To evaluate the association between early treatment and urodynamic improvement in pediatric and adolescent patients with neurogenic bladder.
MethodologyRetrospective longitudinal and observational study (between 1990 and 2013) including patients with neurogenic bladder and myelomeningocele treated based on urodynamic results. The authors evaluated the urodynamic follow-up (bladder compliance and maximum bladder capacity and pressure) considering the first urodynamic improvement in two years as the outcome variable and early referral as the exposure variable, using a descriptive and multivariate analysis with logistic regression model.
ResultsAmong 230 patients included, 52% had an early referral. The majority were diagnosed as overactive bladder with high bladder pressure (≥40cm H2O) and low bladder compliance (3mL/cmH2O) and were treated with oxybutynin and intermittent catheterization. Urodynamic follow-up results showed 68% of improvement at the second urodynamic examination decreasing bladder pressure and increasing bladder capacity and compliance. The percentage of incontinence and urinary tract infections decreased over treatment. Early referral (one-year old or less) increased by 3.5 the probability of urodynamic improvement in two years (95% CI: 1.81–6.77).
ConclusionTreatment onset within the first year of life improves urodynamic prognosis in patients with neurogenic bladder and triplicates the probability of urodynamic improvement in two years. The role of neonatologists and pediatricians in early referral is extremely important.
Avaliar a associação entre tratamento precoce e melhora urodinâmica em pacientes pediátricos e adolescentes portadores de bexiga neurogênica.
MetodologiaEstudo observacional longitudinal retrospectivo (entre 1990-2013) em pacientes com bexiga neurogênica e mielomeningocele tratados com base no diagnóstico urodinâmico. Avaliamos a evolução urodinâmica (complacência, capacidade e pressão vesical) considerando primeira melhora urodinâmica em até dois anos como variável desfecho e encaminhamento precoce (primeira urodinâmica até um ano de vida) como exposição. Foi realizada análise descritiva e multivariada com modelo de regressão logística.
ResultadosEntre 230 pacientes incluídos 52% foram encaminhados precocemente. A maioria tinha bexiga hiperativa com pressão maior que 40cmH2O, complacência abaixo de 3ml/cmH2O e foitratadacom oxibutinina e cateterismo intermitente. Na evolução urodinâmica, 68% apresentou melhora já no segundo exame com redução da pressão e aumento da capacidade e da complacência vesical. O percentual de incontinência e infecção urinária diminuiu ao longo do tratamento. O encaminhamento precoce aumentou 3,5 vezes a probabilidade de melhora urodinâmica até dois anos em relação aos encaminhados após o primeiro ano de idade (CI95% 1,81-6,77).
ConclusãoTratar no primeiro ano de vida melhora o prognóstico urodinâmico de pacientes com bexiga neurogênica, triplicando a probabilidade de melhora urodinâmica em até dois anos. A atuação do neonatologista e do pediatra, reconhecendo e encaminhando o paciente precocemente para o diagnóstico é extremamente importante.
Chronic kidney disease (CKD) is a worldwide public health problem.1 Evidence has confirmed the increase in cases, with millions of individuals being treated by renal replacement therapy – dialysis or kidney transplantation. Its prevalence in the world's population exceeds 10% and may reach 50% in high-risk subpopulations,2 including patients with neurogenic bladder,3 a neurological dysfunction of the lower urinary system that changes the phases of filling and emptying of the bladder. Neural tube congenital malformations, such as myelomeningocele, are the most frequent causes of neurogenic bladder in childhood. At least 25% of the most severe symptoms in pediatric urology are associated with neurogenic bladder.4 Approximately 40% of children with neurogenic bladder develop some degree of renal impairment.5
The appropriate process of urination depends on the synergy between the bladder and the urinary sphincter complex. This allows the bladder to remain relaxed and under low pressure during the filling phase, which characterizes bladder compliance. The emptying phase begins when the bladder capacity is reached, which generates a contraction of the bladder with elevation of the intravesical pressure, ideally up to 40cmH2O, accompanied by sphincter relaxation, allowing complete emptying without post-void urinary residue.
