to characterize and compare clinical, epidemiological, and laboratory aspects of infants with acute lower respiratory infection (ALRI) associated with the detection of adenovirus (ADV) or respiratory syncytial virus (RSV).
Methodsa preliminary respiratory infection surveillance study collected samples of nasopharyngeal aspirate (NPA) for viral research, linked to the completion of a standard protocol, from children younger than two years admitted to a university hospital with ALRI, between March of 2008 and August of 2011. Polymerase chain reaction (PCR) was used for eight viruses: ADV, RSV, metapneumovirus, Parainfluenza 1, 2, and 3, and Influenza A and B. Cases with NPA collected during the first 24hours of admission, negative results of blood culture, and exclusive detection of ADV (Gadv group) or RSV (Grsv group) were selected for comparisons.
Resultsthe preliminary study included collection of 1,121 samples of NPA, 813 collected in the first 24hours of admission, of which 50.3% were positive for at least one virus; RSV was identified in 27.3% of cases surveyed, and ADV was identified in 15.8%. Among the aspects analyzed in the Gadv (n = 58) and Grsv (n = 134) groups, the following are noteworthy: the higher mean age, more frequent prescription of antibiotics, and the highest median of total white blood cell count and C-reactive protein values in Gadv.
ConclusionsPCR can detect persistent/latent forms of ADV, an aspect to be considered when interpreting results. Additional studies with quantitative diagnostic techniques could elucidate the importance of the high frequency observed.
caracterizar e comparar aspectos clínicos, epidemiológicos e laboratoriais de lactentes com evidências de infecção aguda do trato respiratório inferior (IATRI) associada à detecção do adenovírus (ADV) ou do vírus sincicial respiratório (VSR).
Métodosum estudo preliminar de vigilância de infecções respiratórias desenvolveu coleta de aspirado nasofaríngeo (ANF) para pesquisa viral, vinculada ao preenchimento de protocolo padrão, de menores de dois anos internados com quadro de IATRI em hospital universitário, entre março de 2008 e agosto de 2011. Utilizou-se técnica da reação em cadeia da polimerase (PCR) para oito vírus: ADV, VSR, metapneumovírus, parainfluenza 1, 2 e 3 e influenza A e B. Foram selecionados para comparações os casos com ANF coletado nas primeiras 24horas da admissão, resultado de hemocultura negativo e detecção exclusiva de ADV (grupo Gadv) ou VSR (grupo Gvsr).
Resultadoso estudo preliminar incluiu coleta de 1.121 amostras de ANF, sendo 813 coletadas nas primeiras 24h da admissão, das quais 50,3% foram positivas para ao menos um dos vírus, com VSR em primeiro lugar, em 27,3%, e ADV em segundo, em 15,8% dos casos pesquisados. Dentre os aspectos analisados nos grupos Gadv (n=58) e Gvsr (n=134), destacaram-se a média da idade mais elevada, maior frequência da prescrição de antibióticos e medianas mais elevadas para contagem total de leucócitos e valores da proteína C-reativa no Gadv.
Conclusõesa PCR utilizada pode detectar formas persistentes/latentes de ADV, aspecto a ser considerado ao interpretar os resultados. Estudos complementares com técnicas diagnósticas quantitativas, por exemplo, poderiam evidenciar a importância da elevada frequência verificada.
