Children with Down syndrome have delayed psychomotor development, which is a factor that influences the level of difficulty in toilet training. The current study aims to estimate the age toilet training starts and completes in children with DS compared to children with normal psychomotor development and to evaluate the method and type of toilet training most frequently used, as well as its association with lower urinary tract symptoms and functional constipation.
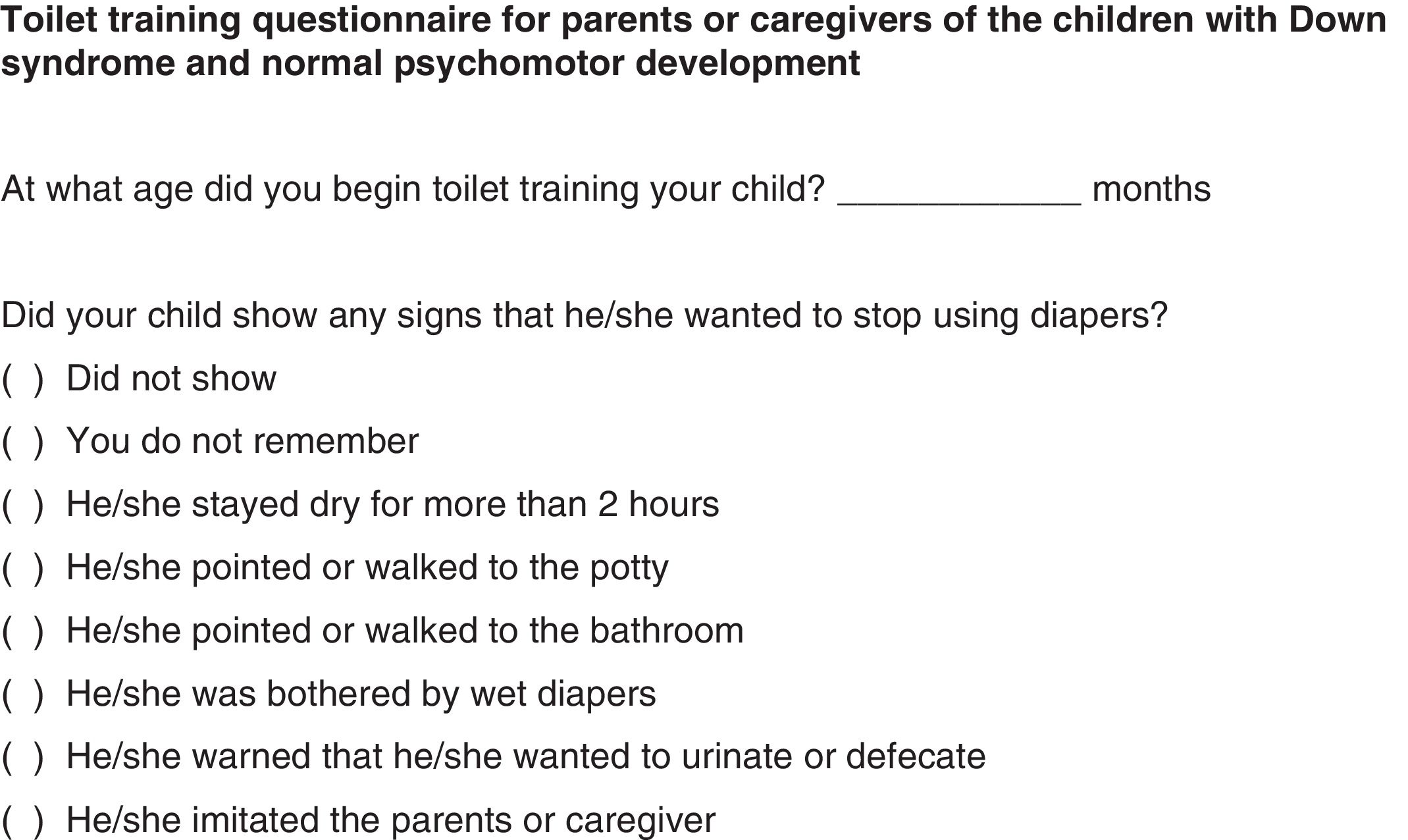
MethodsA case–control study was carried out from 2010 to 2015. All parents completed a questionnaire designed to assess the toilet training process. Lower urinary tract symptoms were assessed through the application of the Dysfunctional Voiding Symptom Score. The presence of functional constipation was assessed according to the Rome III criteria.
