Despite anti-smoking prevention programs, many adolescents start smoking at school age. The main objectives of this study were to determine the prevalence and risk factors associated with smoking in adolescents living in Uruguaiana, RS, Brazil.
MethodsA prospective study was conducted in adolescents (12–19 years), enrolled in municipal schools, who answered a self-administered questionnaire on smoking.
Results798 adolescents were enrolled in the study, with equal distribution between genders. The tobacco experimentation frequency (ever tried a cigarette, even one or two puffs) was 29.3%; 14.5% started smoking before 12 years of age and 13.0% reported smoking at least one cigarette/day last month. Having a smoking friend (OR: 5.67, 95% CI: 2.06–7.09), having cigarettes offered by friends (OR: 4.21, 95% CI: 2.46–5.76) and having easy access to cigarettes (OR: 3.82, 95% CI: 1.22–5.41) was identified as factors associated with smoking. Having parental guidance on smoking (OR: 0.67, 95% CI: 0.45–0.77), having no contact with cigarettes at home in the last week (OR: 0.51, 95% CI: 0.11–0.79) and knowing about the dangers of electronic cigarettes (OR: 0.88, 95% CI: 0.21–0.92) were identified as protection factors.
ConclusionThe prevalence of smoking among adolescents in Uruguaiana is high. The implementation of measures to reduce/stop tobacco use and its new forms of consumption, such as electronic cigarettes and hookah, are urgent and imperative in schools.
Apesar dos programas de prevenção antitabagista, muitos adolescentes começam a fumar na idade escolar. Foram objetivos do estudo determinar a prevalência e os fatores de risco associados ao consumo de tabaco em adolescentes moradores do município de Uruguaiana RS, Brasil.
MétodosEstudo transversal, realizado em adolescentes de 12 a 19 anos, matriculados em escolas do município, que responderam questionário autoaplicável sobre tabagismo.
ResultadosParticiparam 798 adolescentes com igual distribuição entre os gêneros. A frequência de experimentação de tabaco (Alguma vez tentou fumar um cigarro, mesmo que uma ou duas tragadas) foi 29,3%, sendo que 14,5% começaram fumar antes dos 12 anos de vida e 13,0% deles afirmaram terem fumado pelo menos um cigarro/dia no último mês. Foram identificados como associados ao tabagismo: ter amigo tabagista (OR:5,67, IC95%:2,06-7,09), ter oferta de cigarro pelo amigo (OR:4,21, IC95%:2,46-5,76) e facilidade de conseguir cigarros (OR:3,82, IC95%:1,22-5,41). Ter orientações dos pais sobre tabagismo (OR:0,67, IC95%:0,45-0,77), não ter contato com cigarro em casa na última semana (OR:0,51, IC95%:0,11-0,79) e saber os malefícios do cigarro eletrônico (OR:0,88, IC95%:0,21-0,92) foram identificados como de proteção.
ConclusõesA prevalência de tabagismo entre os adolescentes de Uruguaiana é alta. A implantação de medidas nas escolas para reduzir ou acabar o consumo de tabaco e de suas novas modalidades, como os cigarros eletrônicos e o narguilé é urgente e imperiosa.
Tobacco use is the leading preventable cause of death and diseases worldwide and it is estimated that in the 21st century, one billion people will die because of smoking.1 Approximately 80% of smokers in the world live in countries with low and/or medium income, where the burden of tobacco-related diseases has a great impact.2
A total of 11% of deaths from ischemic heart disease and 70% of deaths from lung, bronchial, and tracheal cancer are attributed to tobacco use. It is believed that the increased prevalence of smoking observed in developing countries over the years will be responsible for a two-fold increase in the overload of healthcare for non-communicable diseases.3 Therefore, it is necessary to establish an efficient and systematic surveillance mechanism to monitor the trends of use of tobacco and its derivatives.4
An international collaborative study of schoolchildren from 131 countries showed that adolescents are the group with the highest risk for smoking initiation, since the overall prevalence of schoolchildren who are active smokers was 8.9%, being higher in the Americas (17.5%) and Europe (17.9%), and less than 10% in other assessed regions.5
In Brazil, the National School-Based Health Survey (Pesquisa Nacional de Saúde do Escolar [PeNSE]) documented that 30% of young individuals aged between 13 and 15 started smoking before 12 years of age.6 It has been reported that habits acquired at this stage of life are usually kept at adulthood and are difficult to modify,7 and that although adolescents have knowledge of the risks that are involved in the consumption of tobacco and its derivatives, their habits seem to be divergent.8 It is during the transition years, during high school and college/university, that tobacco use starts, as well as greater stabilization of smoking behavior.9
For this reason, over the past decades, the school environment has been the focus of specific efforts to influence the behavior of adolescents, by using appropriate interventions to help them avoid tobacco use at such an early stage in their lives.10,11
Thus, considering the consumption of cigarettes by adolescents as a risk behavior to their health and that although a recent Brazilian study12 showed a reduction in the prevalence of smoking among young individuals, particularly those in a vulnerable socio-economic condition, smoking among adolescents it is still a major challenge in the city of Uruguaiana, state of Rio Grande do Sul, Brazil.
