) | 1886.67±628.97 | 1923.37±612.17 | 1718.29±640.83 |
| Gestational weeks | 32.91±2.94 | 32.97±2.93 | 32.59±3.08 |
| Days in NICU | 24.93±24.28 | 24.45±23.68 | 27.24±27.54 |
| Delivery (%) | |||
| Multiple births | 17.9% | – | – |
| C-section | 49.5% | 43.6% | 76.5% |
A child medical risk index was calculated to serve as covariate, consisting of the mean of standardized scores of child gestational weeks (reversed), birth weight (reversed), and number of days in the NICU. A higher score is indicative of greater medical risk.
Data analysisData were analyzed using the Statistical Package for Social Sciences software (SPSS) (IBM Corp., Released 2013, IBM SPSS Statistics for Windows, version 22.0k, NY, USA). Descriptive statistics for maternal perceived stress and psychological symptoms were first examined for the total sample. Then, independent t-tests and chi-squared tests were used to determine whether mothers of preterm multiples and mothers of preterm singletons were different with respect to maternal age, child medical risks, and family socioeconomic disadvantage. Differences between mothers exposed and mothers not exposed to socioeconomic disadvantage were also examined with respect to maternal age and child medical risks. Further analyses were conducted using two-way multivariate analysis of variance (MANOVA) to test group differences in maternal perceived stress and psychological symptoms, while controlling for child medical risks. Interaction effects were also explored.
ResultsSample characteristics are presented in Tables 1 and 2. At time of assessment, mothers were aged 19–48 years (34.01±5.20). Seventy-two were primiparous and 17 were mothers of multiples (all twins, except one mother of triplets). In the majority of cases, the pregnancy was planned (82.1%), medically monitored (96.8%), and infants were delivered vaginally (50.5%). The majority of mothers were married (91.6%). The remaining were single (6.3%) or divorced (2.1%). Regarding maternal education, three mothers had four years of formal education, 25 had five to nine years, 30 had ten to 12 years, and the remaining had a college degree. Seventy-three mothers had a job, 21 were unemployed, and one mother was retired. Moreover, 31 (32.6%) families were living with incomes below the national poverty line.
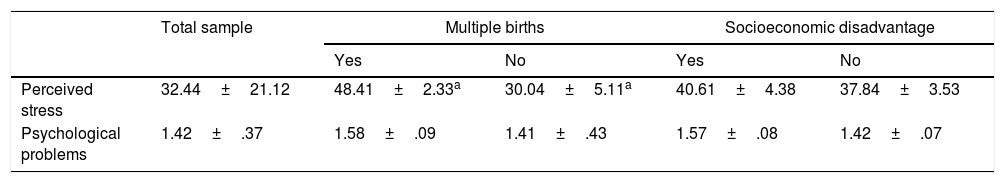
For the total sample, mothers’ mean perceived stress was 32.44±21.12, while the mean of psychological symptoms was 1.42±.37 (Table 3). Analyses showed that mothers of preterm multiples and mothers of preterm singletons were not significantly different in any of the following demographic and study variables: maternal age, t(93)=−1.18, p=0.24; child medical risks, t(93)=−0.45, p=0.66; or family socioeconomic disadvantage, χ2=3.91, p=0.06. Likewise, mothers exposed and mothers not exposed to socioeconomic disadvantage did not differ in terms of child medical risks, t(93)=0.90, p=0.37; however, mothers living in a context of socioeconomic disadvantage were significantly older, t(93)=2.35, p=0.02.
Group differences in maternal perceived stress and psychological problems: means±standard deviations.