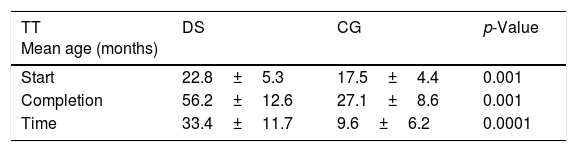
ResultsThe study included 93 children with Down syndrome and 204 children with normal psychomotor development (control group [CG]). The mean age of toilet training onset was 22.8 months in those with DS and 17.5 months in the CG (p=0.001). In children with DS, the mean age when completing toilet training was 56.2 months and 27.1 months in the CG (p=0.001). Among children with DS, females completed toilet training earlier (p=0.02). The toilet training method used most often was child-oriented approach in both groups. No association was observed with the presence of lower urinary tract symptoms or functional constipation and the age of beginning and completing toilet training in both groups.
ConclusionChildren with Down syndrome experienced prolonged toilet training time. Prospective longitudinal studies are essential to gain insight into the toilet training of these children.
Crianças com síndrome de Down apresentam desenvolvimento psicomotor atrasado, fator que influencia o nível de dificuldade do treinamento esfincteriano. O presente estudo tem como objetivo estimar a idade em que o treinamento esfincteriano é iniciado e concluído em crianças com SD em comparação a crianças com desenvolvimento psicomotor normal, avaliar o método e o tipo de treinamento esfincteriano utilizado com maior frequência, bem como sua associação com sintomas do trato urinário inferior e constipação funcional.
MétodosUm estudo caso-controle foi realizado de 2010 a 2015. Todos os pais preencheram um questionário destinado a avaliar o processo de treinamento esfincteriano. O sintomas do trato urinário inferior foram avaliados por meio da aplicação do Dysfunctional Voiding Symptom Score. A presença de constipação funcional foi avaliada de acordo com os critérios Roma III.
ResultadosO estudo incluiu 93 crianças com síndrome de Down e 204 crianças com desenvolvimento psicomotor normal (Grupo de Controle (GC)). A idade média em que as crianças iniciaram o treinamento esfincteriano foi de 22,8 meses naquelas com SD e 17,5 meses no GC (p=0,001). Em crianças com SD, a idade média ao concluir o treinamento esfincteriano foi de 56,2 meses e 27,1 meses no GC (p=0,001). Entre as crianças com SD, as do sexo feminino concluíram o treinamento esfincteriano mais cedo (p=0,02). O método de treinamento esfincteriano mais utilizado foi a abordagem voltada para a criança em ambos os grupos. Não houve associação com a presença de sintomas do trato urinário inferior ou constipação funcional e a idade no início e na conclusão do treinamento esfincteriano em ambos os grupos.
ConclusãoCrianças com síndrome de Down apresentaram tempo de treinamento esfincteriano prolongado. Estudos longitudinais prospectivos são essenciais para obter uma visão do treinamento esfincteriano dessas crianças.
Down syndrome (DS) is the most common chromosomal malformation,1 with a median life expectancy of approximately 58 years.2 DS births account for about 1–3 per 1000 live births.3 Approximately 64% of individuals with DS have at least one major associated congenital anomaly.1 Several studies show a high prevalence of abnormal findings in the lower urinary system, which can lead to progressive kidney or urinary disorders.1,4,5 Children with DS have delayed psychomotor development and problems with learning,6 being the most common genetic cause of intellectual disability.2
Toilet training for a child with any disability, including DS, is one the most challenging developmental milestones, as it is for any child.7,8 Toilet training methods have fluctuated over the last 100 years.9 Child-oriented approach is recommended by the American Academy of Pediatrics (AAP) for children with normal psychomotor development, which suggests beginning the toilet training process only when the children shows readiness signs.9–11 Therefore, this model of toilet training comprises three variant forces in child development: physiological maturation, external feedback, and internal feedback.10,11 An alternative approach, is the intensive, structured, and parent-oriented method for toilet training in one day based on the principles of conditioning and imitation developed by Azrin and Foxx.9,12 Other methods that have emerged include the assisted infant toilet training, elimination communication, and the daytime wetting alarm.9
A longitudinal survey by Schum et al. showed that the age at start of toilet training was 23 months in girls with normal psychomotor development and 25 months in boys.13 Continence acquisition was concluded at age 34.1 months in girls and 35.8 months in boys.13 A recent study in Turkey demonstrated that the beginning of toilet training occurred with 15.7 months and the conclusion with 22.3 months.14 In Brazil, the mean age at which children begin and complete toilet training was 22 months and 27.4 months respectively.15 In developing countries, toilet training appears to occur at a lower age than that in developed countries.14 Regarding children with DS, the mean age of initial interest in toilet training was between 36 and 45.7 months,8,16 and the mean age at completion of toilet training was reported to be between 48 and 66 months.8,16–18 A Brazilian study with children with intellectual disabilities of various etiologies, including 15 with DS, showed that 99% were toilet trained until 60 months age.19
The current study aimed to estimate the age toilet training starts and completes in children with DS compared to children with normal psychomotor development, evaluate the method and type of toilet training most frequently used, and the readiness signs identified, as well as the association between toilet training and lower urinary tract symptoms (LUTS) and functional constipation.