The main risk factors for renal impairment related to the diagnosis of neurogenic bladder are increased pressure, reduced bladder capacity and compliance, detrusor sphincter dyssynergia, and post-void residue. To reduce renal morbidity, it is necessary to identify and treat these risk factors as early as possible. The urodynamic evaluation is recognized as the gold standard diagnostic method,6–9 because it is the only examination capable of safely identifying these risk factors, assessing the coordination and pressure variations between the bladder, urethra, and sphincter complex and the integration between the bladder filling and emptying phases, identifying the causes of dysfunction, and guiding the appropriate treatment and follow-up of the disease.
The assessment of the evolution of patients with neurogenic bladder based on clinical criteria and diagnostic imaging, as seen in most publications, is of utmost importance. However, the present study focused on prevention, with the follow-up based on the improvement of urodynamic indicators, which notoriously represent risk factors for renal impairment. This service has been recommending early diagnosis and treatment for two decades, considering the evaluation of patient evolution based on urodynamic improvement and, consequently, on the reduction of kidney failure associated with neurogenic bladder.
This study aimed to evaluate the association between early treatment and urodynamic improvement of patients with neurogenic bladder in a pediatric hospital.
MethodsThis was a retrospective, longitudinal, observational study of pediatric and adolescent patients with neurogenic bladder treated between 1990 and 2013 at the Pediatric Urodynamic and Urinary Dysfunction Outpatient Clinic of Instituto Fernandes Figueira/FIOCRUZ. After approval by the Research Ethics Committee (CEP-IFF, Opinion 281,768), the medical records were selected through an active search in the Medical Documentation and Archive Service. The inclusion criteria for the search were: referral to the service between 1990 and 2013 with a diagnosis of myelomeningocele and neurogenic bladder (ICD Q05 and N31.9). All eligible patients were included.
Treatment was indicated based on the initial urodynamic diagnosis performed after myelomeningocele correction. Oxybutynin was indicated for the control of overactive bladder and low bladder compliance, when maximum bladder pressure was ≥40cmH2O.
Intermittent catheterization was indicated when bladder emptying was ineffective. Nocturnal catheterization was indicated for patients with recurrent urinary tract infections, renal and urinary tract evolution worsening at the ultrasound (US; onset or worsening of hydronephrosis), presence of grade 4 and 5 vesicoureteral reflux, very elevated urodynamic pressure levels, and renal function deterioration.10 The use of antibiotics was indicated for treatment in urinary tract infections confirmed clinically and through laboratory exams, according to the susceptibility test, as well as a prophylactic measure, according to the clinical and laboratory history of recurrent urinary tract infections.
The evolution analysis was based on the results of urodynamic exams performed subsequently, at intervals of six months to one year, depending on the severity observed at the first examination. Consequently, for this study, the date of the first urodynamic evaluation was considered as “point zero”. On this occasion, the initial bladder behavior was classified into one of four categories: normal bladder (relaxed during filling, sustained bladder contraction upon reaching maximum capacity with relaxed sphincter, complete emptying without post-void residue); underactive bladder (incapable of generating or sustaining contraction that allowed bladder emptying); overactive bladder (detrusor contractions during filling, elevated intravesical pressures, and early emptying before reaching maximum bladder capacity) and low bladder compliance (loss of bladder capacity to remain relaxed during filling, progressive increase in intravesical pressure, elevated bladder pressures, and early emptying). Overactive bladder and low bladder compliance are at-risk urodynamic diagnoses.
At the subsequent urodynamic assessments, when the bladder showed normalization during the evolution in response to the treatment received, the term “compensated bladder” was used. The collected urodynamic variables were: maximum bladder pressure, loss pressure, bladder capacity in relation to the expected capacity for age, and bladder compliance.
Regarding the clinical history, the following symptoms related to the urinary system were observed: presence, degree, and time of urinary continence, as well as episodes of urinary tract infection and bacteriuria.