Therefore, the authors aimed to carry out this study among adolescents enrolled in public schools in the municipality of Uruguaiana to assess the true dimensions of the problem.
MethodsStudy designProspective study carried out between March and June 2015 in the city of Uruguaiana, RS, whose population is estimated at 125,435 inhabitants, of which 6% are at the age range of the study, i.e., 12–19 years.13
Of the 66 schools in the municipality (31 municipal, 32 state, and three private schools) 51 were excluded (31 municipal and 20 state schools) as the students enrolled in these schools were not at the age range assessed in the study. Of the 15 remaining schools, eight were randomly selected for the study. During the second phase, classes containing students at the age group assessed in the study were randomly selected in each school and the students were invited to participate.
Sample size calculationThe sample size calculation was performed using these parameters: prevalence of 10% for tobacco consumption with a confidence level of 95% and alpha error of 5%, resulting in 750 students, plus 20% for eventual losses, which resulted in a final sample of 900 students.
The study was approved by the Ethics Committee of Hospital Santa Casa de Caridade of Uruguaiana and was granted permission to carry out the research by the Department of State Education and respective private schools in Uruguaiana.
All adolescents signed the free and informed consent form, and those younger than 18 years also had the form signed by their parents/guardians.
Data collectionThe adolescents allowed to participate in the study answered the self-administered questionnaire in the classroom, and due to confidentiality issues, were identified only by age and gender. The questionnaires were filled out with the help of a trained investigator (VJO, physical education teacher) present in the classroom at that time.
The self-administered questionnaire used in the study was the California Tobacco Survey,14 translated into Portuguese and adapted to the Brazilian culture according to international recommendations.15 The questionnaire was independently translated into Portuguese by two Brazilian physicians specialized in allergies (forward translation). The two translations were compared by two other physicians and disagreements were eliminated after consensus. The product was then translated into English by a native English-speaking translator (backward translation) and compared to the original questionnaire, with no relevant differences found between them. The final version in Portuguese was administered to a group of adolescents to assess their understanding and difficulties in answering it, and a few linguistic adaptations were performed (patient testing). A few adjustments were made and the final version of the questionnaire was completed (Tables 1 and 2).