In developing countries, acute lower respiratory infections (ALRIs) have a significant role among the general population. They are the first cause of death in low-income countries and the fourth in middle-income countries, such as Brazil.1
The main etiological agents involved are viruses and bacteria, and currently, more sensitive diagnostic techniques support the theory that viral-bacterial coinfection are common and increase the severity of pneumonia cases, probably due to inhibition of pulmonary antibacterial defenses.2 This hypothesis is supported by the reduced need for hospitalizations for pneumonia associated with viral infections among children vaccinated against pneumococcus, as observed in some countries.3,4
Adenoviruses (ADVs) are responsible for 1% to 5% of all respiratory infections5 and 5% to 10% of childhood pneumonias,6 with a peak incidence around the age of 2 years,7,8 and may be associated with fatal cases or sequelae that can result in clinical manifestation for years after the initial infection. A recent meta-analysis of relevant studies published in the last 40 years on major (restrictive/obstructive lung disease and bronchiectasis) as well as minor (including asthma) sequelae of pneumonia in childhood, concluded that ADV pneumonia is associated with higher risk of sequelae, among other possible analyzed factors, such as need for hospitalization and age younger than two years.9
Laboratory techniques used for ADV screening include cell cultures, immunofluorescence (IF), and serology, which are more traditional, as well as more modern and sensitive molecular techniques such as polymerase chain reaction (PCR),10,11 and they do not always indicate infection, but simply viral presence or excretion.The persistence capacity of ADVs in different tissues is well known, including the upper12 and lower13 respiratory airways of asymptomatic children.
When analyzing data related to admissions of children younger than 2 years with evidence of ALRI, the clinical, epidemiological, and laboratory aspects of cases in which only ADV was identified, among different respiratory viruses screened by PCR in samples of nasopharyngeal aspirate (NPA) was characterized and compared with cases in which only respiratory syncytial virus (RSV), considered the main ALRI agent in infants and young children, was identified.14,15
MethodsData selected for this descriptive study was obtained from a preliminary prospective ALRI surveillance project in children hospitalized at the Department of Pediatrics and Child Care of the Hospital Central da Santa Casa de Misericórdia de São Paulo between March of 2008 and August of 2011. This study was approved by the ethics committee on human research of the institution.16 The service, located downtown, performs approximately 60,000 emergency room consultations and 60,000 urgent and emergency care consultations annually in children aged 0 to 14 years.
Patient selectionThe preliminary project included the enrollment of children younger than 2 years hospitalized with a syndromic diagnosis of ALRI, according to an adaptation of the definitions developed by WHO,17 including family and/or medical report of cough and/or respiratory distress (difficulty breathing characterized by tachypnea, for the age group, and/or persistence of chest wall, and/or sternal notch retractions, and/or use of accessory respiratory muscles in a calm child), and/or those who had one or more of the following clinical diagnoses established by the medical staff responsible for emergency care and hospitalization: bronchiolitis, pneumonia, wheezing or bronchospasm laryngotracheobronchitis, pertussis-like syndrome, cyanosis, and apnea.
Multiple inclusions were accepted, provided that each case represented a new ALRI episode (with medical and/or parental report of full resolution and/or return to baseline status for an unspecified time interval before a new episode). The time of onset was not restricted, allowing for the inclusion of patients who had chronic diseases with recurrent clinical manifestations, such as cough in patients with asthma or heart disease, possibly overlapping those commonly observed during the course of respiratory viral infections. Based on the cases included in the preliminary study, cases in which the NPA samples were collected after 24hours of hospitalization were initially excluded from this analysis, to ensure that the profile of community-acquired viral infections was recorded.18 From these selected cases, those that had positive blood culture results for bacteria and/or fungi were excluded when compared with those that presented exclusive detection of ADV or RSV.
ProceduresThe search for eligible cases, coordinated by the researcher in charge of the preliminary study, was conducted from Monday to Friday between 8 am and 12 pm, for operational reasons, at the pediatric emergency room unit. After the informed consent was signed by the legal guardian, the patient was included in the study, and a protocol was completed with information related to the following domains: demographic data, signs and symptoms, personal and family history, environmental conditions, admission diagnoses, complementary examinations, initial treatment, and clinical outcome.
Sample collectionSamples were collected through a cannula adapted to a vacuum-connected, saline-drip chamber introduced through the nostril up to the nasopharynx. After collection, the NPA sample was immediately stored under refrigeration (4°C to 6°C), and then fractionated into three aliquots and stored in liquid nitrogen. Weekly, the aliquots were properly screened, and inadvertently repeated or inadequate samples were excluded. Samples transported to the Laboratory of Clinical and Molecular Virology of the Instituto de Ciências Biomédicas da Universidade de São Paulo, where they were kept at a temperature of -70°C until viral analysis.
