To present the characteristics of pediatric patients with chronic and irreversible diseases submitted to palliative extubation.
MethodThis is a descriptive analysis of a series of patients admitted to a public pediatric hospital, with chronic and irreversible diseases, permanently dependent on ventilatory support, who underwent palliative extubation between April 2014 and May 2019. The following information was collected from the medical records: demographic data, diagnosis, duration and type of mechanical ventilation; date, time, and place of palliative extubation; medications used; symptoms observed; and hospital outcome.
ResultsA total of 19 patients with a mean age of 2.2 years were submitted to palliative extubation. 68.4% of extubations were performed in the ICU; 11 patients (57.9%) died in the hospital. The time between mechanical ventilation withdrawal and in-hospital death ranged from 15minutes to five days. Thirteen patients used an orotracheal tube and the others used tracheostomy. The main symptoms were dyspnea and pain, and the main drugs used to control symptoms were opioids and benzodiazepines.
ConclusionsIt was not possible to identify predictors of in-hospital death after ventilatory support withdrawal. Palliative extubation requires specialized care, with the presence and availability of a multidisciplinary team with adequate training in symptom control and palliative care.
Apresentar as características de pacientes pediátricos portadores de doenças crônicas e irreversíveis submetidos a extubação paliativa.
MétodoTrata-se de análise descritiva de uma série de casos de pacientes internados em hospital público pediátrico, portadores de doenças crônicas e irreversíveis, dependentes de forma permanente de suporte ventilatório e que foram submetidos a extubação paliativa entre abril de 2014 e maio de 2019. Foram coletadas as seguintes informações do prontuário: dados demográficos, diagnóstico, duração e tipo de ventilação mecânica; data, hora e local de realização da extubação paliativa, medicamentos utilizados, sintomas observados e desfecho hospitalar.
Resultados19 pacientes com idade média de 2,2 anos foram submetidos a extubação paliativa. 68,4% das extubações foram realizadas dentro da UTI, 11 pacientes (57,9%) evoluíram para óbito no hospital. O tempo entre a retirada de ventilação mecânica e o óbito hospitalar variou entre 15 minutos e 5 dias. 13 pacientes usavam tubo orotraqueal e os demais, traqueostomia. Os principais sintomas foram dispneia e dor e as principais drogas utilizadas para o controle dos sintomas foram os analgésicos opioides e benzodiazepínicos.
ConclusõesNão foi possível identificar fatores preditores de óbito no hospital após a retirada do suporte ventilatório. A extubação paliativa demanda cuidado especializado com presença e disponibilidade de equipe multiprofissional com formação adequada em controle de sintomas e cuidados paliativos.
Technological progress in advanced life support has, over the last decades, brought an undeniable benefit regarding treatment optimization and clinical recovery of pediatric patients with diseases that cause severe impairment of vital functions.1–3 However, all this technological apparatus has been routinely used in patients with chronic and irreversible diseases, who become dependent on artificial support to permanently maintain vital functions, with a negative impact on the quality of life of patients, their families, and the care team. Such a scenario has raised ethical and moral conflicts regarding the meaning of life and survival, and while life support actions are favorable in most circumstances, withdrawal of this support is ethically appropriate when the suffering associated with treatment outweighs the benefits for the child.4
The artificial prolongation of biological life without concomitant prolongation of biographical life is considered futile and responsible for causing unnecessary additional suffering, in fact meaning the prolongation of the death process.1
The practice of medicine often does not recognize that death is a natural part of life and imposes treatments potentially associated with intense suffering to patients with life-threatening conditions, including those in the final stage of severe and irreversible diseases, regardless of the values and preferences of patients and family members. Palliative extubation is the interruption of mechanical ventilation in patients with irreversible diseases when the goal of treatment, defined together with the family, is to provide care and comfort and allow the disease to follow its natural course untildeath.1 This is the practice of orthothanasia, which aims to allow natural disease evolution, not accelerating but also not postponing death. It must be differentiated from euthanasia, defined as the practice or omission of an action whose purpose is to cause the death of someone submitted to intense suffering, motivated by feelings of compassion.
Palliative extubation is a complex procedure that requires the presence of professionals with experience in palliative care. It involves communication skills, adequate planning, multiprofessional team participation, and advanced knowledge of symptom control.