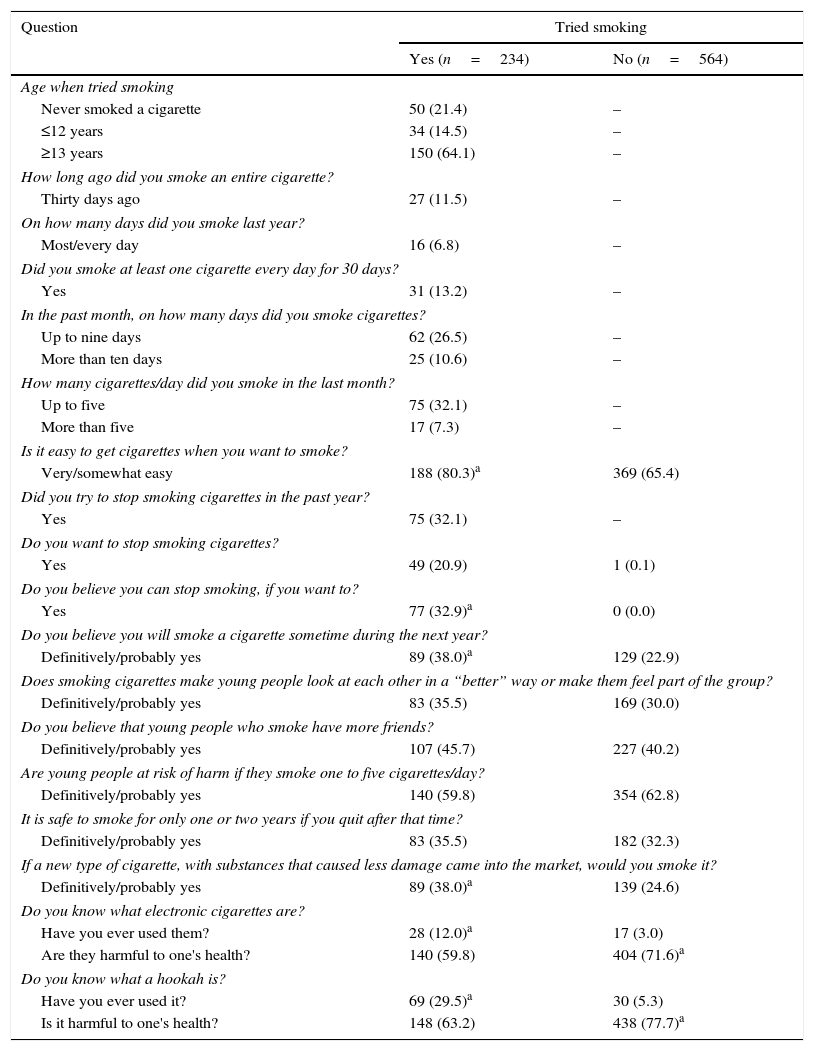
Adolescents’ answers regarding tobacco use and thoughts about it.
| Question | Tried smoking | |
|---|---|---|
| Yes (n=234) | No (n=564) | |
| Age when tried smoking | ||
| Never smoked a cigarette | 50 (21.4) | – |
| ≤12 years | 34 (14.5) | – |
| ≥13 years | 150 (64.1) | – |
| How long ago did you smoke an entire cigarette? | ||
| Thirty days ago | 27 (11.5) | – |
| On how many days did you smoke last year? | ||
| Most/every day | 16 (6.8) | – |
| Did you smoke at least one cigarette every day for 30 days? | ||
| Yes | 31 (13.2) | – |
| In the past month, on how many days did you smoke cigarettes? | ||
| Up to nine days | 62 (26.5) | – |
| More than ten days | 25 (10.6) | – |
| How many cigarettes/day did you smoke in the last month? | ||
| Up to five | 75 (32.1) | – |
| More than five | 17 (7.3) | – |
| Is it easy to get cigarettes when you want to smoke? | ||
| Very/somewhat easy | 188 (80.3)a | 369 (65.4) |
| Did you try to stop smoking cigarettes in the past year? | ||
| Yes | 75 (32.1) | – |
| Do you want to stop smoking cigarettes? | ||
| Yes | 49 (20.9) | 1 (0.1) |
| Do you believe you can stop smoking, if you want to? | ||
| Yes | 77 (32.9)a | 0 (0.0) |
| Do you believe you will smoke a cigarette sometime during the next year? | ||
| Definitively/probably yes | 89 (38.0)a | 129 (22.9) |
| Does smoking cigarettes make young people look at each other in a “better” way or make them feel part of the group? | ||
| Definitively/probably yes | 83 (35.5) | 169 (30.0) |
| Do you believe that young people who smoke have more friends? | ||
| Definitively/probably yes | 107 (45.7) | 227 (40.2) |
| Are young people at risk of harm if they smoke one to five cigarettes/day? | ||
| Definitively/probably yes | 140 (59.8) | 354 (62.8) |
| It is safe to smoke for only one or two years if you quit after that time? | ||
| Definitively/probably yes | 83 (35.5) | 182 (32.3) |
| If a new type of cigarette, with substances that caused less damage came into the market, would you smoke it? | ||
| Definitively/probably yes | 89 (38.0)a | 139 (24.6) |
| Do you know what electronic cigarettes are? | ||
| Have you ever used them? | 28 (12.0)a | 17 (3.0) |
| Are they harmful to one's health? | 140 (59.8) | 404 (71.6)a |
| Do you know what a hookah is? | ||
| Have you ever used it? | 69 (29.5)a | 30 (5.3) |
| Is it harmful to one's health? | 148 (63.2) | 438 (77.7)a |
Chi-squared/Fisher's exact test.