Patients and methodsThe study group comprised 127 children with DS, aged 3–14 years, who regularly attended a specialized clinic for DS from February 2010 through February 2015. A group comprised of 225 children with normal psychomotor development, already toilet trained, matched for gender, age, and socioeconomic status, who attended a pediatric and adolescent clinic comprised the control group (CG).
Children with a current urogenital disorder, untreated hypothyroidism, current use of medications or who had diseases known to interfere with bladder or sphincter function, those who still wore diapers until the end of the study, and those aged less than 3 years were not included.
A questionnaire based on the study by Stadtler et al. and Mota et al. was developed and applied to the parents to assess the history of toilet training, including age at which a child started and completed toilet training, readiness signs presented, use of potty chair or toilet, and toilet training methods,10,15 (Appendix A) urinary abnormalities, presence of chronic diseases, use of medications, and socioeconomic status. Age at which toilet training was completed was defined as the age at which a child maintained full bladder and bowel control, without any failure in holding urine or stool during the day and night.14 Children with DS who used diapers in the first evaluation were re-evaluated after completing toilet training, when the parents answered the questionnaire. This questionnaire aimed to collect the child's history and has not been externally validated. The prevalence of LUTS was estimated using the Dysfunctional Voiding Symptom Score (DVSS),20 adapted and validated for this population.21 The cutoff values to indicate the presence of LUTS were greater than 6 for females and greater than 9 for males. The presence of functional constipation was assessed according to the Rome III criteria.22 Children were only evaluated when toilet training was completed. A complete physical exam and standard assessment was performed on all subjects (including evaluation of the lumbosacral region, searching for occult spinal dysraphism). Parents were asked about history of urinary tract infection, and a urine culture was collected.
Data were expressed as means±SD, medians, and interquartile ranges, or as absolute values and fractions. Student's t-test was used to compare continuous variables, while categorical variables were compared using Fisher's exact test. Standardized mean difference (SMD) and the respective confidence intervals were additionally expressed as a measure of the effects sizes. All tests were two-sided; p<0.05 and 95% confidence interval (CI) were considered statistically significant and were performed using GraphPad Prism® (Prism, version 7.00 for Windows, GraphPad Software, CA, USA).
The current study (amendment protocol number 1960.019.2010) was approved by the University Ethics Committee, and all parents or those responsible for the patients in both groups signed an informed consent form.
ResultsOf the 127 children with DS, 93 were included in the study. Of these, 30 children who used diapers in the first evaluation were re-assessed after completing toilet training, when the parents answered the questionnaire. Of the 34 not included, three refused to participate, 14 were younger than three years of age, one girl was diagnosed with West syndrome, two boys had a posterior urethral valve, one girl had a decompensated ventricular septal defect, and five children were diagnosed with untreated hypothyroidism. Eight children had not completed toilet training by the end of the study (three girls with a mean age of 3.9±2 years and five boys with a mean age of 4.3±2.3 years); of these, all had untreated functional constipation. The CG consisted of 204 children with normal psychomotor development.
The mean age of patients when the questionnaire was answered was 7.7±2.0 years in children with DS and 7.3±3.1 years in the CG (p=0.24). Females represented 47.3% (44/93) of the children with DS and 49.5% (101/204) of the CG (p=0.80). No statistical difference was observed regarding socioeconomic status between the groups (p=0.36).