All urodynamic evaluations were reviewed by specialists. From the urodynamic evolution standpoint, urodynamic improvement was considered in relation to the previous examination when there was reduction in pressure levels (maximum bladder pressure and loss pressure), increase in bladder capacity and bladder compliance, and reduction in the frequency of unconstrained detrusor contractions, in cases of overactive bladder. The study outcome was the first urodynamic improvement in up to two years of treatment; early referral, defined as the referral in up to one year of life, was considered the exposure variable.
Treatment adherence was also assessed and determined based on information present in the medical records, considering attendance to scheduled appointments and examinations, continuous use of prescribed medication, and intermittent catheterization as indicated throughout the disease evolution.
A collection form and a database were specifically developed for the study. The studied variables were selected based on the search for indicators in the literature and discussions on the subject in specialized congresses and multidisciplinary meetings with experts from the research group, considering the outcomes to be tested. The following initial data were recorded in the collection form: gender, age at referral, decade of referral and adherence; and the following data were collected at each urodynamic evaluation: urodynamic diagnosis, urodynamic indicators, indicated treatment, and symptoms related to neurogenic bladder. The considered symptoms were diurnal and nocturnal urinary incontinence and urinary tract infection.
A descriptive analysis of all variables studied at the time of the first evaluation was carried out, using frequency tables and numerical summary statistics. Bivariate analyses were then performed among the study variables at the time of the first evaluation and the outcome variable, using the chi-squared test. At this step, crude relative risk was calculated as a measure of the association between each study variable and the outcome.
The variables whose p-values were lower than 0.1 were selected for the multivariate analysis, which used logistic regression modeling to determine the adjusted relative risks. The selected variables were included in the modeling process using the forward method, according to the order of greatest deviance, using a significant result (p<0.05) in the likelihood ratio test as criterion to maintain the variable in the model. The significance of each coefficient estimated in the final model was determined using Wald test.