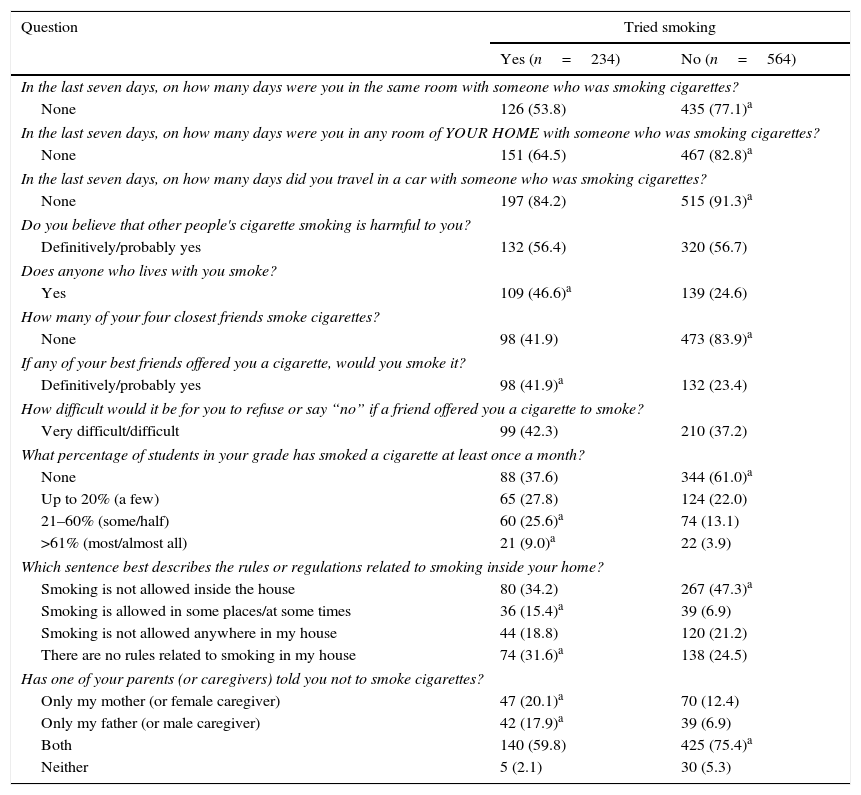
Adolescents’ answers related to exposure to other people's smoking.
| Question | Tried smoking | |
|---|---|---|
| Yes (n=234) | No (n=564) | |
| In the last seven days, on how many days were you in the same room with someone who was smoking cigarettes? | ||
| None | 126 (53.8) | 435 (77.1)a |
| In the last seven days, on how many days were you in any room of YOUR HOME with someone who was smoking cigarettes? | ||
| None | 151 (64.5) | 467 (82.8)a |
| In the last seven days, on how many days did you travel in a car with someone who was smoking cigarettes? | ||
| None | 197 (84.2) | 515 (91.3)a |
| Do you believe that other people's cigarette smoking is harmful to you? | ||
| Definitively/probably yes | 132 (56.4) | 320 (56.7) |
| Does anyone who lives with you smoke? | ||
| Yes | 109 (46.6)a | 139 (24.6) |
| How many of your four closest friends smoke cigarettes? | ||
| None | 98 (41.9) | 473 (83.9)a |
| If any of your best friends offered you a cigarette, would you smoke it? | ||
| Definitively/probably yes | 98 (41.9)a | 132 (23.4) |
| How difficult would it be for you to refuse or say “no” if a friend offered you a cigarette to smoke? | ||
| Very difficult/difficult | 99 (42.3) | 210 (37.2) |
| What percentage of students in your grade has smoked a cigarette at least once a month? | ||
| None | 88 (37.6) | 344 (61.0)a |
| Up to 20% (a few) | 65 (27.8) | 124 (22.0) |
| 21–60% (some/half) | 60 (25.6)a | 74 (13.1) |
| >61% (most/almost all) | 21 (9.0)a | 22 (3.9) |
| Which sentence best describes the rules or regulations related to smoking inside your home? | ||
| Smoking is not allowed inside the house | 80 (34.2) | 267 (47.3)a |
| Smoking is allowed in some places/at some times | 36 (15.4)a | 39 (6.9) |
| Smoking is not allowed anywhere in my house | 44 (18.8) | 120 (21.2) |
| There are no rules related to smoking in my house | 74 (31.6)a | 138 (24.5) |
| Has one of your parents (or caregivers) told you not to smoke cigarettes? | ||
| Only my mother (or female caregiver) | 47 (20.1)a | 70 (12.4) |
| Only my father (or male caregiver) | 42 (17.9)a | 39 (6.9) |
| Both | 140 (59.8) | 425 (75.4)a |
| Neither | 5 (2.1) | 30 (5.3) |
Chi-squared/Fisher's exact test.