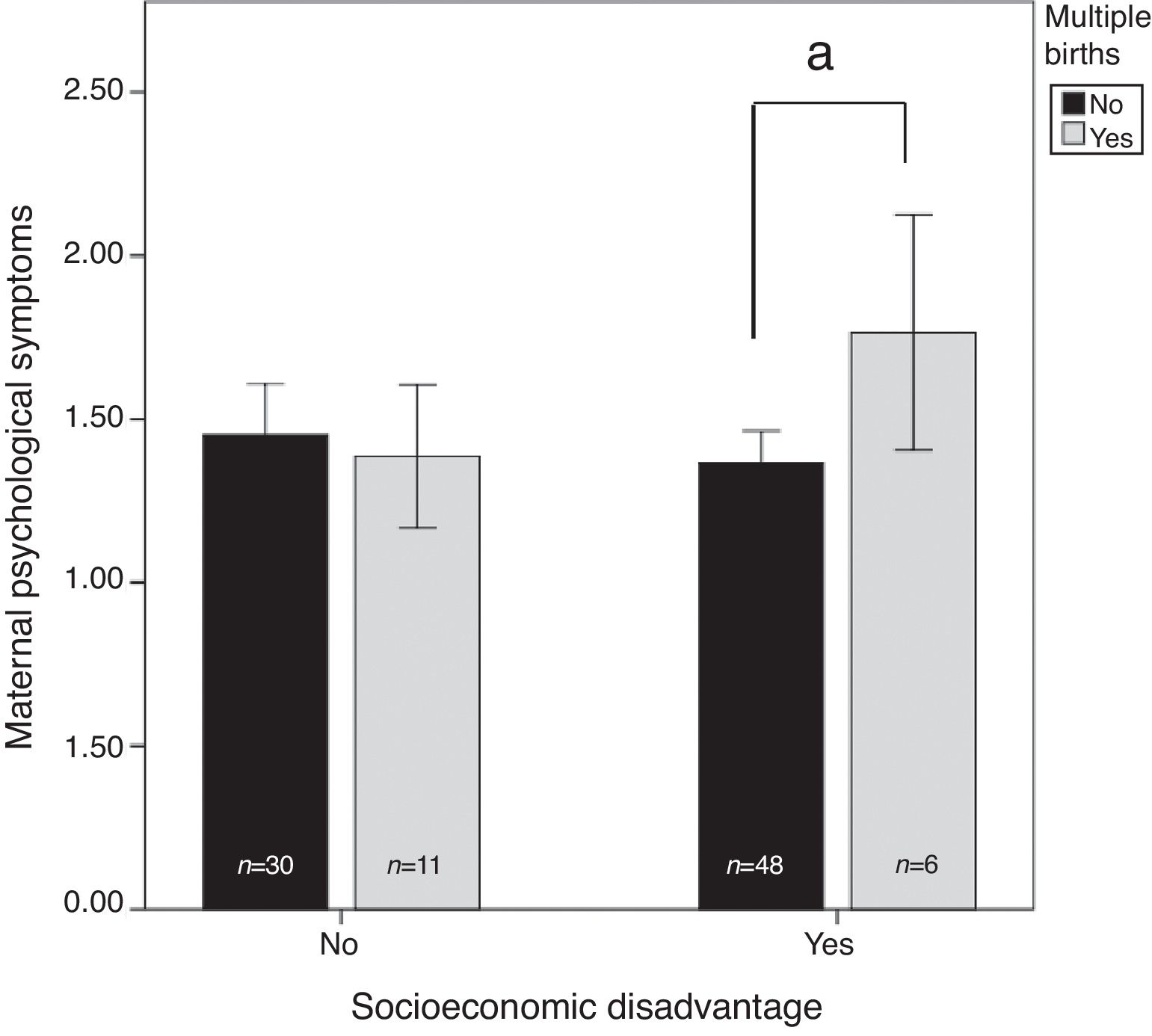
Then, two-way MANOVA was performed. Multiple births and family socioeconomic disadvantage were included in the analysis as factors, while child medical risk was entered as a covariate. Data entered into the MANOVA satisfied the requirements for homogeneity of covariance matrices (Box's test, p=0.12) and equality of variances for each dependent variable (Levene's tests: for perceived stress, p=0.11; for psychological problems, p=0.93). The main results revealed a statistically significant principle effect of multiple births on the combined dependent variable, F(1,95)=5.25, p=0.007, Wilks’ Λ=0.89. Further examination of this result indicated that mothers of preterm multiples reported higher levels of stress than mothers of preterm singletons, F(1,95)=10.70, p=0.002, Eta2=0.11. No significant differences were observed between mothers exposed and unexposed to socioeconomic disadvantage (Table 3). However, there was a marginally significant multiple births vs. socioeconomic status effect on the combined dependent variables, F(1,95)=2.75, p=0.06, Wilks’ Λ=0.94. Given this tendency, between-subjects effects were then examined. Results indicated that the impact of multiple births on maternal psychological problems (but not levels of stress) differ whether mothers were exposed (vs. unexposed) to socioeconomic adversities, F(1,95)=5.25, p=0.02, Eta2=0.055. More specifically, simple effects analysis revealed that, in the context of socioeconomic disadvantage, mothers of preterm multiples significantly reported more psychological symptoms (1.77±0.33) than mothers of preterm singletons (1.37±0.34). However, in the absence of socioeconomic adversities, mothers of preterm multiples (1.39±0.33) and mothers of singletons (1.45±0.42) reported similar levels of psychological problems (Fig. 1).