A descriptive analysis of urodynamic evolution and symptoms related to neurogenic bladder over time was performed through proportions and medians for categorical and numerical variables, respectively.
ResultsA total of 322 patients met the inclusion criteria. Ten patients were lost due to missing data: urodynamic evaluation (seven patients), initial diagnosis (one patient), and improvement throughout treatment (two patients). Additionally, 76 patients were lost, as they underwent only one urodynamic evaluation. Six patients were excluded because they had a normal bladder at the first urodynamic evaluation. The results shown below refer to the remaining 230 patients.
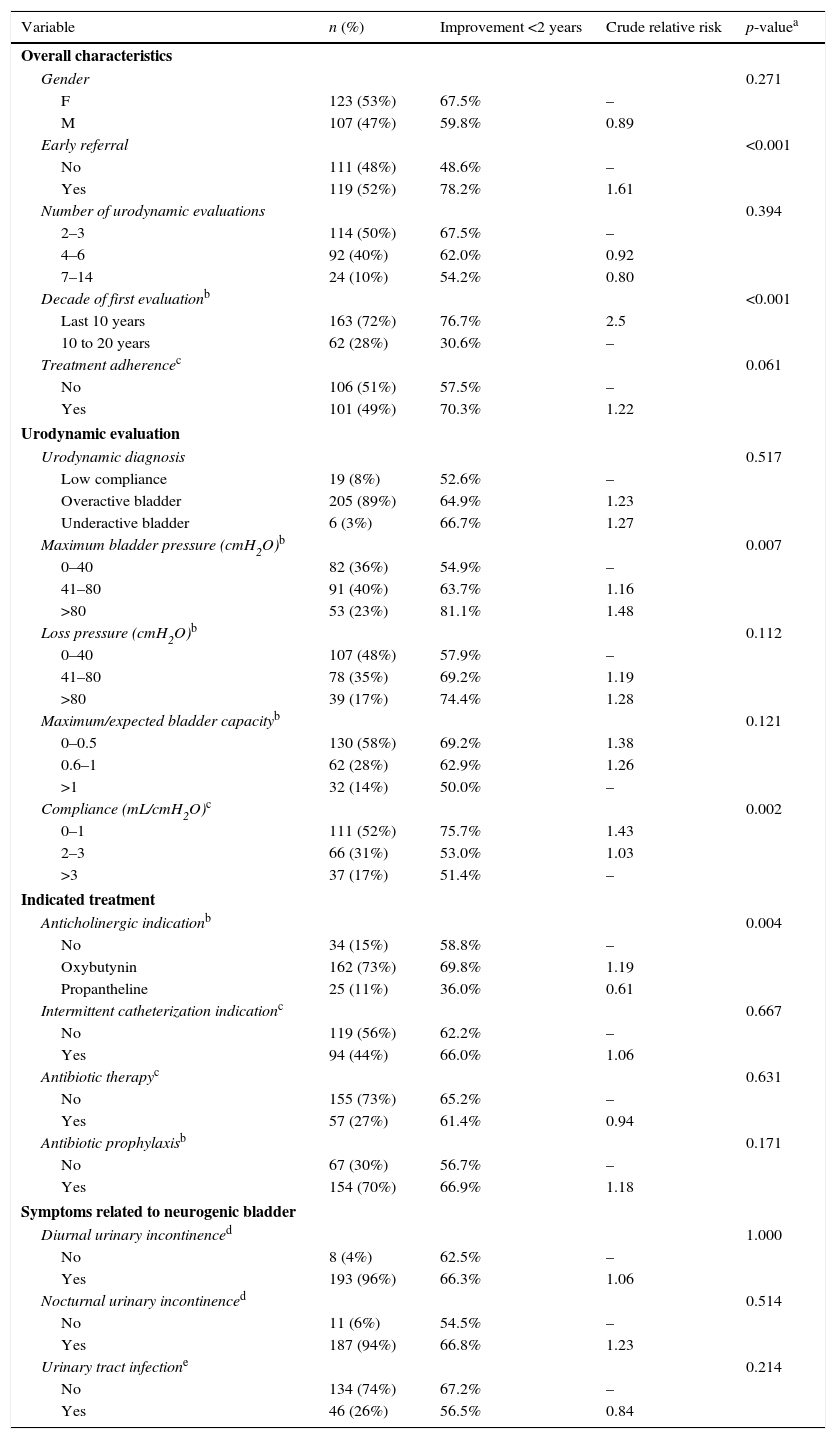
The characteristics of these patients at the time of the first urodynamic evaluation are described in Table 1. There was no significant difference regarding gender proportions.
Characteristics of the population at the first urodynamic evaluation and association with improvement in up to two years of treatment, 1990 and 2013.
| Variable | n (%) | Improvement <2 years | Crude relative risk | p-valuea |
|---|---|---|---|---|
| Overall characteristics | ||||
| Gender | 0.271 | |||
| F | 123 (53%) | 67.5% | – | |
| M | 107 (47%) | 59.8% | 0.89 | |
| Early referral | <0.001 | |||
| No | 111 (48%) | 48.6% | – | |
| Yes | 119 (52%) | 78.2% | 1.61 | |
| Number of urodynamic evaluations | 0.394 | |||
| 2–3 | 114 (50%) | 67.5% | – | |
| 4–6 | 92 (40%) | 62.0% | 0.92 | |
| 7–14 | 24 (10%) | 54.2% | 0.80 | |
| Decade of first evaluationb | <0.001 | |||
| Last 10 years | 163 (72%) | 76.7% | 2.5 | |
| 10 to 20 years | 62 (28%) | 30.6% | – | |
| Treatment adherencec | 0.061 | |||
| No | 106 (51%) | 57.5% | – | |
| Yes | 101 (49%) | 70.3% | 1.22 | |
| Urodynamic evaluation | ||||
| Urodynamic diagnosis | 0.517 | |||
| Low compliance | 19 (8%) | 52.6% | – | |
| Overactive bladder | 205 (89%) | 64.9% | 1.23 | |
| Underactive bladder | 6 (3%) | 66.7% | 1.27 | |
| Maximum bladder pressure (cmH2O)b | 0.007 | |||
| 0–40 | 82 (36%) | 54.9% | – | |
| 41–80 | 91 (40%) | 63.7% | 1.16 | |
| >80 | 53 (23%) | 81.1% | 1.48 | |
| Loss pressure (cmH2O)b | 0.112 | |||
| 0–40 | 107 (48%) | 57.9% | – | |
| 41–80 | 78 (35%) | 69.2% | 1.19 | |
| >80 | 39 (17%) | 74.4% | 1.28 | |
| Maximum/expected bladder capacityb | 0.121 | |||
| 0–0.5 | 130 (58%) | 69.2% | 1.38 | |
| 0.6–1 | 62 (28%) | 62.9% | 1.26 | |
| >1 | 32 (14%) | 50.0% | – | |
| Compliance (mL/cmH2O)c | 0.002 | |||
| 0–1 | 111 (52%) | 75.7% | 1.43 | |
| 2–3 | 66 (31%) | 53.0% | 1.03 | |
| >3 | 37 (17%) | 51.4% | – | |
| Indicated treatment | ||||