The questionnaire consists of questions related to tobacco and smoking, as well as thoughts and knowledge on tobacco (Table 1) and exposure to smoke from others (Table 2), the smoking status of family members and friends, and knowledge of hazardous smoking habits.
The adolescents that smoked cigarettes at some point in their lives (have you ever tried smoking a cigarette, even one or two puffs?) were considered experimental smokers. Adolescents who smoked cigarettes on “one or more days in the last thirty days” were considered current smokers, as recommended by the Centers for Disease Prevention and Control (CDC) and the World Health Organization (WHO).15
Statistical analysisAfter reviewing the returned questionnaires, 102 were discarded due to questionnaire completion errors and the remaining 798 were analyzed. The obtained data were transferred to an Excel spreadsheet for further statistical analysis. Considering smoking as the dependent variable, the results were shown in relation to the exposure or not to smoke, using the chi-squared or Fisher's exact test. The variables identified as significant (p<0.05) were used in the logistic regression model (stepwise backward) and significant differences were identified.
ResultsA total of 798 questionnaires were adequately filled out, with equal distribution by gender, as they were distributed in equal numbers to both genders in each classroom.
According to the affirmative answer to the question “Have you ever tried a cigarette, even one or two puffs?” adolescents were characterized as “has tried smoking” (n=234), and the ones that answered no, as “never smoked” (n=564).
Table 1 summarizes the adolescents’ answers regarding smoking. A total of 29.3% reported having tried smoking (234/798), whereas 21.4% (50/234) reported never having smoked an entire cigarette, 14.5% started smoking before age 12, and 64.1% after 13 years old.
When asked about how long ago they had smoked an entire cigarette, 11.5% reported smoking in the last month (Table 1). Although 6.8% (16/234) of the adolescents reported having smoked on most days or every day in last month, 13.2% (31/234) had smoked at least one cigarette every day and 32.1% (75/234) had smoked at least five cigarettes in the last 30 days (Table 1). Additionally, 32.1% (75/234) reported having tried to quit smoking in the last year and 32.9% (77/234) believed they could stop smoking if they wanted to (Table 1).
The comparative analysis between the two groups significantly showed that 80.3% of those who tried smoking said they thought it was very/somewhat easy to stop smoking if they wanted to, 32.9% (77/234) believed they would be able to quit smoking if they wanted to, and 20.9% (49/234) reported they wanted to quit smoking.
Regarding thoughts on tobacco (Table 1) among those who had tried smoking, there was a significantly greater number of adolescents that believed they would be smoking in the following year. However, both groups believed that smoking cigarettes made their peers look at them in a “better” way or made them feel part of the group and that smokers had more friends, although they felt that smoking one to five cigarettes a day did not put them at risk and that smoking for one to two years would be safe, if they stopped after this period (Table 1).
When asked about a new type of cigarettes containing substances that caused less damage, 38.0% of those who tried smoking and 24.6% of those who did not smoke said they would use them (Table 1). Among the adolescents who tried smoking, there was a significantly greater account of knowledge of electronic cigarettes and hookahs when compared to those who never smoked; the use of electronic cigarettes and hookahs was also higher among those who had tried smoking (Table 1). In contrast, among those who had never smoked, there was a greater knowledge of both (electronic cigarettes and hookahs) being harmful to health (Table 1).
Regarding exposure to smoke from other people, it was observed that those who tried smoking were significantly more exposed to other people's tobacco smoke at home, in the bedroom, or in the car (Table 2). Nevertheless, there was no significant difference between the two groups regarding the thought that the smoke from others would cause damage: 56.4% for those who had tried smoking and 56.7% for those who had never smoked (Table 2).