Sample processingThe following viral agents were screened: RSV, influenza virus (FLU) A and B, parainfluenza virus (PIV) 1, 2, and 3, metapneumovirus (MPV), and ADV. The PCR technique was used, starting by extracting viral genetic material (RNA/DNA) from a fraction of 500μL of each NPA sample, using an automated extraction system according to instructions from the manufacturer of the chosen lysis buffer (NucliSens® Iso Kit - BioMérieux).
In the case of viruses whose genetic material was RNA (RSV, FLU, MPV, and PIV), reverse transcription PCR was performed using the MultiScribe Reverse Transcriptase enzyme according to instructions of the manufacturer of the High Capacity cDNA Archive Kit (Applied Biosystems), in order to obtain the complementary DNA (cDNA). After the cDNA/DNA was obtained, PCR was initiated, employing Taq DNA Polymerase (Biotools) for amplification in an automated thermocycler (GeneAmp PCR System 9700 - Applied Biosystems).
The primers used allowed for the amplification of part of the gene that corresponds to one of the polypeptides that comprise the viral capsid common to the several serotypes of human ADV. The amplified product was submitted to agarose gel electrophoresis (Gibco - BRL) prepared with ethidium bromide, for later reading and recording of the DNA bands on the gel in an ultraviolet transilluminator (UV-MacroVue 20 - Hoefer), comparing them to known controls to identify the genetic material.
Groups for analysisBased on the cases initially selected for this study, two groups were created for analysis (both with negative blood cultures), according to the PCR results: the Gadv group, which included cases with positive PCR exclusively for ADV, and the Grsv group, which included cases with positive PCR exclusively for RSV, compared to the other viruses studied.
Statistical analysisIn the bivariate analysis, the chi-squared test or Fisher's exact test were used for qualitative variables, and Student's t-test or the Mann-Whitney test were used for quantitative variables. The Statistical Package for Social Sciences (SPSS) for Windows® release 13.0 (SPSS Inc. - Chicago, IL, USA) was used for the statistical analyses, and the statistical significance level was set at 5%.
ResultsThe preliminary study incorporated 1,121 NPA samples. After excluding repeated or inadequate samples and applying the inclusion criteria, 813 samples were initially selected, corresponding to different episodes of suspected ALRI that occurred in 712 children. Of these, 633 (88.9%) were included only once.
Among the conclusive cases that were initially selected, 50.3% (409/813) samples were positive for at least one of the viruses studied, with RSV present in 27.3% (222/813), ADV in 15.8% (128/813), PIV in 7.2% (59/813), MPV in 4.8% (39/813), and FLU in 4.5% (37/813) of the cases studied.
