End-stage renal disease is a health problem that consumes public and private resources. This study aimed to identify the cost of hemodialysis (either daily or conventional hemodialysis) and transplantation in children and adolescents.
MethodsThis was a retrospective cohort of pediatric patients with End-stage renal disease who underwent hemodialysis followed by kidney transplant. All costs incurred in the treatment were collected and the monthly total cost was calculated per patient and for each renal therapy. Subsequently, a dynamic panel data model was estimated.
ResultsThe study included 30 children who underwent hemodialysis (16 conventional/14 daily hemodialysis) followed by renal transplantation. The mean monthly outlay for hemodialysis was USD 3500 and USD 1900 for transplant. Hemodialysis costs added up to over USD 87,000 in 40 months for conventional dialysis patients and USD 131,000 in 50 months for daily dialysis patients. In turn, transplant costs in 50 months reached USD 48,000 and USD 70,000, for conventional and daily dialysis patients, respectively. For conventional dialysis patients, transplant is less costly when therapy exceeds 16 months, whereas for daily dialysis patients, the threshold is around 13 months.
ConclusionTransplantation is less expensive than dialysis in children, and the estimated thresholds indicate that renal transplant should be the preferred treatment for pediatric patients.
A Doença Renal em Estágio Final é um problema de saúde que consome recursos públicos e privados. Nosso objetivo é identificar o custo da hemodiálise (hemodiálise diarias ou convencional) e transplante em crianças e adolescentes.
MétodosUma coorte retrospectiva de pacientes pediátricos com Doença Renal em Estágio Final (DREF) submetidos à hemodiálise após transplante de rim. Todos os custos incorridos no tratamento foram cobrados e o custo total mensal foi calculado por paciente e por cada terapia renal. Então, foi estimado um modelo dinâmico com dados em painel.
ResultadosEstudamos 30 crianças submetidas à hemodiálise (16 hemodiálises convencionais/14 hemodiálises diárias) após transplante renal. O gasto médio mensal para hemodiálise foi US$3,5 mil e US$1,9 mil para transplante. Os custos de hemodiálise somam mais de US$87 mil em 40 meses para pacientes submetidos a hemodiálise convencional (HC) e US$131 mil em 50 meses para pacientes submetidos a hemodiálise diária (HD). Por outro lado, os custos de transplante em 50 meses atingem US$48 e US$70 mil, para pacientes submetidos a HC e HD, respectivamente. Para pacientes submetidos à hemodiálise convencional, o transplante é menos oneroso quando a terapia ultrapassa 16 meses, ao passo que para pacientes submetidos a hemodiálise diária o limiar é cerca de 13 meses.
ConclusãoO transplante é menos caro que a diálise em crianças e os limiares estimados indicam que o transplante renal deve ser o tratamento preferencial para pacientes pediátricos.
End-stage renal disease (ESRD) is a disorder characterized by the irreversible loss of kidney function. The disease is a health problem that increases mortality rate, causes a negative impact on the quality of life of patients, and consumes a high amount of resources. Kidney transplantation is the treatment of choice for ESRD in children, and preemptive transplant should be the first therapeutic goal for pediatric patients with this condition.1
In Brazil, a large portion of the budget of the Brazilian Unified Health System (Sistema Único de Saúde [SUS]) is allocated for renal replacement therapies; increased demands are predicted, due to the rising prevalence of the disease.2 The incidence and prevalence of pediatric chronic dialysis in Brazil is 6 and 20 cases per million age-related population (pmarp), respectively,3 and the incidence of pediatric kidney transplantation is 4 pmarp.4 Hemodialysis is three times more used than peritoneal dialysis (75% vs. 25%), and there are regional differences in access to ESRD treatment, which is lowest in the North and Midwest regions.3,4 Inequalities in access to ESRD treatment are not exclusive to Brazil and have a macroeconomic origin.5–8
Given the amount of resources used in the treatment of the disease, various studies estimate the costs of renal replacement therapies. In general, those studies suggest that transplanting younger and healthier individuals and even those with considerable ESRD co-morbidities is cost-effective.9–16
However, most of these studies are based on data from adults, and no study has analyzed the costs of childhood renal replacement therapies in Brazil. Extrapolation from the studies with adults is not appropriate, since ESRD has peculiarities in each age range, making treatment in children and adolescents almost individualized, and thus more complex and expensive.