The main objective of this study is to present the characteristics of pediatric patients with chronic and irreversible diseases submitted to palliative extubation. The secondary objective is to analyze factors associated with patients' survival after withdrawal of ventilatory support.
Materials and methodsThis is a descriptive analysis of a series of patients admitted to a public pediatric hospital with chronic and irreversible diseases, permanently dependent on ventilatory support, and submitted to palliative extubation between April 2014 and May 2019. The data were retrospectively collected from patient records to complete a data collection form with the following information: demographic characteristics (age, gender); main and secondary diagnosis; duration of mechanical ventilation; type of ventilation interface (orotracheal tube or tracheostomy cannula); time between decision making and palliative extubation; date, time, and place of procedure (ICU or ward); medications used to prepare for the procedure; ventilatory parameters before withdrawal of support; symptoms observed after withdrawal of ventilatory support; treatment implemented to control symptoms, and hospital outcome (discharge or death). The variables are presented as median and interquartile range. The chi-squared test was used to analyze factors related to in-hospital death.
This study was approved by the institution's Research Ethics Committee (protocol No. 08211419.6.0000.5119).
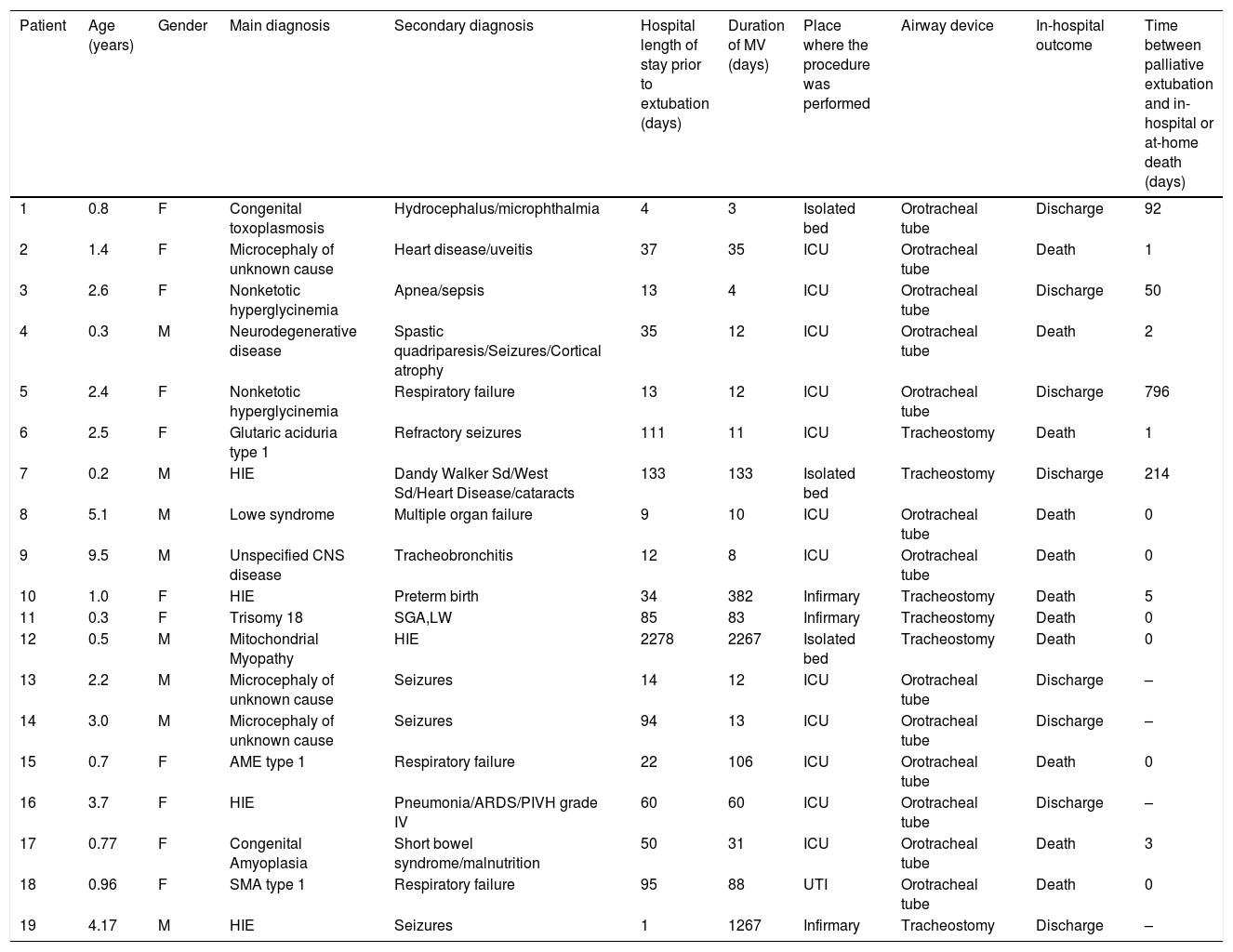
ResultsBetween April 2014 and May 2019, after the multidisciplinary team’s consensus and creation of the care plan jointly with the family, 19 patients aged 5 months to 9 years were submitted to palliative extubation at the hospital. All patients had neurological diseases, or severe and irreversible neuromuscular diseases (Table 1).