The individuals who had tried smoking were significantly more exposed to smoke, as they lived and interacted with smokers, which would facilitate accepting the offer of a cigarette by a friend (41.9% for those who had tried smoking and 23.4% for those who had never smoked) (Table 2). Moreover, those who tried smoking reported a high percentage of school friends who smoked, or who were allowed to smoke in the house, and 47.0% of them reported there were no rules about smoking restrictions (Table 2). Among those who had never smoked, 47.3% reported smoking was not allowed inside the house. In both groups, this control is exercised by the mother and/or father (Table 2).
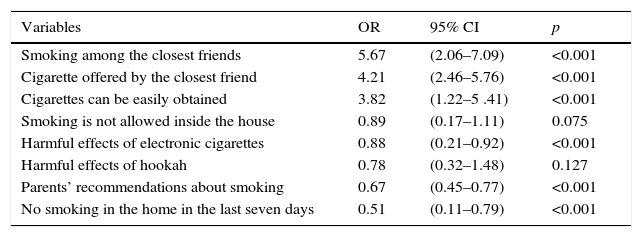
The variables identified as significantly associated with smoking after the logistic regression analysis are shown in Table 3. The following were identified as risk factors for smoking: having friends who smokes, having cigarettes offered by friends, and easy access to cigarettes (Table 3). Having parental guidance on smoking, not being exposed to smoking at home in the last week, and knowledge on the harmful effects of electronic cigarettes were identified as protective factors (Table 3). The fact that smoking was not allowed inside the home showed borderline value for significance.
Factors identified as related to smoking in adolescence after logistic regression analysis.
| Variables | OR | 95% CI | p |
|---|---|---|---|
| Smoking among the closest friends | 5.67 | (2.06–7.09) | <0.001 |
| Cigarette offered by the closest friend | 4.21 | (2.46–5.76) | <0.001 |
| Cigarettes can be easily obtained | 3.82 | (1.22–5 .41) | <0.001 |
| Smoking is not allowed inside the house | 0.89 | (0.17–1.11) | 0.075 |
| Harmful effects of electronic cigarettes | 0.88 | (0.21–0.92) | <0.001 |
| Harmful effects of hookah | 0.78 | (0.32–1.48) | 0.127 |
| Parents’ recommendations about smoking | 0.67 | (0.45–0.77) | <0.001 |
| No smoking in the home in the last seven days | 0.51 | (0.11–0.79) | <0.001 |
OR, odds ratio; 95% CI, 95% confidence interval.
Adolescence is an important stage in life, when because of the discoveries, the concerns, the need to explore the unknown and venture without worrying about the consequences, adolescents often adopt risky behaviors, including cigarette smoking.8 However, although not all adolescents who try cigarettes become smokers, experimentation is the first step toward future adherence to regular consumption of tobacco products.7
The definition of a smoker used in the present study was the one recommended by the WHO15 and the prevalence of smoking among the evaluated adolescents was 37.2%, with 13.2% of them smoking every day, higher than the rate previously observed in other locations.5 These rates were lower than those among the general population in several locations in Brazil (22.3–29.3%).16 However, they were much higher than those observed in Porto Alegre: 7.4% for men and 9.1% in women.11
It is noteworthy that among the adolescents evaluated here, 14.5% started cigarette smoking before 12 years of age and 64.1% did so after the age of 13, similarly to what was previously observed among students of the public school system in ten Brazilian city capitals, showing that 11.6% of students had tried smoking between 10 and 12 years of age,17 as well as Study of Cardiovascular Risks in Adolescents (ERICA)11 where 30% of young individuals had tried smoking before 12 years and earlier than the age observed by other authors.18
Early initiation of tobacco use is an important prognostic factor for disease and should be avoided. The delay of a few years in the start of consumption can reduce by almost two-fold the risk of damage caused by tobacco to health.6 On the other hand, it is shown that with increasing age, adolescents who try tobacco and do not interrupt the habit become tobacco users, thus consolidating the habit of smoking.7
The main factors associated with cigarette smoking by adolescents evaluated here were: having friends who smoke and having cigarettes offered by friends, in addition to easy access to cigarettes (Table 3). Although in Brazil there are laws that hinder cigarette access and consumption by children and adolescents, such as the Child and Adolescent Statute that prohibits the sale, supply, or delivery of cigarettes to children or adolescents,19 the present data confirmed that this practice has not been respected and it has been identified as a risk factor for smoking, as 80.3% of adolescent smokers reported easy access to cigarettes when they wanted to smoke (Table 1).
