To analyze the level of sedation in intubated children as a risk factor for the development of subglottic stenosis.
MethodsAll patients between 30 days and 5 years of age who required endotracheal intubation in the pediatric intensive care unit between 2013 and 2014 were included in this prospective study. They were monitored daily and COMFORT-B scores were obtained. Flexible fiber-optic laryngoscopy was performed within eight hours of extubation, and repeated seven to ten days later if the first examination showed moderate to severe laryngeal injuries. If these lesions persisted and/or if the child developed symptoms in the follow-up period, microlaryngoscopy under general anesthesia was performed to evaluate for subglottic stenosis.
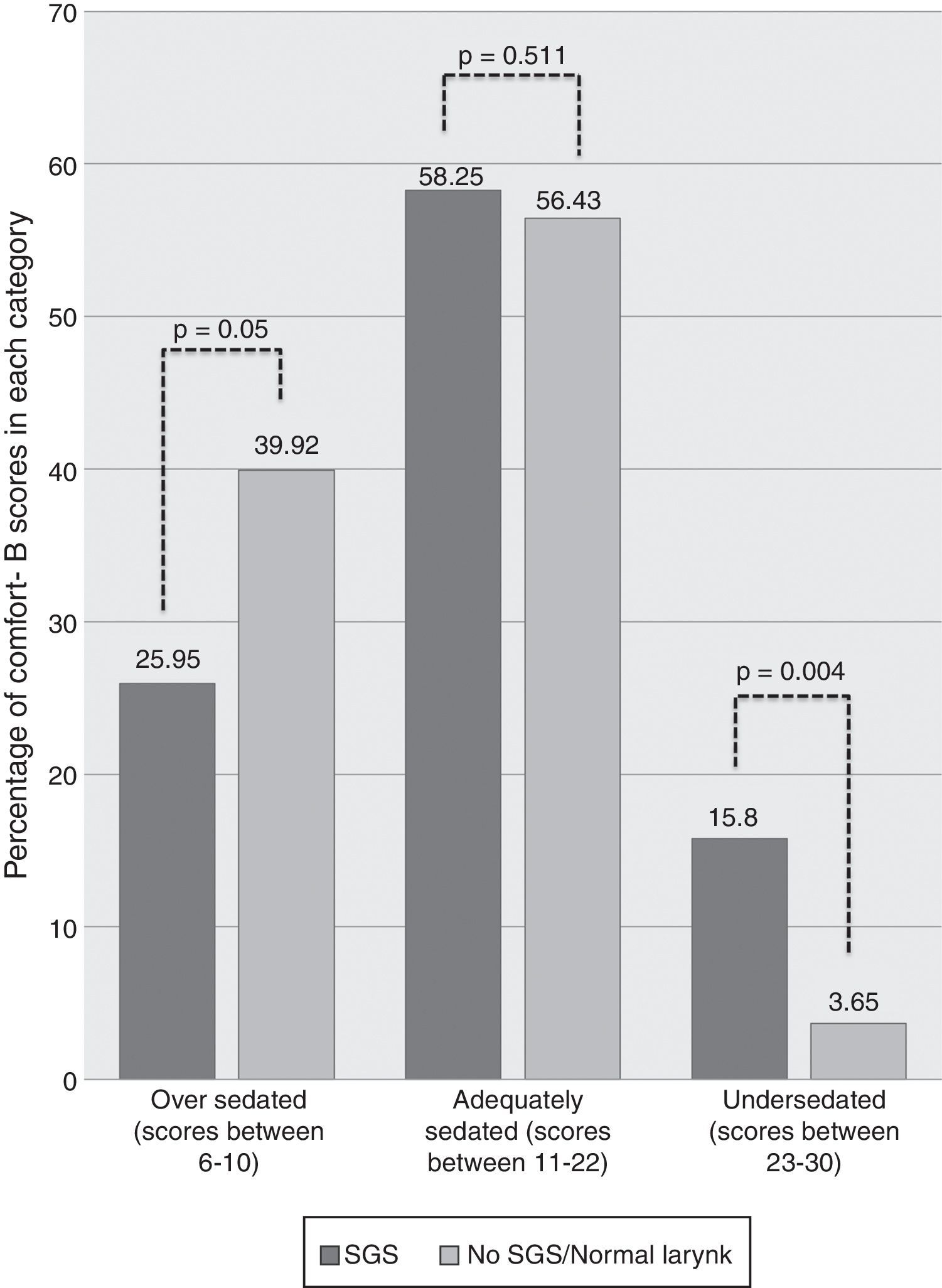
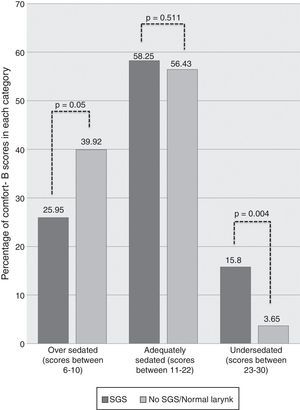
ResultsThe study included 36 children. Incidence of subglottic stenosis was 11.1%. Children with subglottic stenosis had a higher percentage of COMFORT-B scores between 23 and 30 (undersedated) than those who did not develop subglottic stenosis (15.8% vs. 3.65%, p=0.004).