| Anticholinergic indicationb | 0.004 | |||
| No | 34 (15%) | 58.8% | – | |
| Oxybutynin | 162 (73%) | 69.8% | 1.19 | |
| Propantheline | 25 (11%) | 36.0% | 0.61 | |
| Intermittent catheterization indicationc | 0.667 | |||
| No | 119 (56%) | 62.2% | – | |
| Yes | 94 (44%) | 66.0% | 1.06 | |
| Antibiotic therapyc | 0.631 | |||
| No | 155 (73%) | 65.2% | – | |
| Yes | 57 (27%) | 61.4% | 0.94 | |
| Antibiotic prophylaxisb | 0.171 | |||
| No | 67 (30%) | 56.7% | – | |
| Yes | 154 (70%) | 66.9% | 1.18 | |
| Symptoms related to neurogenic bladder | ||||
| Diurnal urinary incontinenced | 1.000 | |||
| No | 8 (4%) | 62.5% | – | |
| Yes | 193 (96%) | 66.3% | 1.06 | |
| Nocturnal urinary incontinenced | 0.514 | |||
| No | 11 (6%) | 54.5% | – | |
| Yes | 187 (94%) | 66.8% | 1.23 | |
| Urinary tract infectione | 0.214 | |||
| No | 134 (74%) | 67.2% | – | |
| Yes | 46 (26%) | 56.5% | 0.84 | |
The patient's age at the time of the first urodynamic evaluation, considered here as the “point zero” of the analysis, ranged from 14 days to 19 years, with a mean of 2.9 years and a median of 0.85 years (10.2 months). Most patients (80%) had their urinary system evaluated for the first time in early childhood; 52% were referred early and underwent the first urodynamic evaluation within the first year of life (Table 1). However, 9% of patients were referred for the first time when they were older than 9 years of age. The number of urodynamic evaluations performed per patient within the period ranged from two to 14. Most patients (77%) were included in the study less than ten years ago.
The most common urodynamic diagnosis found at the first evaluation was overactive bladder (89%; Table 1). Most patients had bladder pressure >40cmH2O, being >80cmH2O in 23% of them. The loss pressure was >40cmH2O in approximately 50% of the patients, and in 17%, it was >80cmH2O. More than 80% of the patients had bladder compliance <3mL/cmH2O and bladder capacity below the expected for age (Table 1). Most patients had been treated with anticholinergics (mainly oxybutynin) since the first diagnosis. Intermittent catheterization was indicated in a little less than 50% of the total cases. Antibiotic therapy to control urinary tract infection was indicated in 27% of cases and maintenance of a prophylactic antibiotic therapy, in 70%.
Regarding the main symptoms related to neurogenic bladder, 96% had diurnal urinary incontinence and 94% had nocturnal incontinence, associated or not with fecal incontinence. Urinary infection was present in 26% of the cases (Table 1) and this variable was showed the largest percentage of missing data (22%).