When considering dialysis treatment alone, recent data indicate that daily hemodialysis promotes better outcomes for children when compared with conventional dialysis.17 Consequently, the interest in daily hemodialysis has increased but, to date, the costs of this therapy have not been evaluated.
In this context, this study aimed to fill these gaps by identifying the costs of hemodialysis (either daily [DHD] or conventional hemodialysis [CHD]) and transplantation in children and adolescents. This is the first analysis in Brazil to compile all costs of different kidney treatment therapies in children.
MethodsThe authors report on a single-center cohort of 30 pediatric patients with ESRD who were treated between 2007 and 2013, all of whom underwent hemodialysis followed by kidney transplantation at Hospital Samaritano. The convenience sample was drawn from the 168 pediatric kidney transplants that were performed during the study period. Data were retrospectively collected for all treatment costs including material, medicine, equipment, medical fees, administrative costs, daily rates of hospitalization, physiotherapy, nutrition, nursing, administrative fees, equipment, wages, and laboratory tests.
The monthly total costs were calculated for each patient on hemodialysis and transplantation (by the official price index [IPCA]). The mean accumulated cost for each of the therapies was then calculated.
Two data sources were used: the administrative database from the Hospital, with cost information for both types of therapies and the classification in billing procedures and the NEFRODATA software (version 5.12–LifeSys, Divinópolis, MG, Brazil), with detailed information on material and medicine for hemodialysis.
The main outcome was the total monthly cost per patient, adding variable costs, other variable expenses (items not billed to the patient, such as usage of laundry facilities) and fixed costs (administrative rates, apartments, and operating rooms). As patients were followed during different periods, all values were converted into November 2013 U.S. dollars using the official inflation rate and the mean exchange rate for that month,1 in order to compare costs.
The analysis of costs of hemodialysis was performed categorizing patients into two types: those who underwent CHD and those who underwent daily hemodialysis DHD, each patient belonging to only one type of treatment. In theory, patients on DHD present double the dialysis costs when compared with those undergoing CHD, thus significantly affecting the costs.
Two time variables were constructed: one calculating the time (months) that each patient spent on hemodialysis therapy and the other calculating the transplant and duration of follow-up therapy.
Statistical methodsDescriptive analysisFirstly, the evolution of the mean monthly cost in different renal therapies was calculated by averaging the total cost in each month over the number of patients. The values considered are only for months with at least two patients.
Comparisons of groupsQuantitative variables between the groups (DHD vs. CHD) were compared using the Mann–Whitney test, while the Wilcoxon matched-pairs test was used to compare treatments (hemodialysis vs. transplantation). The chi-squared or Fisher's exact test were used to compare proportions. In all tests, the limit of 5% (p<0.05) to reject the null hypothesis was adopted.
Subsequently, an econometric model was estimated in order to control for within-patient heterogeneity and generate predictions as function of past values, while also quantifying the uncertainty with confidence intervals.
Econometric analysisSince the 30 patients were observed over different periods in hemodialysis and following transplantation, the framework chosen was that of a dynamic panel with asymptotics in the cross-sectional dimension and fixed time.
Taking the cross-sectional heterogeneity and the autocorrelation into account, the following model was formed:
where j indexes whether the patient was in hemodialysis or transplant and whether he/she is undergoing CHD or DHD treatment. Index i refers to the patient and t, to the time. Variable yit is the total mean monthly cost that patient i had in the t-eth month in treatment.The model allows for fixed effects, ai, so that each patient might have a different recurring level of expenses compatible with his/her physical condition (such as age and weight) and how well he/she responds to treatment. The quadratic trend captures the smooth or intense fall in monthly costs over the duration of treatment. Finally, the inclusion of lagged dependent variables models the temporal structure.