Characteristics of patients submitted to palliative extubation in HIJPII between 2014 and 2019.
| Patient | Age (years) | Gender | Main diagnosis | Secondary diagnosis | Hospital length of stay prior to extubation (days) | Duration of MV (days) | Place where the procedure was performed | Airway device | In-hospital outcome | Time between palliative extubation and in-hospital or at-home death (days) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 0.8 | F | Congenital toxoplasmosis | Hydrocephalus/microphthalmia | 4 | 3 | Isolated bed | Orotracheal tube | Discharge | 92 |
| 2 | 1.4 | F | Microcephaly of unknown cause | Heart disease/uveitis | 37 | 35 | ICU | Orotracheal tube | Death | 1 |
| 3 | 2.6 | F | Nonketotic hyperglycinemia | Apnea/sepsis | 13 | 4 | ICU | Orotracheal tube | Discharge | 50 |
| 4 | 0.3 | M | Neurodegenerative disease | Spastic quadriparesis/Seizures/Cortical atrophy | 35 | 12 | ICU | Orotracheal tube | Death | 2 |
| 5 | 2.4 | F | Nonketotic hyperglycinemia | Respiratory failure | 13 | 12 | ICU | Orotracheal tube | Discharge | 796 |
| 6 | 2.5 | F | Glutaric aciduria type 1 | Refractory seizures | 111 | 11 | ICU | Tracheostomy | Death | 1 |
| 7 | 0.2 | M | HIE | Dandy Walker Sd/West Sd/Heart Disease/cataracts | 133 | 133 | Isolated bed | Tracheostomy | Discharge | 214 |
| 8 | 5.1 | M | Lowe syndrome | Multiple organ failure | 9 | 10 | ICU | Orotracheal tube | Death | 0 |
| 9 | 9.5 | M | Unspecified CNS disease | Tracheobronchitis | 12 | 8 | ICU | Orotracheal tube | Death | 0 |
| 10 | 1.0 | F | HIE | Preterm birth | 34 | 382 | Infirmary | Tracheostomy | Death | 5 |
| 11 | 0.3 | F | Trisomy 18 | SGA,LW | 85 | 83 | Infirmary | Tracheostomy | Death | 0 |
| 12 | 0.5 | M | Mitochondrial Myopathy | HIE | 2278 | 2267 | Isolated bed | Tracheostomy | Death | 0 |
| 13 | 2.2 | M | Microcephaly of unknown cause | Seizures | 14 | 12 | ICU | Orotracheal tube | Discharge | – |
| 14 | 3.0 | M | Microcephaly of unknown cause | Seizures | 94 | 13 | ICU | Orotracheal tube | Discharge | – |
| 15 | 0.7 | F | AME type 1 | Respiratory failure | 22 | 106 | ICU | Orotracheal tube | Death | 0 |
| 16 | 3.7 | F | HIE | Pneumonia/ARDS/PIVH grade IV | 60 | 60 | ICU | Orotracheal tube | Discharge | – |
| 17 | 0.77 | F | Congenital Amyoplasia | Short bowel syndrome/malnutrition | 50 | 31 | ICU | Orotracheal tube | Death | 3 |
| 18 | 0.96 | F | SMA type 1 | Respiratory failure | 95 | 88 | UTI | Orotracheal tube | Death | 0 |
| 19 | 4.17 | M | HIE | Seizures | 1 | 1267 | Infirmary | Tracheostomy | Discharge | – |
ARDS, acute respiratory distress syndrome; CNS, central nervous system; F, female; HIE, hypoxic-ischemic encephalopathy; HIJPII, Hospital Infantil João Paulo II; ICU, intensive care unit; LW, low weight; M, male; MV, mechanical ventilation; PIVH, peri-intraventricular hemorrhage; Sd, syndrome; SGA, small for gestational age; SMA, spinal muscular atrophy.