ConclusionChildren who developed subglottic stenosis were less sedated than children who did not develop subglottic stenosis.
Analisar o nível de sedação em crianças intubadas como um fator de risco para o desenvolvimento de estenose subglótica (ES).
MétodosTodos os pacientes entre 30 dias e 5 anos de idades que necessitaram de intubação endotraqueal na Unidade de Terapia Intensiva Pediátrica entre 2013 e 2014 foram incluídos neste estudo prospectivo. Eles foram monitorados diariamente e foram obtidos os escores da escala COMFORT-B. Foi feita laringoscopia com tubo flexível de fibra óptica em 8 horas da extubação e repetida 7-10 dias depois, caso o primeiro exame tenha mostrado lesões laríngeas moderadas a graves. Caso essas lesões tenham persistido e/ou caso a criança tenha desenvolvido sintomas no período de acompanhamento, foi feita microlaringoscopia sob anestesia geral para avaliar a ES.
ResultadosIncluímos 36 crianças. A incidência da ES foi de 11,1%. As crianças com ES apresentaram um maior percentual de escores da escala COMFORT-B entre 23 e 30 (subsedados) que os que não desenvolveram ES (15,8% em comparação a 3,65%, p=0,004).
ConclusãoAs crianças que desenvolveram ES foram menos sedadas que as crianças que não desenvolveram ES.
Acquired subglottic stenosis (SGS) is most commonly a consequence of prolonged endotracheal intubation, with a reported incidence of 2.8–11.3%.1–3 There are several risk factors already under consideration; however, there are only a few studies with sufficiently adequate design to ascertain its association.
While previous publications have suggested that inadequate sedation is a risk factor for the development of SGS,4,5 these studies were either expert opinions or retrospective reviews with no control group. The proposed mechanism of injury is that the agitation of the child could cause excessive movement of the endotracheal tube (ETT) in the airway, predisposing to laryngeal stenosis.
In 2007, a study from the present research group enrolling 35 pediatric patients showed that the number of additional doses of sedation that the child received during the intubation period was a risk factor for SGS.6 Later, another article by the same group including 142 children confirmed that the number of extra doses of sedation was effectively a risk factor, and also identified prolonged intubation time as a significant predictor of the development of SGS. However, solely from the data collected, it could not be concluded whether the reason for the larynx injury was trauma because of the child's excessive agitation, or hypoperfusion and local ischemia because of excessive sedation, which, along with the trauma due to the ETT in contact with the airway mucosa, culminated in the development of SGS.7
In order to clarify this issue in children beyond the neonatal period, the authors conducted research in the pediatric intensive care unit (PICU) of this hospital, collecting data regarding the sedation of patients. The aim of this study was therefore to verify if there is any association between the degree of sedation during the intubation period and the development of SGS after extubation.
MethodsThis was a prospective cohort study that included all children from 30 days to 5 years of age who were intubated in the PICU of Hospital de Clínicas de Porto Alegre (HCPA), between 2013 and 2014, and whose parents or guardians agreed to participate by signing an informed consent. Patients were excluded if they had signs of previous laryngeal disease, such as dysphonia and stridor, prior intubation, current or past tracheostomy, craniofacial malformations, or children in poor general condition. The protocol was approved by the Research and Ethics Committee of HCPA.
Intubation procedures followed a protocol of fast intubation sequence, with the use of midazolam, fentanyl, and rocuronium. Children were then sedated with midazolam 0.2mg/kg/h and fentanyl 2mcg/kg/h during the entire intubation period. All extra sedative medication doses were considered “additional doses of sedation.”
All children were monitored daily in the PICU after intubation, and data such as number of additional sedation doses received, number of days intubated, need for reintubation, and need for ETT repositioning were collected. The size of the ETT was determined by guidelines from the American Heart Association.8 Verification of tube size adequacy is performed by evaluating the difference of inspiratory and expiratory tidal volumes, as measured by the PICU assistant; tube size is considered adequate when there is a difference of around 20–25% between the two measured volumes. If the difference is greater than that, then PICU staff upsize the ETT. If the difference is smaller, they downsize it.