DiscussionThe present study aimed to examine the differences between mothers of preterm multiples and mothers of preterm singletons with respect to perceived stress and maternal psychological symptoms, while controlling for the effect of child medical risks. As expected, the results revealed that mothers of preterm multiples experienced significantly higher stress levels than mothers of preterm singletons months after delivery, when their children were 12 months of corrected age. It is important to highlight that this result is in line with previous studies, which have also shown, consistently, that mothers of multiples are significantly more likely than mothers of singletons to report severe parenting stress, not only days after delivery, but also months after giving birth.11,18
Surprisingly, no significant differences emerged between groups with respect to maternal psychological symptoms in the present study. This data is consistent with other studies that have also failed to document differences between mothers of multiples and mothers of singletons in psychological functioning. For instance, Glazebrook et al.19 found that mothers of multiples did not have poorer mental health than mothers of singletons, one year postpartum. Nevertheless, the present results differ from other research that, on the contrary, indicated the presence of elevated psychological difficulties among mothers of preterm multiples.9,10 Such divergent results across studies may be attributable to methodological issues. More precisely, in the present investigation, as well as in the work of Glazebrook et al.,19 maternal mental health was assessed using global reports of psychological functioning, while in other studies researchers have relied on measures aimed to specifically assess maternal levels of anxiety or depression.20 In addition to this possibility, it may also be the case that maternal psychological difficulties may be more salient in the very first days or months after giving birth, during a period when the mother is still adapting to the role of being a parent of two or more fragile children. Accordingly, Van den Akker et al.,21 in a meta-analysis, concluded that maternal depression was more common before the end of one year postpartum. On the contrary, in the present study assessments occurred one year after delivery. However, it is unclear whether any of these explanations is responsible for the results reported herein. Future studies, longitudinal in design, are clearly needed.
Adding to the above research aims, this report also sought to innovate and extend the current literature by exploring the putative amplifying adverse effect of socioeconomic disadvantage on the relation between multiple preterm births and maternal adjustment. Data showed that mothers of preterm multiples significantly reported more psychological symptoms than mothers of singletons, but only when exposed to socioeconomic adversities. This result clearly points to the relevance of parental socioeconomic background for women's adjustment, as previously suggested by other studies.12,13 However, and most importantly, these results may help to clarify the inconsistencies found in the literature about the emergence of psychological symptoms among mothers of preterm multiples, as discussed in the preceding paragraph. More precisely, this study expands previous literature by suggesting that the birth of multiples does not necessary adversely impacts women's mental health. Instead, it may be the case that the negative impact of multiple births on the psychological functioning of women occurs when mothers are, simultaneously, exposed to a context of social disadvantage. Such adversity will prevent families from obtaining the resources and support needed to adequately care for and relate to more than one small, fragile infant at once.