Approximately half of the included patients adhered to the treatment, receiving regular treatment as indicated and attending all scheduled appointments and exams.
The first urodynamic improvement was observed in up to two years of treatment in 64% of the patients; 28% presented the first improvement after two years and 8% did not show improvement during the entire follow-up period.
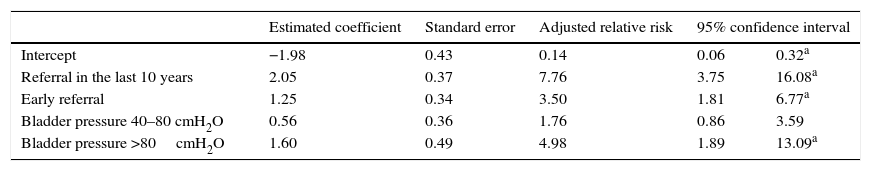
The following variables showed p-value <0.1 at the bivariate analysis and were selected for the modeling process: early referral, decade of the first evaluation, treatment adherence, bladder pressure, bladder compliance, and indication of anticholinergic drugs. After adjusting for the logistic regression model, early referral remained significantly associated with the outcome urodynamic improvement in up to two years of treatment (Table 2). The probability of urodynamic improvement in up to two years among those who were referred early for specialized treatment was 3.5 times higher than for those referred after the first year of life (95% CI: 1.81–6.77). Patients referred in the last ten years or with bladder pressure >80cmH2O at the first evaluation also had a greater probability of urodynamic improvement in two years.
Logistic regression model for urodynamic improvement in up to two years of treatment.
| Estimated coefficient | Standard error | Adjusted relative risk | 95% confidence interval | ||
|---|---|---|---|---|---|
| Intercept | −1.98 | 0.43 | 0.14 | 0.06 | 0.32a |
| Referral in the last 10 years | 2.05 | 0.37 | 7.76 | 3.75 | 16.08a |
| Early referral | 1.25 | 0.34 | 3.50 | 1.81 | 6.77a |
| Bladder pressure 40–80 cmH2O | 0.56 | 0.36 | 1.76 | 0.86 | 3.59 |
| Bladder pressure >80cmH2O | 1.60 | 0.49 | 4.98 | 1.89 | 13.09a |
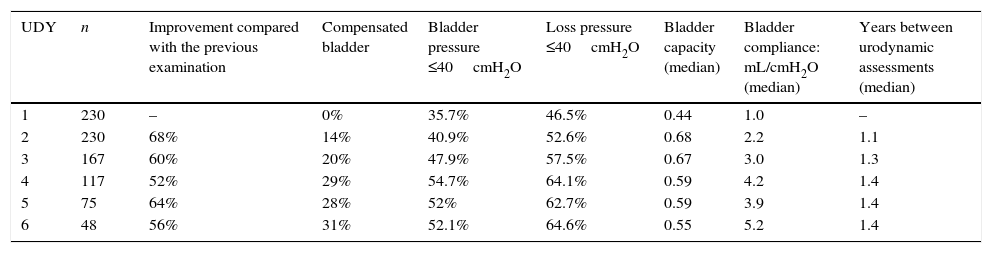
Overall, 910 evaluations were reviewed for the analysis of urodynamic evolution. However, since the number of patients with seven or more evaluations was very small, they were excluded from the statistical analysis; therefore, 867 evaluations were available, related to the first six evaluations performed. The mean time interval between urodynamic evaluations was 1.6 years, with a median of 1.3 years. Most patients repeated the examination after a period of six to 12 months (21%) and 12–18 months (34%).