In 2013, the application of the COMFORT-B sedation scale was implemented at the PICU of HCPA in order to measure the level of sedation and to assist in evaluating the need for additional doses of sedation. Nurses who had been previously trained applied this scale every three hours. It evaluates items such as level of consciousness, calmness/agitation, respiratory response, physical movement, muscle tone, and facial tension.9
Patients underwent flexible fiber-optic laryngoscopy (FFL) in the PICU within eight hours after extubation, with nasal topical anesthesia and without sedation. All children used supplemental oxygen due to the recent extubation. The patients were positioned, and oxygen saturation and heart rate were monitored throughout the examination. The examinations were recorded and later examined by a blinded reviewer, who classified them in Group 1 – no laryngeal injuries or mild injuries, or Group 2 – moderate to severe laryngeal lesions, according to a criteria previously published by the authors.1
All children were followed-up after discharge from the PICU. Those with moderate to severe lesions on the initial post-extubation FFL, and any additional children with laryngeal symptoms during follow-up, underwent a second FFL seven to ten days after extubation, and were followed up further. Those with persistent laryngeal lesions received subsequent microlaryngoscopy to evaluate for possible SGS.
Families were asked to bring their children exclusively to the research medical staff whenever respiratory symptoms developed. None of the patients had a diagnosis of SGS established without microlaryngoscopy being performed.
Patients were then divided into two final groups: those who developed SGS and those who did not. Children in the SGS group were enrolled in a follow-up program and were treated by the otolaryngology team.
The program Predictive Analytics Software (PASW) version 17.0.2 (Somers, NY, USA) was used for statistical analysis. Quantitative variables were expressed as mean±SD when they had normal distribution. Otherwise, they were described as median, 25th and 75th percentiles, as well as minimum and maximum values. The Mann–Whitney U-test was used for calculating the difference between the groups. Categorical variables were expressed as number of patients (n) and percentage (%). Fisher's exact test with chi-squared distribution was used to calculate the difference between the proportions. For calculation of the 95% confidence interval (95% CI), the Wilson score method was used.
ResultsDuring the two-year period of research in PICU, 45 children were eligible for the study. Of these, nine children were not included because their parents refused to participate (two children), they underwent tracheostomy for prolonged mechanical ventilation (three children), died before extubation (two children), or died after the initial assessment (two children). Thus, there was an eventual loss of 20% of patients, and 36 children were included.
The median age of the included children was 2.6 months (25th–75th percentiles: 1.9–7.2) and 50% (18) were male.
In the initial FFL, 16 children (44.4%) had moderate to severe injuries. The incidence of SGS at the end of follow-up was 11.1% (four children; 95% CI, 4.17–29.60).
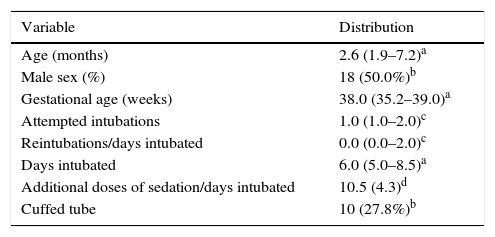
Data regarding population characteristics are presented in Table 1.
Population characteristics (n=36).
| Variable | Distribution |
|---|---|
| Age (months) | 2.6 (1.9–7.2)a |
| Male sex (%) | 18 (50.0%)b |
| Gestational age (weeks) | 38.0 (35.2–39.0)a |
| Attempted intubations | 1.0 (1.0–2.0)c |
| Reintubations/days intubated | 0.0 (0.0–2.0)c |
| Days intubated | 6.0 (5.0–8.5)a |
| Additional doses of sedation/days intubated | 10.5 (4.3)d |
| Cuffed tube | 10 (27.8%)b |
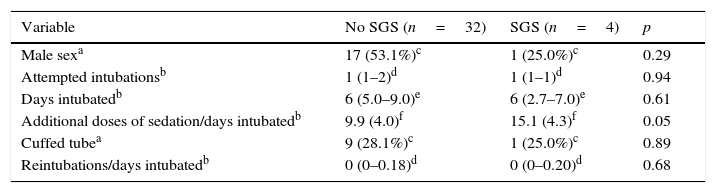
Data regarding other possible risk factors, including the number of days of intubation, additional doses of sedation/days of intubation, number of intubations/days of intubation, and the presence of a cuffed tube, are presented in Table 2. Univariate analysis showed no statistically significance for these variables.
Analysis of isolated risk factor for subglottic stenosis (n=36).
| Variable | No SGS (n=32) | SGS (n=4) | p |
|---|---|---|---|
| Male sexa | 17 (53.1%)c | 1 (25.0%)c | 0.29 |
| Attempted intubationsb | 1 (1–2)d | 1 (1–1)d | 0.94 |
| Days intubatedb | 6 (5.0–9.0)e | 6 (2.7–7.0)e | 0.61 |
| Additional doses of sedation/days intubatedb | 9.9 (4.0)f | 15.1 (4.3)f | 0.05 |
| Cuffed tubea | 9 (28.1%)c | 1 (25.0%)c | 0.89 |
| Reintubations/days intubatedb | 0 (0–0.18)d | 0 (0–0.20)d | 0.68 |
SGS, subglottic stenosis.