The econometric errors εitj are independently and identically distributed over time and patients, but robust standard errors are also employed for heteroscedasticity.
As is common in the dynamic panels literature, the inclusion of lagged dependent variables in the model generates a bias when time is fixed and the within or first-differences estimator is used. Therefore, the estimator employed is the system GMM that instruments the transformed endogenous variables and the level endogenous variables by lagged levels and first-differences of the dependent variable.
Considering that the study was performed through analysis of secondary data from databases and did not require any intervention or even any procedure with patients, the ethics committee of the institution approved the project without the need to obtain informed consent from patients and parents (Process No.: 321.698).
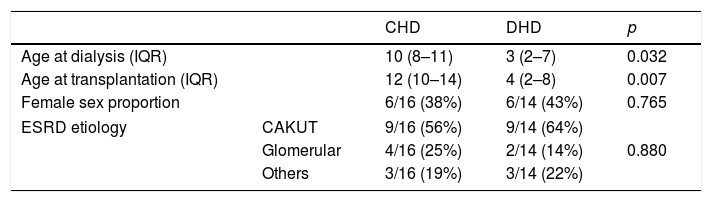
ResultsThe study sample involved 30 children (18 boys/12 girls) who underwent hemodialysis (16 CHD/14 DHD) followed by renal transplantation. The main etiology of ESRD was congenital anomalies of the kidney and urinary tract (CAKUT) in 18 patients (60%), and the mean age at transplantation was 9 years (SD=5). In 25 cases (83%), transplant was from deceased donors. The median duration of each therapy was 20 (IQR=10–31) months for hemodialysis, while median transplant therapy was 27 (IQR=20–33) months (p=0.028).
Table 1 presents the demographic and clinical data of the sample.
Demographic and clinical data of the studied sample according to type of dialysis before transplantation.
| CHD | DHD | p | ||
|---|---|---|---|---|
| Age at dialysis (IQR) | 10 (8–11) | 3 (2–7) | 0.032 | |
| Age at transplantation (IQR) | 12 (10–14) | 4 (2–8) | 0.007 | |
| Female sex proportion | 6/16 (38%) | 6/14 (43%) | 0.765 | |
| ESRD etiology | CAKUT | 9/16 (56%) | 9/14 (64%) | |
| Glomerular | 4/16 (25%) | 2/14 (14%) | 0.880 | |
| Others | 3/16 (19%) | 3/14 (22%) | ||
CHD, conventional hemodialysis; DHD, daily hemodialysis; IQR, interquartile range; CAKUT, congenital anomalies of the kidney and the urinary tract; ESRD, end-stage renal disease.
One observation concerning an item that was in the dataset and was unrelated to renal therapies (a Cochlear implant, which is a high one-off cost [USD 34,900]) was dropped. This single observation would have increased the mean cost of hemodialysis.
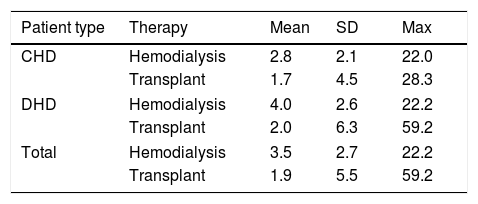
Combining the different monthly costs per patient, the mean cost of hemodialysis was USD 3500 and USD 1900 for transplant, according to Table 2. Half of the patients had cost equal to or lower than USD 3300 per month for hemodialysis and USD 120 for transplant. In turn, the highest sum incurred in a month was higher for transplant, reaching USD 59,200 vs. USD 22,200 for HD. This indicates that, overall, transplants initially have higher costs, but in the long run they are more economical.