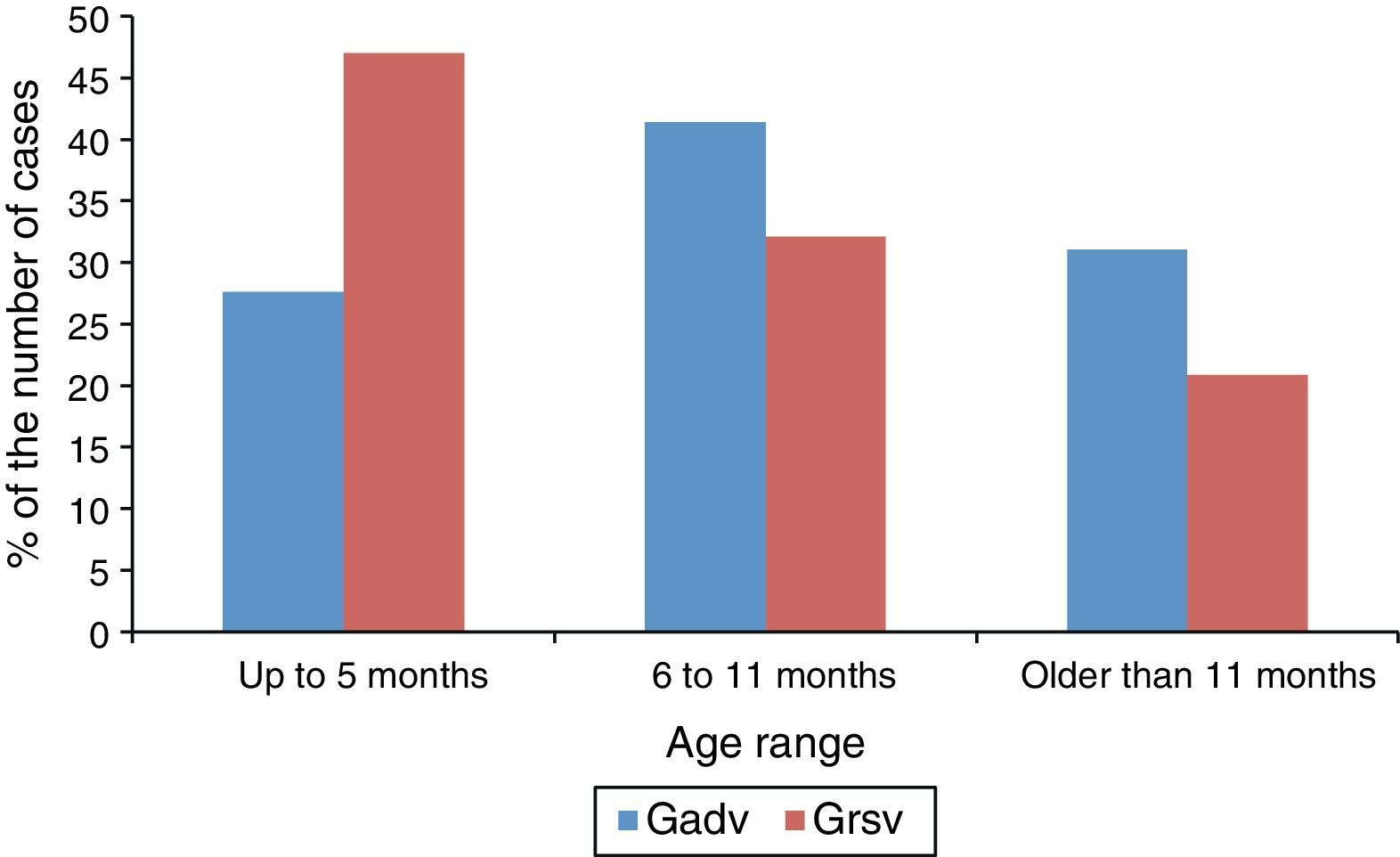
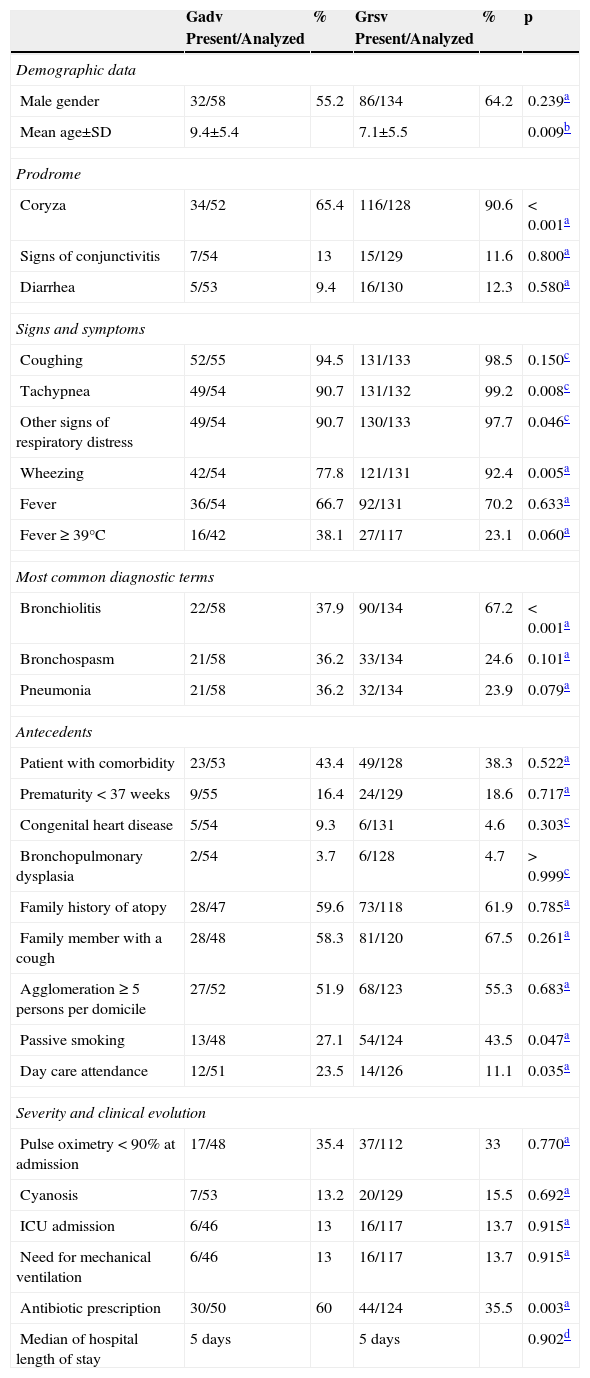
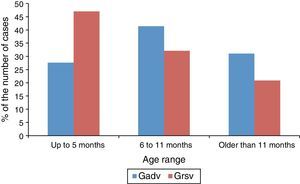
A total of 637/712 (89.5%) patients studied had negative blood culture results; 58 cases were included in the Gadv group, and 134 in the Grsv group. The clinical and epidemiological aspects of the Gadv and Grsv groups are compared in Table 1, while Fig. 1 presents the distribution of cases by age range in both groups.
Clinical and epidemiological aspects of the cases in the Gadv and Grsv groups.
| Gadv Present/Analyzed | % | Grsv Present/Analyzed | % | p | |
|---|---|---|---|---|---|
| Demographic data | |||||
| Male gender | 32/58 | 55.2 | 86/134 | 64.2 | 0.239a |
| Mean age±SD | 9.4±5.4 | 7.1±5.5 | 0.009b | ||
| Prodrome | |||||
| Coryza | 34/52 | 65.4 | 116/128 | 90.6 | < 0.001a |
| Signs of conjunctivitis | 7/54 | 13 | 15/129 | 11.6 | 0.800a |
| Diarrhea | 5/53 | 9.4 | 16/130 | 12.3 | 0.580a |
| Signs and symptoms | |||||
| Coughing | 52/55 | 94.5 | 131/133 | 98.5 | 0.150c |