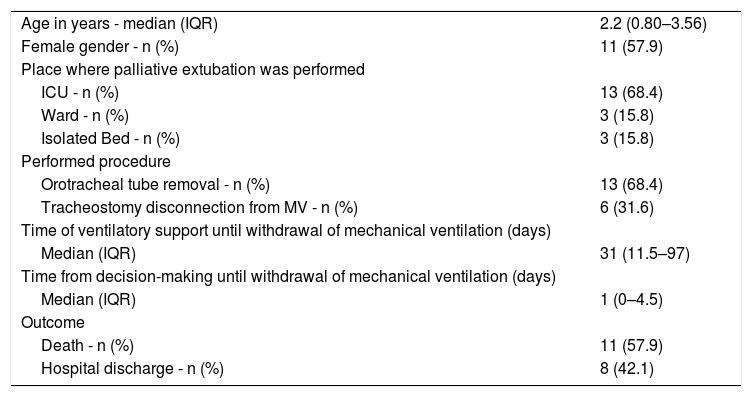
The mean age of patients submitted to palliative extubation was 2.2 years; most extubations were performed in the ICU (intensive care unit) and most patients were on mechanical ventilation for more than 30 days (Table 2).
Characteristics of patients submitted to palliative extubation at HIJPII between 2013 and 2018 (n=19).
| Age in years - median (IQR) | 2.2 (0.80–3.56) |
| Female gender - n (%) | 11 (57.9) |
| Place where palliative extubation was performed | |
| ICU - n (%) | 13 (68.4) |
| Ward - n (%) | 3 (15.8) |
| Isolated Bed - n (%) | 3 (15.8) |
| Performed procedure | |
| Orotracheal tube removal - n (%) | 13 (68.4) |
| Tracheostomy disconnection from MV - n (%) | 6 (31.6) |
| Time of ventilatory support until withdrawal of mechanical ventilation (days) | |
| Median (IQR) | 31 (11.5–97) |
| Time from decision-making until withdrawal of mechanical ventilation (days) | |
| Median (IQR) | 1 (0–4.5) |
| Outcome | |
| Death - n (%) | 11 (57.9) |
| Hospital discharge - n (%) | 8 (42.1) |
ICU, intensive care unit; MV, mechanical ventilation.
After extubation, 11 patients (57.9%) died in the hospital. One patient died during the reduction of mechanical ventilation parameters before disconnection; only one patient died within the first hour after withdrawal of ventilatory support, and another four died between one and six hours. The time between withdrawal of mechanical ventilation and in-hospital death ranged from 15min to five days, with a median of four hours and 20min. Among the eight patients discharged from the hospital, six were intubated, two in the first intubation and the others with previous extubation failures. All had indication of tracheostomy due to neurological symptoms, airway protection difficulty, and superficial breathing pattern. The other two patients discharged from the hospital had received mechanical ventilation through tracheostomy for 133 and 1267 days, respectively, with previous disconnection failures; the latter came from home to palliative extubation. In the first year after discharge, three patients died between 50 and 214 days after extubation and one patient died two years after hospital discharge.
Regarding the type of ventilatory support, six patients had a tracheostomy cannula and 13 an endotracheal tube at the time of the palliative extubation. The mean time during which patients received ventilatory support before extubation was 188 days among patients discharged from the hospital and 276 days among those who died during hospitalization. After excluding from the analysis the three patients who remained for more than six months on ventilation before palliative extubation, the means were similar in both groups: 34 and 43 days, respectively.
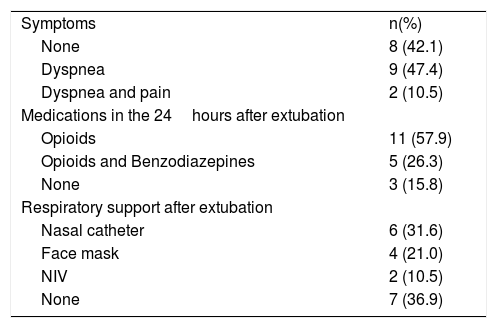
Eight patients did not receive medication as preparation for extubation; nine patients received corticosteroids, six received atropine, and five received scopolamine. All palliative extubations were performed during the day, and among them, four were performed in the afternoon period. No discomfort symptoms were observed in eight patients after the palliative extubation, but five of them were receiving morphine and one patient, fentanyl. The main symptoms, medications, and respiratory support used after palliative extubation are described in Table 3.