Mean monthly costs per type of treatment (in thousand USD).
| Patient type | Therapy | Mean | SD | Max |
|---|---|---|---|---|
| CHD | Hemodialysis | 2.8 | 2.1 | 22.0 |
| Transplant | 1.7 | 4.5 | 28.3 | |
| DHD | Hemodialysis | 4.0 | 2.6 | 22.2 |
| Transplant | 2.0 | 6.3 | 59.2 | |
| Total | Hemodialysis | 3.5 | 2.7 | 22.2 |
| Transplant | 1.9 | 5.5 | 59.2 | |
CHD, conventional hemodialysis; DHD, daily hemodialysis.
Subdividing the costs by billing group, it was observed that patients in HD had the following distribution: (a) medications and material=64%, (b) prosthesis and orthesis=15%, (c) hospital services=17% and (d) diagnostic medicine service=4%. Transplant patients costs were divided as: (a) medications and material=49%, (b) prosthesis and orthesis=9%, (c) hospital services=35% and (d) diagnostic medicine service=7% (p=0.014).
Analyzing separately CHD and DHD patients, the mean monthly cost of DHD was higher, at USD 4000 (Table 2).
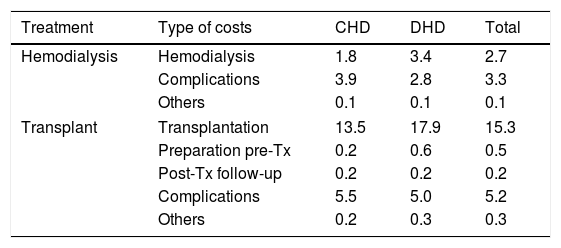
It is noteworthy that transplant initially requires high expenditure, but its cost subsequently decelerates, eventually resulting in an overall savings over the average incurred for hemodialysis. It is estimated that the accumulated costs for transplant can reach USD 43,600.00 in the first month and gradually increase in the follow-up period. After two years of treatment, the accumulated cost post-transplant rises to between USD 43,600.00 and USD 65,368.00 on average, as opposed to double the cost that is observed in hemodialysis for the same period. Expenses with transplant are, on average, also higher for DHD patients by almost USD 4580. However, costs of treating complications are similar for both groups (Table 3).
Mean monthly costs for types of treatment (in thousand USD).
| Treatment | Type of costs | CHD | DHD | Total |
|---|---|---|---|---|
| Hemodialysis | Hemodialysis | 1.8 | 3.4 | 2.7 |
| Complications | 3.9 | 2.8 | 3.3 | |
| Others | 0.1 | 0.1 | 0.1 | |
| Transplant | Transplantation | 13.5 | 17.9 | 15.3 |
| Preparation pre-Tx | 0.2 | 0.6 | 0.5 | |
| Post-Tx follow-up | 0.2 | 0.2 | 0.2 | |
| Complications | 5.5 | 5.0 | 5.2 | |
| Others | 0.2 | 0.3 | 0.3 | |
CHD, conventional hemodialysis; DHD, daily hemodialysis.