| Tachypnea | 49/54 | 90.7 | 131/132 | 99.2 | 0.008c |
| Other signs of respiratory distress | 49/54 | 90.7 | 130/133 | 97.7 | 0.046c |
| Wheezing | 42/54 | 77.8 | 121/131 | 92.4 | 0.005a |
| Fever | 36/54 | 66.7 | 92/131 | 70.2 | 0.633a |
| Fever ≥ 39°C | 16/42 | 38.1 | 27/117 | 23.1 | 0.060a |
| Most common diagnostic terms | |||||
| Bronchiolitis | 22/58 | 37.9 | 90/134 | 67.2 | < 0.001a |
| Bronchospasm | 21/58 | 36.2 | 33/134 | 24.6 | 0.101a |
| Pneumonia | 21/58 | 36.2 | 32/134 | 23.9 | 0.079a |
| Antecedents | |||||
| Patient with comorbidity | 23/53 | 43.4 | 49/128 | 38.3 | 0.522a |
| Prematurity < 37 weeks | 9/55 | 16.4 | 24/129 | 18.6 | 0.717a |
| Congenital heart disease | 5/54 | 9.3 | 6/131 | 4.6 | 0.303c |
| Bronchopulmonary dysplasia | 2/54 | 3.7 | 6/128 | 4.7 | > 0.999c |
| Family history of atopy | 28/47 | 59.6 | 73/118 | 61.9 | 0.785a |
| Family member with a cough | 28/48 | 58.3 | 81/120 | 67.5 | 0.261a |
| Agglomeration ≥ 5 persons per domicile | 27/52 | 51.9 | 68/123 | 55.3 | 0.683a |
| Passive smoking | 13/48 | 27.1 | 54/124 | 43.5 | 0.047a |