Observed symptoms, medications, and support after palliative extubation.
| Symptoms | n(%) |
| None | 8 (42.1) |
| Dyspnea | 9 (47.4) |
| Dyspnea and pain | 2 (10.5) |
| Medications in the 24hours after extubation | |
| Opioids | 11 (57.9) |
| Opioids and Benzodiazepines | 5 (26.3) |
| None | 3 (15.8) |
| Respiratory support after extubation | |
| Nasal catheter | 6 (31.6) |
| Face mask | 4 (21.0) |
| NIV | 2 (10.5) |
| None | 7 (36.9) |
NIV, noninvasive ventilation.
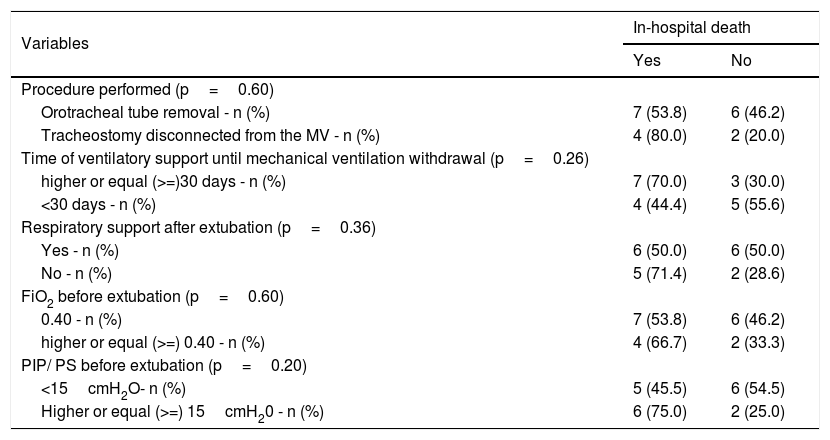
The duration of mechanical ventilation, use of endotracheal tube or tracheostomy cannula, the offer of respiratory support after extubation (oxygen or noninvasive ventilation), and the ventilatory parameters before extubation were not associated with in-hospital death (hospital discharge or death) – Table 4.
Characteristics of patients who died in the hospital after palliative extubation (n=19).
| Variables | In-hospital death | |
|---|---|---|
| Yes | No | |
| Procedure performed (p=0.60) | ||
| Orotracheal tube removal - n (%) | 7 (53.8) | 6 (46.2) |
| Tracheostomy disconnected from the MV - n (%) | 4 (80.0) | 2 (20.0) |
| Time of ventilatory support until mechanical ventilation withdrawal (p=0.26) | ||
| higher or equal (>=)30 days - n (%) | 7 (70.0) | 3 (30.0) |
| <30 days - n (%) | 4 (44.4) | 5 (55.6) |
| Respiratory support after extubation (p=0.36) | ||
| Yes - n (%) | 6 (50.0) | 6 (50.0) |
| No - n (%) | 5 (71.4) | 2 (28.6) |
| FiO2 before extubation (p=0.60) | ||
| 0.40 - n (%) | 7 (53.8) | 6 (46.2) |
| higher or equal (>=) 0.40 - n (%) | 4 (66.7) | 2 (33.3) |
| PIP/ PS before extubation (p=0.20) | ||
| <15cmH2O- n (%) | 5 (45.5) | 6 (54.5) |
| Higher or equal (>=) 15cmH20 - n (%) | 6 (75.0) | 2 (25.0) |
FiO2, Fraction of inspired oxygen; PIP, Peak inspiratory pressure; PS, Pressure support.
Pediatricians often care for patients with chronic and irreversible diseases, permanently dependent on artificial mechanical ventilation, restricted to a hospital bed for months or years, who may experience great suffering caused by invasive procedures. These patients are often accompanied by their mothers, who delegate the care of their healthy children to relatives, abandon home responsibilities, end relationships and leave the labor market, with severe social and financial impacts.