However, one cannot blame exclusively the legal product trade, as one should consider the clandestine sales of cigarettes, such as those that are the result of smuggling and even obtaining them from friends and/or relatives who smoke. Moreover, the role of social networks in influencing and strengthening smoking habits is clear, which has been increasingly studied and has shown that having friends who smoke increases the tolerance to these habits, as well as the possibility of adopting them,20 identified as the main risk factor for smoking among adolescents assessed here (Table 3). These data are corroborated by a North-American study, which observed that non-smoking adolescents with friends who smoked were more likely to start smoking in the future than those whose friends did not smoke.21
It is noteworthy that, although parental smoking was more frequent among adolescent smokers (Table 2), it was not identified as a risk factor for current smoking. This is in contrast with the observations of other studies that show the critical influence of parents on adolescent smoking behavior. It is known that children are more likely to reproduce the behaviors and attitudes of their parents, who are considered by them as role models; additionally, parents who smoke are more likely to allow smoking inside the house.22
On the other hand, having parental guidance on smoking, not being exposed to smoking at home in the last week, and knowing the harmful effects of electronic cigarettes were identified as protective factors (Table 3). In a way, all these factors are derived from education about the harmful effects of smoking.
Although there has been a reduction in smoking rates among parents, the same has not occurred among adolescents.23 This suggests that tobacco control interventions should be more comprehensive and targeted to other influences, such as friends,20 school,9 visual media,24 or toward the acquisition of new habits, such as the use of hookahs25 or electronic cigarettes,26 with the latter being an important initiating agent of smoking, as well as increased tax rates.2
Thus, comparing the results observed in the ERICA11 and PeNSE-201227 studies, the prevalence of experimentation was 18.5% vs. 19.6%, respectively, lower than the present result of 29.3%, and for current smoking, 5.7% vs. 5.1%, against 13% among the present study's adolescents. Nevertheless, one cannot rule out the possibility of underreporting by the adolescents themselves, identified as common practice in studies on smoking. The low rates observed in these national studies11,27 possibly reflect the country's pioneering comprehensive policies, which have a major impact on reducing tobacco use among young individuals, such as the legislation that banned smoking in indoor public environments, the ban on advertising in all media except at sales points, and the prohibition of misleading descriptors, such as “light” or “ultra-light” on cigarette packs.28
In the city of Uruguaiana (South Brazil), the results were different. The finding of higher prevalence rates in the South could be possibly due to the region cultivation and production of tobacco, as well as a greater influence of European migration that traditionally entails a high prevalence of smoking habits, which can be perpetuated through generations.11 To all these facts, one must be add the easy access to cigarettes, such as in the case of smuggling, as recently identified in the city of Uruguaiana.29
It is important that anti-smoking educational programs be encouraged in schools, so that students receive guidance and professional help, especially for those who want to quit smoking.9,30 The demand for specialized health services outside the school environment can result in increased school absenteeism and even hinder the adolescents’ access and adherence to the programs.
These results reinforce the need to strengthen, at the municipal or state level, public policies aimed at reducing or eliminating contact of children and/or adolescents with cigarettes. Compliance with the laws restricting the sale and consumption of cigarettes, increasing the legal age of purchase, promoting healthy lifestyles, family involvement in the prevention of smoking habit programs, price increases, implementation of anti-smoking programs in schools, as well as appropriate guaranteed treatments for smokers, are some of the measures that could be undertaken.
Pediatricians, being the first professionals to care for the children, know their environmental exposure, follow their development, and have a primary role as educators and promoters of healthy habits.
Although the consequences of smoking are observed in adulthood, it should be noted that the reduction or restriction of tobacco consumption in adolescence will have an educational impact on health and can reduce the possibility of contact with other restrictions or illicit drugs, so it is essential for the physician to be attentive and well informed, and to participate in the development of new approaches to fight against smoking, in an integrated and interdisciplinary manner.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Urrutia-Pereira M, Oliano VJ, Aranda CS, Mallol J, Solé D. Prevalence and factors associated with smoking among adolescents. J Pediatr (Rio J). 2017;93:230–7.
Study carried out at Escola Paulista de Medicina (EPM), Universidade Federal de São Paulo (UNIFESP), São Paulo, SP, Brazil.