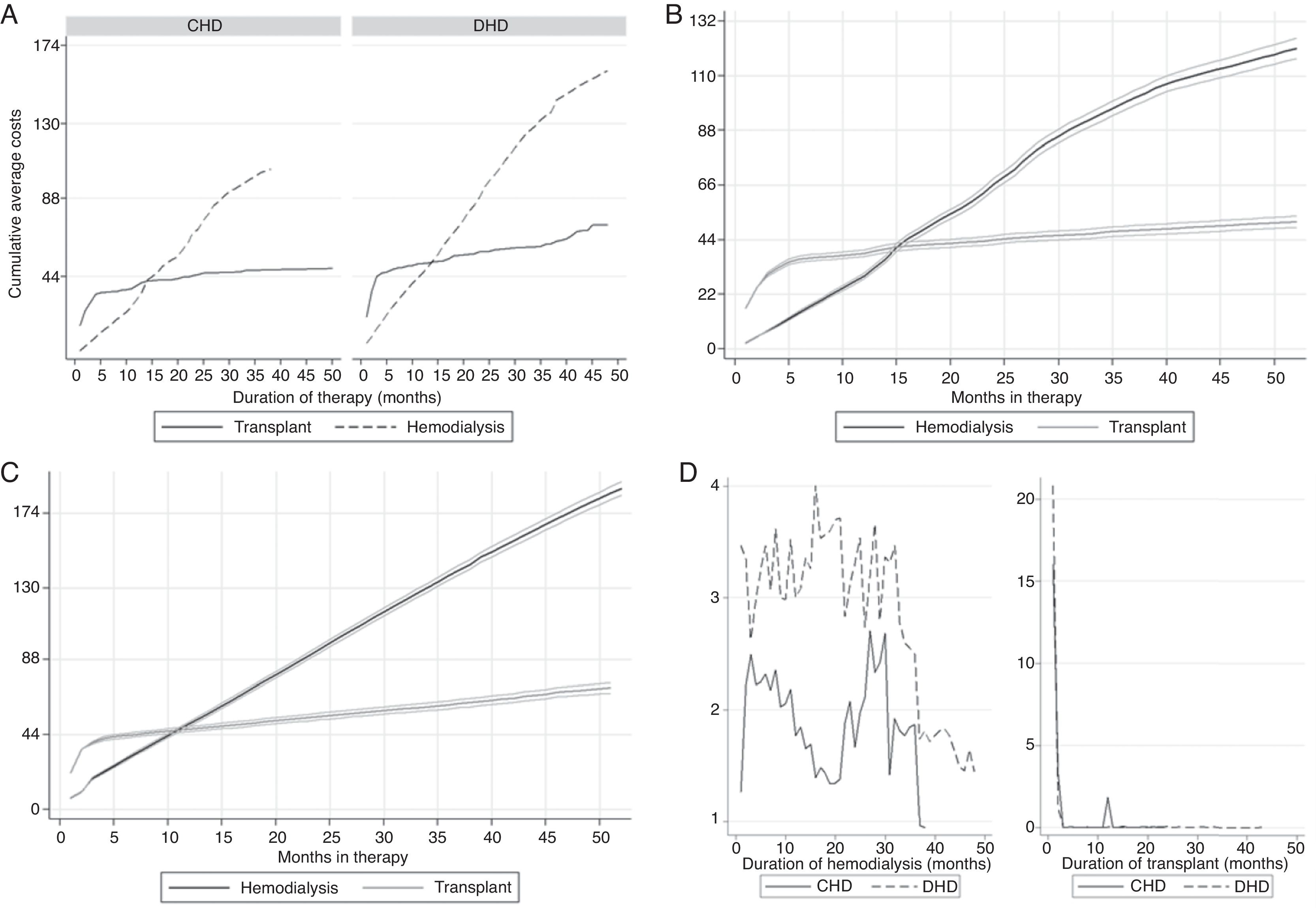
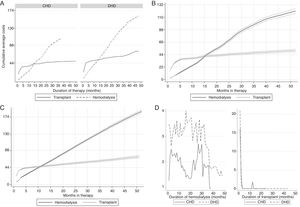
Fig. 1A presents the evolution of the mean monthly cost of different renal therapies, by averaging the total sample cost for each month. It shows that hemodialysis costs add up to over USD 87,000 in 40 months for CHD patients and USD 131,000 in 50 months for DHD patients. In turn, transplant costs in 50 months reach USD 48,000 and USD 70,000 for CHD and DHH patients, respectively. It is noteworthy that the gap between the transplant cumulative costs for CHD patients and DHD patients increase early post-transplant, since most expenses are incurred in the first few months.
A, cumulative mean monthly costs comparing hemodialysis and transplant, by patient type (in thousand USD); B, testing for statistically significant differences in cumulative costs: CHD (in thousand USD); C, testing for statistical differences in cumulative costs: DHD (in thousand USD); D, evolution of the mean monthly cost of hemodialysis sessions (left) and from hospitalization due to transplant (right), by patient type (in thousand USD).