Pediatric care should be practiced to promote the best treatment for the child. While it is generally assumed that offering life support measures is the best choice, there are situations in which withholding or withdrawing life support measures is ethically appropriate or even recommended. In children with severe and irreversible conditions, maintaining invasive treatments might be no longer beneficial and may become deleterious, as it is associated with side effects and intense suffering, for both the child and the family. The decision-making regarding the maintenance and/or withdrawal of life support measures should be based on the ethical principle regarding the best interests of the child, which, while in some situations may seem highly subjective and difficult to define, should be the focus of health professionals when they are defining the appropriate care goals. The process of withdrawal and/or witholding of life-support treatment presupposes a shared decision based on respectful and honest communication between team members, the patient and the family.4
One of the most difficult and most common decisions for doctors and parents regarding withdrawal of artificial life support is the discontinuation of mechanical ventilation.5
The first reported palliative extubation case occurred in 1975 in New Jersey. A young woman named Karen Ann Quinlan remained in a permanent vegetative state following an episode of prolonged cardiopulmonary arrest. Her life was maintained by mechanical ventilation and artificial feeding through a gastrostomy tube. After withdrawal of support, to the surprise of doctors and her parents, Karen was able to assume and maintain adequate breathing patterns, lived for 10 years in a vegetative state, and died in 1986 from pneumonia.6
Mark et al. carried out a review on the prevalence of life support withdrawal in adults admitted to intensive care units in different countries around the world and found that the prevalence of withdrawal of support measures ranged from 0% in Israel to 84.1% in the United States.3 In Brazil, although still incipient and scarcely reported, there was a 30% increase in ICU life support limitation actions between 1988 and 2002, which increased from 6% in 1988 to 36% in 2002, although non-resuscitation orders were the main type of limitation. There was also an increase in family participation in the decision-making process, from 22% in 1988 to 55% in 2002.7,8
In 2008, a study published in Brazil evaluated the incidence of life support limitation in the last 48h of children's lives in seven pediatric intensive care units in the South, Southeast, and Northeast of Brazil, analyzing the medical records of 428 patients.2 Lago et al. identified that most supportive limitation actions comprised the decision not to perform cardiopulmonary resuscitation (CPR) in the event of cardiopulmonary arrest. Life support measures were withdrawn or reduced in only 2.5% of patients who did not receive CPR, such as decreased inotropic drugs or ventilatory support in the last 48h of life. Inotropic infusion was maintained or increased in 66% of patients with non-resuscitation orders and 48.3% of patients had mechanical ventilation settings increased in the last 48h of life. It is noteworthy that only 52.5% of patients with support limitation had the decision to limit support clearly recorded in their medical records.2,7,8
In the present study, the decision-making process and care plan, including the withdrawal of ventilatory support, were described in detail in all medical records of patients who were submitted to palliative extubation. The main factors that may have contributed to the proper documentation were as follows: the procedure and documentation by a team trained in palliative care, previous case discussions by a multidisciplinary team, shared decision with the family, and greater knowledge of ethical and legal aspects that support the interruption of advanced life support.9,10
Several authors have described institutional guidelines and protocols for palliative extubation.1,6,11–13 In this series of patients, withdrawal of mechanical ventilation or endotracheal tube removal was performed after the progressive reduction of ventilatory parameters. Although both withdrawal without prior reduction in ventilatory parameters and disconnection following weaning have been described in the literature, Robert et al. described that symptoms of upper respiratory obstruction and gasping tend to be more prevalent when disconnection is made without weaning, requiring greater attention from the palliative care team to address symptoms. Moreover, the team’s stress tends to be less when disconnection is preceded by progressive weaning from mechanical ventilation.11
Regarding the prevalent symptoms after withdrawal of ventilatory support and its treatment, data available in the literature are very similar to those described in the present study. The main symptoms were dyspnea and pain, and the main drugs used to control symptoms were opioids and benzodiazepines.14,15
Although the withdrawal of ventilatory support usually results in death within a few minutes, in some cases the patient can survive for days, weeks, or months, as it is not the withdrawal of mechanical ventilation that causes death, but rather the disease itself. Explaining this to parents is crucial for them to prepare themselves for all possible outcomes, as well as to comfort them, absolving them of the responsibility of having authorized the death of their loved one.5 The family should be encouraged to spend as much time as possible with the child, hold the child, participate in their bathing and care, and ensure that all symptoms are adequately controlled by the team.