Children with DS initiated their toilet training at age of 22.8±5.3 months and in CG, at 17.5±4.4 months (SMD=5.52, 95% CI 4.26–6.78, p=0.0001). The time required to complete toilet training was 33.4±11.7 months in children with DS and 9.6±6.2 months in the CG (SMD=24.04, 95% CI 21.94–26.14, p=0.0001). The mean age at which toilet training was completed was 56.2±12.6 months in the children with DS and 27.1±8.6 months in the CG (SMD=29.12, 95% CI 27.08–31.47, p=0.0001; Table 1).
In children with DS, the mean age to complete toilet training in girls was 53.1±12.7 months, and in boys, 58.9±12.1 months (SMD=−5.89, 95% CI −10.99 to −0.80, p=0.02). In the CG, no statistical difference was observed regarding gender: the mean age for girls to complete toilet training was 27.8±8.9 months and in boys, 27.1±6.9 months (p=0.54).
Regarding readiness signs, 90% of the parents of children with DS responded that ability to walk and discomfort with wet diapers was observed, 1% reported that the child pointed or walked to the bathroom or potty chair, 1% reported that the child indicated the need to void, and 8% showed no readiness signs. 80% of the parents in the CG did not remember the readiness signs; therefore, comparison between the groups was not possible.
The child-oriented approach was the method of choice for toilet training in 87.1% (81/93) of children with DS and in 81.9% (167/204) of those of the CG (p=0.31). All other families used non-specified methods for toilet training.
When assessing the type of equipment used during toilet training, 88.2% (82/93) of the children with DS and 71.6% (146/204) of the CG used a potty chair (p=0.30), and 11.8% (11/93) of the children with DS and 28.5% (58/204) of the CG used the toilet with seat reducer (p=0.10).
LUTS was observed in 19.4% (18/93) of the children with DS and in 14.7% (30/204) of those in CG (p=0.31). The presence of the LUTS was not associated with the average age of start and completion of toilet training in either group (p>0.05).
Functional constipation was observed in 32.3% (30/93) of the children with DS and in 34.8% (71/204) of those in CG (p=0.69). It was found that 30% (9/30) of children with DS and 32.4% (23/71) of those in CG with functional constipation were already receiving treatment with polyethylene glycol (p=0.84). The presence of functional constipation was not associated with the mean age of start and completion of toilet training in both groups (p>0.05).
Only a small number of parents of the children with DS (16% [15/93]) and of the children in the CG (14.2% [29/204]) sought medical advice on toilet training (p=0.51).
DiscussionFew studies address the process of toilet training in children with disabilities,9,23 including those with DS.8,16–18 It is essential to assess the best time to start toilet training process by observing the child's developmental readiness.10 Contemporary literature has demonstrated that readiness signs in children with normal psychomotor development are well developed between 24 and 36 months of age13,24 and, in those with DS, after 36 months of age.8 Readiness signs include mainly motor skills, appropriate language, desire to please based on a positive relationship with the parent, ability to imitate the parents, and specific skills about toilet training (staying dry for more than two hours, discomfort with wet/dirty diapers, and indicating the need to void).8,10,11,13 In the present study, 90% of the parents of children with DS reported that they considered the ability to walk and the discomfort by wet diapers sufficient to begin toilet training in these children, which may have contributed to an early toilet training initiation in these children (22.8 months old). The early start in toilet training in this population was confirmed when comparing the present results to the current guidelines from the National Down Syndrome Society (NDSS),8 which recommend waiting for the third birthday for initiate toilet training. Powers et al. also demonstrated a later age (45.6 months) of initial interest in toilet training in their patients.16
The inclusion of a CG allowed the authors to demonstrate a 29-month delay for completing toilet training in children with DS (56 vs. 27 months). In a recent study with a similar design, Powers et al. identified a delay of 39 months and an age of 66 months for toilet training completion.16 Although the mean age at toilet training completion in that study was 10 months higher, a shorter period of toilet training (20.4 months) was observed in their study compared to the present DS children (34 months). This difference can be explained by the fact that DS children included in this study initiated toilet training at an earlier age (22.8 months) than those in the study by Powers et al.16 (45.6 months). It is, therefore, important to emphasize that an early initiation of toilet training in children with DS appears to have the disadvantage of a longer period of training, but the advantage of a younger age of continence acquisition.