Table 3 shows that the urodynamic pattern improved with treatment. The percentage of improvement in relation to the previous urodynamic evaluation was 68% at the second evaluation and ranged from 52% to 64% at subsequent evaluations. The proportion of patients with compensated bladder at the second evaluation was 14%, and this proportion increased throughout the treatment. The percentage of patients who had maximum bladder pressure and loss pressure <40cmH2O increased over time and stabilized after the fourth urodynamic evaluation. The same was observed for bladder capacity in relation to the capacity expected for age, while bladder compliance showed an upward trend throughout the analyzed period. The median time between evaluations increased until the fourth evaluation and remained constant thereafter.
Urodynamic evolution during follow-up.
| UDY | n | Improvement compared with the previous examination | Compensated bladder | Bladder pressure ≤40cmH2O | Loss pressure ≤40cmH2O | Bladder capacity (median) | Bladder compliance: mL/cmH2O (median) | Years between urodynamic assessments (median) |
|---|---|---|---|---|---|---|---|---|
| 1 | 230 | – | 0% | 35.7% | 46.5% | 0.44 | 1.0 | – |
| 2 | 230 | 68% | 14% | 40.9% | 52.6% | 0.68 | 2.2 | 1.1 |
| 3 | 167 | 60% | 20% | 47.9% | 57.5% | 0.67 | 3.0 | 1.3 |
| 4 | 117 | 52% | 29% | 54.7% | 64.1% | 0.59 | 4.2 | 1.4 |
| 5 | 75 | 64% | 28% | 52% | 62.7% | 0.59 | 3.9 | 1.4 |
| 6 | 48 | 56% | 31% | 52.1% | 64.6% | 0.55 | 5.2 | 1.4 |
UDY, urodynamic assessment.
Bladder capacity: maximum bladder capacity measured during examination/bladder capacity expected for age.
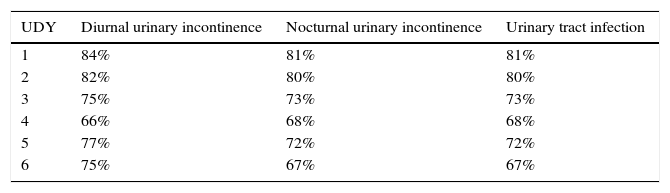
Regarding urinary symptoms, there was a reduction in the percentage of patients with diurnal and nocturnal urinary incontinence, as well as in the percentage of those with urinary tract infection that was diagnosed and treated (Table 4).
Of the five patients with normal urodynamic pattern at the first evaluation who maintained the follow-up, four developed overactive bladder at a subsequent examination and one has not been reevaluated yet.
Eleven patients progressed with some degree of renal impairment and are being followed-up by a nephrologist; none of them has dialysis indication.
DiscussionThe importance of urodynamic diagnosis in pediatric patients with neurogenic bladder has been demonstrated since the 1980s.11,12 In 2012, the International Children's Continence Society published a consensus document confirming the need to perform a urodynamic study in all children born with myelomeningocele as a diagnostic priority; the exam should be performed as soon as the closure of the neurological lesion is stabilized.13 The present study confirmed the association between early referral for specialized diagnosis and treatment and urodynamic improvement. Patients treated up to the first year of life were 3.5 times more likely to improve within two years.
Early urological intervention is essential to reduce morbidity to the upper urinary system. Altered urodynamic findings in pediatric patients with neurogenic bladder are predictive of renal deterioration in adults,14 and the time of delayed treatment is directly proportional to nephropathy severity.15
Since its creation, this service has used urodynamic evaluation as the main tool for the diagnosis and treatment of patients with neurogenic bladder and has sought evidence on the effect of early intervention on patients’ evolution.16,17 The protocol used is preventive and includes early urological evaluation from the first month of life, before the onset of urinary symptoms (urinary incontinence or infection), with urodynamic evaluation in all cases; treatment is initiated based on the urodynamic evaluation results. According to Verpoorten,18 the therapeutic objective should not be limited to treating secondary damages to the lower and upper urinary tract, but rather it should be to ensure normal renal and bladder development, with safe pressure levels and urinary continence.