Some researchers have identified characteristics that can predict the time between withdrawal of ventilatory support and death. Shore et al., in 2012, and Das et al., in 2016, used the Dallas Predictor Tool on children to predict the time between withdrawal of life support and death in ICU patients under 18, and identified the factors associated with reduced survival time after withdrawal of ventilatory support measures, as follows: age ≤1 month, absence of spontaneous breathing, need for elevated ventilatory support parameters, use of high doses of vasoactive and/or inotropic drugs, and use of cardiopulmonary bypass. The mean times between life support withdrawal and death were 17 and 25min, respectively.16,17 In another study evaluating adult patients, Cooke and Huynh noted that elderly, non-white patients, with failure of two or more organs, with surgical pathologies, using vasopressor drugs or intravenous fluids before extubation, and using FiO2>70% had a shorter survival after palliative extubation. The mean survival times were 56 and 54min, respectively.18,19 In the present study, however, the mean time of survival after mechanical ventilation withdrawal was much longer than that described by other authors, and it was not possible to identify any characteristic that correlated with in-hospital death after ventilatory support withdrawal, with 42.1% of patients being discharged.
The main hypothesis for this finding, in addition to the small number of patients in the sample, is the characteristics of the patients: they had chronic diseases, were hemodynamically stable, and were supported with low mechanical ventilation settings. Most patients with severe neurological sequelae develop chronic respiratory failure over the years, due to a reduced level of consciousness, muscle weakness, chest deformities, postural changes, and reduced forced vital capacity, resulting in ineffective coughing for sputum production, microaspiration, and accumulation of secretions in the airways, aggravated by the association of disordered swallowing. In this context, the decision to withdrawmechanical ventilation without a plan for reintubation was performed together with the family. In addition to intensifying measures to control symptoms such as dyspnea and sialorrhea, no routine laboratory tests were performed, and oxygen saturation monitoring was interrupted.
In all the above mentioned studies, the patients were unstable, were admitted to an intensive care unit, and in the case of the studies by Shore et al. and Das et al., they were being considered for organ donation after circulatory death.16,17 The use of accurate scores for predicting the time of death after withdrawal of life support is especially important in countries such as the United States, where the removal of organs for donation is authorized when there is circulatory death, differently from Brazil, where organ retrieval is only authorized when brain death is diagnosed.
Although the hospital where the study was carried out had a team specialized in home care, none of the palliative extubations were performed at home. Some authors emphasize the importance of parental choice regarding the environment at the end of a child's life, considering aspects related to the preservation of privacy and feeling of security, because they are in a familiar environment. Performing the palliative extubation at the child's home can give the parents a greater sense of control over the situation. Such a feeling can help with the grieving process.20 A study conducted in Boston, in the United States, interviewed parents who chose to carry out their children’s end-of-life care at home, including palliative extubation. All of them reported the experience as a positive and very significant one, and expressed their gratitude, giving everyone the opportunity to say goodbye and eliciting memories of comfort and a sense of closure.21 However, several authors draw attention to the fact that palliative extubation in an out-of-hospital setting requires even more accurate planning, which includes everything from transportation between the hospital and home to the care to be performed at home.14,22–24 Because survival time cannot be predicted, a detailed care plan for symptom control at home is required, as well as planning for postmortem support, including provision of the death certificate and coordinating the funeral service.
The present study is limited by the small sample size, which may explain why it was not possible to identify predictors of survival time after ventilatory support withdrawal, in addition to the accuracy of documentation, a frequent source of error in studies of this type. However, data related to limitation or withdrawal of life support have been thoroughly documented in recent years in this institution.
Palliative extubation is a widely used form of life support limitation and withdrawal worldwide, and has been well described in adults. However, there is a paucity of published studies on this subject involving children, especially in Brazil. It represents an extremely specialized form of care that requires the presence and availability of a multidisciplinary team with adequate training in symptom control and palliative care.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Affonseca CA, Carvalho LF, Quinet RP, Guimarães MC, Cury VF, Rotta AT. Palliative extubation: a five-year experience in a pediatric hospital. J Pediatr (Rio J). 2020;96:652–9.
Stydy conducted at Hospital Infantil João Paulo II, Belo Horizonte, MG, Brazil.