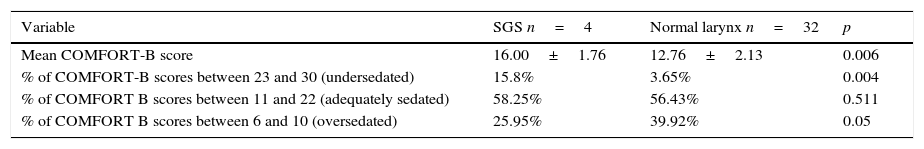
Children who developed SGS had a mean COMFORT-B score of 16.00±1.76, while the mean COMFORT-B score of those who did not develop SGS was 12.76±2.13, with a statistically significant difference (p=0.006). Children with SGS had a higher percentage of COMFORT-B scores between 23 and 30 than those who did not develop SGS (15.8% vs. 3.65%, p=0.004). Data are shown in Table 3 and Fig. 1.
COMFORT-B scores: comparison between the two groups (n=36).
| Variable | SGS n=4 | Normal larynx n=32 | p |
|---|---|---|---|
| Mean COMFORT-B score | 16.00±1.76 | 12.76±2.13 | 0.006 |
| % of COMFORT-B scores between 23 and 30 (undersedated) | 15.8% | 3.65% | 0.004 |
| % of COMFORT B scores between 11 and 22 (adequately sedated) | 58.25% | 56.43% | 0.511 |
| % of COMFORT B scores between 6 and 10 (oversedated) | 25.95% | 39.92% | 0.05 |
SGS, subglottic stenosis.
Owing to the complexity of SGS management and the associated morbidity, it is important to identify risk factors associated with its development. There are few prospective studies on this subject, and most of them were held in neonatal intensive care units.10,11
The authors’ previous studies identified the duration of intubation7 and number of additional doses of sedation received by the child6,7 as risk factors for SGS. The number of reintubation attempts and the use of a cuffed tube were not considered significant.
Sedation was mentioned in some articles as a potential factor for the development of SGS,4,7 although to date this association has not been characterized, because no prospective study has targeted this question directly.
The ideal approach for assessing the degree of sedation of patients is to use existing standard scales. Sedation scales have been increasingly used in pediatric intensive care units to guide the administration of sedatives, evaluating the need to increase the dose of the basal sedation and the need to administer extra doses of sedation.12
The COMFORT-B scale is widely used in studies assessing children's sedation levels and it has proven to be adequate for the management of intubated children in mechanical ventilation.9,13 This scale was validated for the Portuguese language by Amoretti et al., in 2008.14 A recent study showed that the COMFORT-B scale also detects treatment-related changes in pain or distress intensity, and can effectively be used to guide sedation treatment in critically ill children.15
The results of the present study show that children who developed SGS are potentially those that are undersedated in the PICU, which was confirmed by two variables: “mean COMFORT-B score” and “percentage of COMFORT-B scores between 23 and 30 (undersedated children).” Due to restlessness, these children required more doses of additional sedation, i.e., doses beyond those prescribed routinely by an intensive care team. This explains the findings in previous studies, in which the number of additional doses of sedation systematically emerged as an independent risk factor for SGS.6,7
The lack of sedation and the consequent movement of the ETT in the airway have been already cited by experts in the field of pediatric laryngology as risk factors for SGS,16,17 but this is the first prospective study with objective measures of the level of sedation to prove this fact in the pediatric population.
This study failed to demonstrate “days intubated” and “number of additional doses of sedation/days intubated” as significant risk factors, probably because of the limited number of patients. However, these factors were already proved to be significant in the previous studies published.
It is paradoxical that currently the etiology of most SGS is endotracheal intubation, but on the other hand that the ETT itself is indicated by experts to treat acute injuries after intubation, serving as a stent for the healing of glottic and subglottic injuries.15 It could be inferred, therefore, that the problem is probably not the tube itself – considering that this is of the proper size for the child – but the child's excessive movement and the length of time the tube remains in the airway.
In conclusion, in this prospective study including only children beyond the neonatal period, children who developed SGS were less sedated during the time they needed an ETT than children who did not develop SGS, as measured by the COMFORT-B scale.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Schweiger C, Manica D, Pereira DR, Carvalho PR, Piva JP, Kuhl G, et al. Undersedation is a risk factor for the development of subglottic stenosis in intubated children. J Pediatr (Rio J). 2017;93:351–5.
This study was performed in the Hospital de Clínicas de Porto Alegre, Unidade de Terapia Intensiva Pediátrica, Porto Alegre, RS, Brazil.