CHD, conventional hemodialysis; DHD, daily hemodialysis.
In summary, a post-transplant threshold duration of therapy appear to exist, where a transplant becomes a more economical option to hemodialysis. In order to statistically estimate this threshold, taking cross-sectional heterogeneity into account and predicting the cost with the same temporal structure, the following section will present an econometric analysis of the data.
Econometric analysisFig. 1B and C plots the average predicted cumulative costs and their confidence intervals at a 95% confidence level based on the dynamic panel estimation (see regression results in the Online Appendix). Both figures clearly show that hemodialysis becomes a more costly option after a threshold duration of therapy. Being conservative, the threshold is identified when the lower bound of hemodialysis confidence interval surpasses the upper bound of transplant confidence interval.
For CHD patients, it is less costly to undergo transplant when therapy exceeds 16 months. In turn, for DHD patients, the threshold arrives earlier, at approximately 13 months. The result is intuitive, since DHD requires twice as much material and medicine, thus inducing a swift rise in cost.
In both cases, the threshold duration corresponds to a cost of around USD 44,000. It is noteworthy that a DHD patient in transplant therapy costs USD 44,000 in under 5 months, but this amount does not surpasses USD 87,000 in 50 months. In turn, DHD costs add up to USD 87,000 in only 24 months (Table 2).
Analysis of hemodialysis and transplant proceduresEven though the economics of the therapies should cover all costs involved, including hospitalization due to complications and pre- and post-transplant exams, for example, it is also interesting to analyze separately, from a management point of view, hemodialysis sessions and transplant hospitalization costs. This subsection analyzes, from an economic standpoint, the evolution of costs for hemodialysis sessions and transplant hospitalizations. Fig. 1D presents the monthly evolution of these costs in hemodialysis and transplant, which do not diverge significantly from the total costs for each therapy. The transplant procedure cost is almost zero after the first two months, contrary to hemodialysis.
DiscussionThe main finding of this research is that transplant in children and adolescents is an economically more attractive therapy after a relatively short threshold of time. Observing 30 patients from 2007 until 2013 and comparing the costs incurred in hemodialysis and transplant, it can be concluded that transplant is a more advantageous therapy from a cost standpoint after 13–16 months post-transplant.
It is impossible to compare the cost differences among hospitals and countries because there are regional variations, but the present results are in agreement with several studies in adults showing that transplant is more economical when compared with dialysis treatment.13,18 Only one study reported that dialysis was less expensive than transplantation, but their patients only underwent two dialysis sessions per week. Moreover, it was a cross-sectional study, and no econometric technique was implemented to model the costs of treatments according to the duration.19
The innovative aspect of the present research is that it was based only on pediatric patients; the findings are relevant because they extend previous concepts that were reported in adults. Also, the fact that this sample included children who underwent daily dialysis before transplantation is original. More frequent dialysis has the potential to reduce malnutrition, cachexia, allowing greater dietary freedom20; these benefits make DHD an interesting option for children, since it promotes growth and lower morbidity.17,21–23 The authors took advantage of the fact that this center regularly performs DHD in small children to study the economic impact of this treatment modality. To the best of the authors’ knowledge, this is the first time that estimation of costs of renal replacement therapies included daily dialysis.