The best time to initiate toilet training in children with DS is not yet known. In Brazilian children with normal psychomotor development, it was demonstrated that those who began to be trained earlier (before 24 months) had a longer training period, when compared with those whose training started later, no differences were observed regarding the mean age of continence acquisition.15 It is worth noting that the delay in continence acquisition is one of the factors that can postpone elementary school entry for children with DS.25 This is relevant, since the improvement in social skills outcomes for the children who start school at the usual age has been demonstrated, being paramount for the inclusion of these children.26
Girls with DS appear to have an earlier mean developmental age when compared with boys with DS of the same age.27 This finding is consistent with the present results, in which toilet training was completed sooner in females with DS than in their male peers. However, these findings are in disagreement with the results reported by Powers et al.,16 who did not find a significant difference between genders in their group of children with DS. Regarding the CG, no difference between genders was found in this study. Nonetheless, other studies in children with normal psychomotor development showed that girls acquired nearly all the skills to complete toilet training more quickly than boys by approximately 2–3 months.13,15
There are no specific guidelines for toilet training in children with DS.8 In the present study, 87.1% and 88.2% of parents of children with DS used a child-oriented approach and a potty chair for toilet training, respectively, similar to those in the CG. In the present study, parents reported the use of the child-oriented approach, identifying just a few readiness signs, which may have determined an early start of the toilet training process. No family reported the use of the intensive and structured approach (“toilet training in a day” method). Furthermore, no association was observed between the age of toilet training and use of potty chair, as found by Tarhan et al. who described that children who used this type of equipment completed their toilet training at a younger age.14
The occurrence of LUTS in children with DS was similar to that observed in children in the CG. When comparing the present data with a recent study in children with DS (27.7%),16 no statistically significant difference in the prevalence LUTS was observed. In both groups participating in the present study, no association was observed between the age the children started or completed toilet training and the presence of LUTS. In a study of children with normal psychomotor development, no relationship between completing toilet training before 24 months of age and voiding dysfunction was found.28 In another recent study, voiding dysfunction was associated with toilet training starting either before 24 months or after 36 months of age. However, voiding dysfunction was observed only in the presence of functional constipation.29 No studies that demonstrate an association between the age of starting or completing toilet training and LUTS in children with DS were retrieved.
No difference was found in the prevalence of functional constipation among the groups in the present study. Some studies showed that constipation could make defecation painful, and this may be one of the reasons a child may resist toilet training.23 Functional constipation was not associated with the age of toilet training initiation and the time the child takes to complete it. It is important to report that none of the children with DS included in the study were diagnosed with Hirschsprung's disease.
It is also worth noting that, in the present study, only 16% and 14.2% of parents of children with DS and in the CG, respectively, sought medical advice on toilet training. No statistical differences were observed, even though children with DS showed delayed development. These findings are compatible with another study, in which 15% of parents sought medical instructions.15
This present study has several limitations. The present results may not be generalizable to the population at large, as this was a convenience sample. The information provided relied on the memory of the parents or caregivers. Cases tend to attempt to identify what might have caused their disease; healthy controls have no such motivation. Thus, better recall among cases is common.30 This may explain the fact that parents of children with disabilities tend to have better recollection of the important facts that happened to their children than those of children with normal psychomotor development.
The readiness signs for toilet training in DS children still need to be clearly described. The findings presented here are important to demonstrate to parents or caregivers, as well as to the professionals involved in monitoring children with DS, the importance to determine what these signs are in order to begin the toilet training process.
It may be important to carry out intervention studies in which parents receive professional guidance, which would also allow comparing the child-oriented approach with a more structured approach. At this moment, it is known that most of the parents use to centered approach, but it is still not known which method for toilet training in children with DS is most effective.
In conclusion, children with DS start their toilet training process later than those with normal psychomotor development, take a longer time for completing it, doing so at an older age than those without any disabilities. Boys with DS finish their toilet training at an older age than girls with this syndrome. The mostly used toilet training method is the child-oriented approach. LUTS and constipation were not associated with toilet training neither in DS children nor in those with normal psychomotor development.
Conflicts of interestThe authors declare no conflicts of interest.
The authors would like to thank all the participants for their dedication and perseverance, and to thank the Ambulatory Interdisciplinary Team of Down Syndrome of the Department of Health of Children and Adolescents (Brazilian Unified Health System).
Please cite this article as: Mrad FC, Figueiredo AA, Bessa J, Netto JM. Prolonged toilet training in children with Down syndrome: a case–control study. J Pediatr (Rio J). 2018;94:286–92.