The authors have tried to disseminate this practice also among the services that refer patients to this service. Nevertheless, despite all efforts, patients are still referred at a late stage. In this study, 48% of the cases underwent the first urodynamic evaluation after the first year of life, and approximately one in every 12 patients was evaluated only after the age of nine. Most patients had an overactive bladder and at-risk urodynamic evaluation, with blood pressure levels >40cmH2O and reduced bladder capacity and compliance.
During the urination process, the bladder filling stage is the longest. The capacity of the bladder to act as a low-pressure reservoir is essential for the health of the urinary system, mainly renal. The increase in bladder pressure to levels >40cmH2O during the filling stage interferes with the renal filtration and drainage system and is therefore a risk factor. The association between the reduction in glomerular filtration and elevated bladder pressure was experimentally demonstrated in 1988.19 During the emptying phase, the risk lies in the lack of synergy between bladder contraction and sphincter relaxation, with urinary retention and increase in bladder pressure to overcome the obstacle and expel the urine. The associated clinical repercussions are recurrent urinary tract infection, vesicoureteral reflux, and hydronephrosis. The corresponding urodynamic diagnoses are overactive bladder, low bladder compliance (the most commonly observed diagnosis in this study), and detrusor sphincter dyssynergia, which was not diagnosed in the present patients due to problems in the electromyography device.
It was shown that urodynamic improvement throughout the treatment was accompanied by improvement in urinary incontinence and infection. Urinary incontinence is primarily related to loss of storage capacity caused by increased intravesical pressure during filling and reduction in bladder compliance and capacity, which occur in patients with overactive bladder and low compliance. Urinary incontinence was the symptom most commonly associated with neurogenic bladder. Although not a risk factor, it results in stigma and low self-esteem, especially in adolescents with chronic urinary incontinence, with an impact on quality of life.20
A lower percentage of cases of urinary tract infection was observed in the present study when compared with the literature. The differential diagnosis between bacteriuria and urinary infection is often difficult, especially in patients who have intermittent catheterization. The percentages of antibiotic therapy indication and cases of urinary infection were compatible, suggesting this information was factual in the studied group.
Notwithstanding the recognized difficulties, retrospective studies are advantageous to understand and assess the effectiveness of the used approach and to qualify evidence-based care, provided they are methodologically well-designed.21 The variables of the present study showing the highest percentages of missing data were those related to symptoms. The urodynamic variables, which are those of interest for the object, were recovered by reviewing the results of the examinations, not from the description of the medical records. The exposure variable was obtained from the date of birth, which is generally well documented. The researcher responsible for the design and analysis of data was not involved in patient care or data collection, reducing the risk of bias.
Studies conducted in a single center usually have lower external validity. However, the fact that this is a reference center for myelomeningocele treatment, as well as a human resource training center for the Brazilian Unified Health System (Sistema Único de Saúde [SUS]) promotes the inclusion of patients and the participation of professionals from other centers.
As demonstrated, early treatment improves urodynamic prognosis in neurogenic voiding dysfunction. Treatment onset in the first year of life increases by three-fold the probability of urodynamic improvement in up to two years. The role of the neonatologist and the pediatrician in recognizing and referring patients to diagnosis is extremely important, ensuring the start of specialized treatment within the first year of life.
FundingPIP (IFF/FIOCRUZ Research Support Program) and FAPERJ (PP-SUS).
Conflicts of interestThe authors declare no conflicts of interest.
To Merlin P. Jimenez (database development) and scientific initiation fellows: Debora F.L. Diufrayer; Rafaela C. Carvalho; Renata A. Araújo; and Thamires C. Guimarães.
Please cite this article as: Monteiro LM, Cruz GO, Fontes JM, Vieira ET, Santos EN, Araújo GF, et al. Early treatment improves urodynamic prognosis in neurogenic voiding dysfunction: 20 years of experience. J Pediatr (Rio J). 2017;93:420–7.
Study carried out at Fundação Oswaldo Cruz (Fiocruz), Instituto Nacional de Saúde da Mulher, da Criança e do Adolescente Fernandes Figueira (IFF), Rio de Janeiro, RJ, Brazil.