Importantly, these findings also revealed that the elevated susceptibility of mothers of preterm multiples to show adjustment problems, more than one year postpartum, seems to occur even after controlling for the putative effect of child medical risks. In fact, it is worth bearing in mind that no significant associations emerged, in the current report, between child risks at birth and maternal perceived stress and psychological problems. This lack of a significant effect is not in line with other studies.4 However, this does not necessarily mean that child medical adversities have no implications on the well-being and maternal psychological functioning. Perhaps other child factors may be more prominent one year postpartum, such as the presence of neurological dysfunctions, as already evidenced by Walter et al.22 On this subject, more studies are needed.
Implications for policy and practiceTaken together, these results are notable and have important implications for practice. As already mentioned, in recent years, there has been a rise in the number of premature births, but also in the number of multiple pregnancies in many developed countries, mostly due to advances in assisted reproductive technology and to older maternal age at childbirth.23 For instance, data collected for the years 2004 and 2010, in 29 European countries as part of the Euro-Peristat project, revealed that the twinning rate increased on average by 1.7% units (i.e., more than 12.5%) over that six-year period.24 The present data, together with the results of other studies,9-11 suggest that mothers of preterm multiples may be at-risk for severe adjustment problems, particularly when exposed to socioeconomic disadvantage. Healthcare programs should incorporate comprehensive psychological assessments of mothers of children born preterm, specifically for mothers of multiples, not only immediately after birth, but also in the months and years to come. They should also incorporate supportive services and effective, more individualized psychosocial interventions for such mothers (and their partners) in the postnatal period. Policy makers should additionally be informed that by improving the emotional well-being of mothers and their partners, they will also be stimulating and caring for the health and optimal development of children.
LimitationsThere are several limitations to this report that should be addressed in future research. The sample is small, and, thus, this study is limited in its statistical power. In addition, as a cross-sectional study, information regarding the main study variables was available for a single point in time. Thereby, the correlation design of this study limits the exploration of the mechanisms putatively involved in the emergence of elevated stress levels and psychological difficulties in mothers of multiples exposed to socioeconomic disadvantage. The trajectories of maternal adjustment were also not possible to examine. Moreover, future studies should incorporate the assessment of child neurological problems as a potential predictor of maternal lower adjustment, and should consider the evaluation of fathers’ adjustment as well.
Despite the dramatic increase in twin births in much of the Western world, it is striking that little research has sought to examine mental health in parents of multiples. Thus, the present study aimed to expand the current knowledge about the adjustment of mothers of preterm multiples, most notably by exploring the differences between mothers of preterm multiples and mothers of preterm singletons with respect to perceived stress and psychological symptoms, one year postpartum. It also sought to examine the putative negative effect of maternal exposure to socioeconomic disadvantage. Data revealed that mothers of preterm multiples showed elevated stress levels, in comparison to mothers of preterm singletons. Regarding psychological functioning, mothers of preterm multiples reported significantly more symptoms than mothers of preterm singletons, but only when living in a context of socioeconomic adversity. These findings not only suggest that having a preterm (more fragile) infant, in the context of multiple births, is a considerable challenge for many parents, but also that the care giving and psychological demands that derive from it seem to be exacerbated by the exposure of the family to socioeconomic adversities. Future work should include the development of psychosocial treatments to assist parents of preterm multiples, especially those who are exposed to a context of social disadvantage, and who may ultimately benefit the most from supportive interventions.
FundingFundação para a Ciência e a Tecnologia (SFRH/BPD/100994/2014, SFRH/BD/86075/2012).
Conflicts of interestThe authors declare no conflicts of interest.
The authors are very grateful to the children and parents who participated in the study.
This study was conducted within the Psychology Research Center, University of Minho, and partially supported by the Portuguese Foundation for Science and Technology (SFRH/BPD/100994/2014 assigned to the first author; also grant SFRH/BD/86075/2012) and by the Portuguese Ministry of Education and Science through national funds and when applicable co-financed by European Regional Development Fund (ERDF) under the PT2020 Partnership Agreement (UID/PSI/01662/2013).
Please cite this article as: Baptista J, Moutinho V, Mateus V, Guimarães H, Clemente F, Almeida S, et al. Being a mother of preterm multiples in the context of socioeconomic disadvantage: perceived stress and psychological symptoms. J Pediatr (Rio J). 2018;94:491–7.