Although a cost-effectiveness analysis was not performed, it is plausible to assume that this ratio would be elevated, since pediatric solid-organ transplants result in a survival benefit of over 25 years in the United States when compared to children who were placed on the waiting list but were not transplanted.24
This study collected and analyzed costs relating to materials, medicine, doctors, administrative, and hospitalization fees, as well as other incidentals, to establish economic parameters for an efficient allocation of resources in renal replacement therapy for the pediatric population. However, even if indirect costs are excluded, such as hospitalizations due to complications and post-transplant consults, the meaning of the results does not change. In fact, the inference that transplant is a more economical therapy in the long run is further corroborated. Considering only hemodialysis session costs (routine exams, hemodialyzer, materials, medicine, and medical fees) and transplant hospitalization costs in this sample, the threshold is reduced from 13 to 16 months to 9 to 15 months. These results are in agreement with those by Sánchez-Escuredo et al., who reported that transplantation resulted in cost savings even in the first year and was 74% less expensive treatment than hemodialysis in the second year after living donor kidney transplantation.15
The present data were based on mean monthly costs; the problem with this approach is that the temporal dependency of the costs is ignored, impeding a robust inference and a more informed prediction. Estimating an econometric model for the evolution of costs allowed to control within-patient heterogeneity and to generate predictions as function of past values, while also quantifying the uncertainty with confidence intervals. The results allowed an analysis of the costs temporal structure while also controlling for cross-section idiosyncrasies of the patients using dynamic panel data methods.
The present results also considered the fact that CHD and DHD patients may be different. DHD has been reported to decrease the length of hospital stay, the weekly dose of erythropoiesis-stimulating agents, and the number of antihypertensive medications when compared with conventional hemodialysis.13,25,26 It is noteworthy that, in the present sample, the costs of DHD were logically greater than CHD, but the cost of complications was numerically lower, suggesting that intensified hemodialysis promotes a lower incidence of complications.21 These inferior complications costs are more notable when considering that the patients who underwent DHD in the present study were younger at the beginning of treatment.
In the 10–30 months range, the mean costs for CHD patients had a higher growth rate than DHD patients, although the overall trend remained a declining one. The authors concluded that this is not due to a change in the costs dynamics of a particular treatment itself, but due to the change in the sample composition, which happens naturally because patients leave treatment over time. As the sample size decreases, the cost estimates become less precise and end up reflecting individual patients idiosyncrasies. In particular, only half of the CHD sample was in treatment after the 20th month; therefore, the mean costs were greatly influenced by any additional leave. The authors consider that the present econometric approach improves upon the simple comparison of mean monthly (cumulative) costs, because it isolates the idiosyncrasies (fixed-effects in the regression) and the estimation of the dynamics parameters is less affected by sample reductions.
The present research has limitations because it is a retrospective single center study involving a reduced number of children for a limited period. Furthermore, the sample included only patients who underwent hemodialysis, and more studies comparing the costs of transplantation with peritoneal dialysis would be welcome. However, the strength of the study is the fact that it addressed a significant question from an economical point of view, involving a developing country with limited resources, since this scenario is not restricted to Brazil. Moreover, robust econometric models were applied, allowing the prediction of the costs for a longer period.
In summary, the present data suggest that treating patients under CHD for over 16 months would be more expensive than the costs of a transplant. Likewise, transplant is less expensive than treating patients with DHD for over 14 months. Transplant becomes a more economical therapy at the USD 43,590.00 threshold, because the postoperative months do not greatly add to the cumulative costs. In turn, hemodialysis demands a continuous monthly spending of resources, reaching twice the cumulative cost of transplant after 30–40 months. Considering only hemodialysis sessions and hospitalization for transplant, the threshold is USD 30,513.00. Considering that the sample patients spent a median time of 20 months on dialysis, transplant is a better alternative for children undergoing substitutive renal therapies.
The thresholds estimated in this study might serve to guide public policy, indicating that renal transplant should be used vis-à-vis hemodialysis for patients of the pediatric population in a long duration therapy.
FundingResearch funded by the Brazilian Ministry of Health through the ‘Programa de Apoio ao Desenvolvimento Institucional do Sistema Único de Saúde – PROADI-SUS’, protocol number: 25000.180613/2011-11.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Camargo MF, Barbosa KS, Fetter SK, Bastos A, Feltran LS, Koch-Nogueira PC. Cost analysis of substitutive renal therapies in children. J Pediatr (Rio J). 2018;94:93–9.
In this study, the IPCA inflation rate was used. Because the Central Bank uses the IPCA index for inflation targeting purposes, it is regarded as the Brazilian official price index. The mean exchange rate for November 2013 was 2.2947 BRL/USD.