| Day care attendance | 12/51 | 23.5 | 14/126 | 11.1 | 0.035a |
| Severity and clinical evolution | |||||
| Pulse oximetry < 90% at admission | 17/48 | 35.4 | 37/112 | 33 | 0.770a |
| Cyanosis | 7/53 | 13.2 | 20/129 | 15.5 | 0.692a |
| ICU admission | 6/46 | 13 | 16/117 | 13.7 | 0.915a |
| Need for mechanical ventilation | 6/46 | 13 | 16/117 | 13.7 | 0.915a |
| Antibiotic prescription | 30/50 | 60 | 44/124 | 35.5 | 0.003a |
| Median of hospital length of stay | 5 days | 5 days | 0.902d | ||
Gadv, group associated with the exclusive detection of adenovirus among analyzed viruses; Grsv, group associated with exclusive detection of respiratory syncytial virus among analyzed viruses; ICU, intensive care unit; m, months, SD, standard deviation.
Distribution by age range of cases in the groups Gadv (n = 58) and Grsv (n = 134)a.
Gadv, group associated with the exclusive detection of adenovirus, among the studied viruses; Grsv, group associated with the exclusive detection of respiratory syncytial virus among the studied viruses.
a p = 0.040 at the chi-squared test.
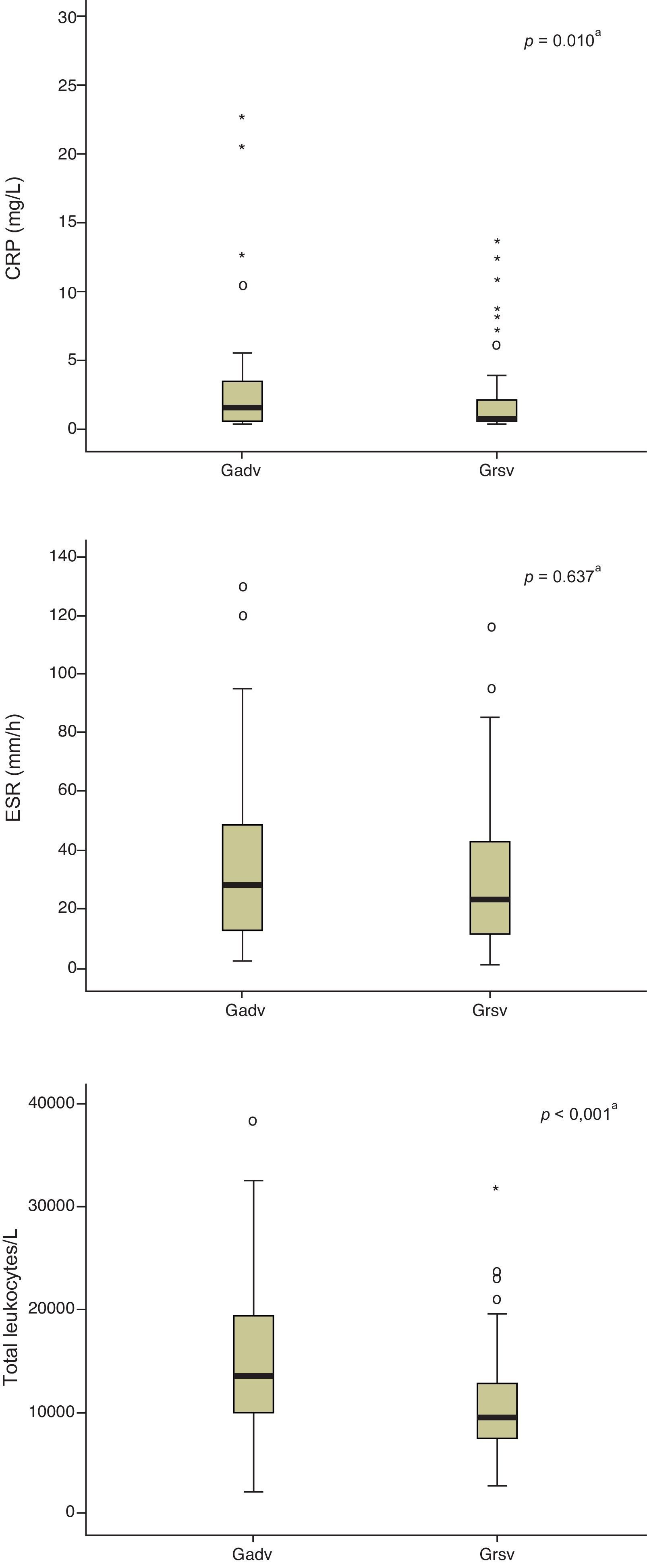
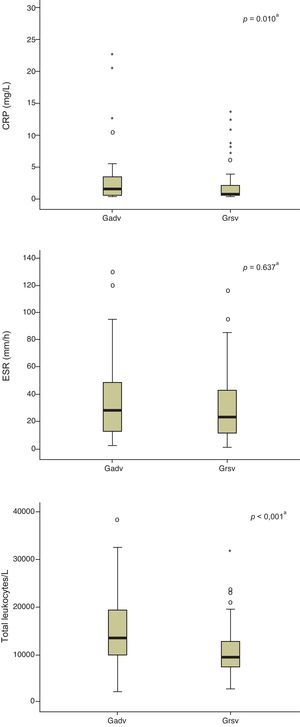
Fig. 2 compares the median values of the inflammatory markers studied in the Gadv and Grsv groups.
Distribution of values of inflammatory markers collected from cases of Gadv and Grsv groups. a Mann-Whitney test. CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; Gadv, group associated with the exclusive detection of adenovirus among the analyzed viruses; Grsv, group associated with the exclusive detection of respiratory syncytial virus among the analyzed viruses.
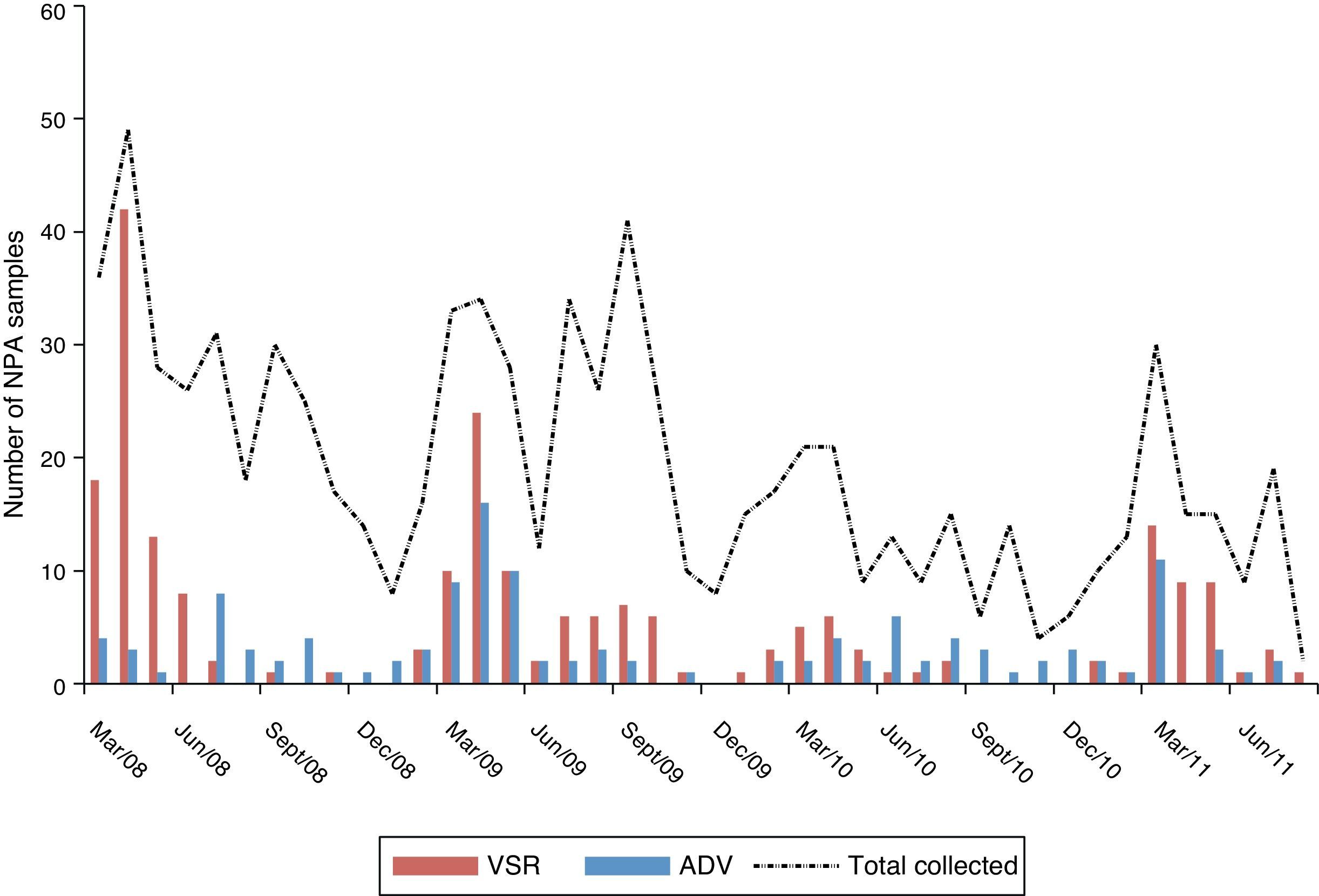
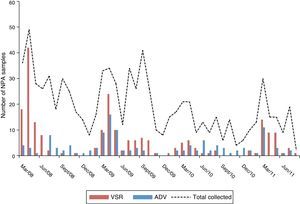
Fig. 3 presents the seasonal distribution of all cases that tested positive at the PCR for ADV or RSV, and the total NPA samples collected.
Monthly distribution of total NPA samples collected for viral testing by PCR and positive samples for adenovirus and respiratory syncytial virus, alone or in co-detections in children hospitalized with suspected acute lower respiratory infection (ALRI) at the Hospital Central da Santa Casa de São Paulo between March of 2008 and August of 2011. ADV, samples positive for adenovirus; ALRI, acute lower respiratory infection; NPA, nasopharyngeal aspirate; PCR, polymerase chain reaction; RSV, samples positive for respiratory syncytial virus.
The positivity of 50.3% for at least one of the eight screened viruses is equivalent to the findings of similar studies, while the high frequency of ADV detection, present in 15.8% of cases, second to RSV, is notable. Recently, a study in Paraguay also recorded a high rate of 18% (9/50) of ADV detection by PCR in NPA samples from children hospitalized with symptoms of severe acute respiratory infection (ARI), with 77.8% of the positive samples obtained from children younger than 2 years.19 Khamis et al.20 who used PCR to study the occurrence of 12 viruses in NPA samples in children younger than 5 years admitted with ARIs, obtained an overall positivity of 51% (130/256), with RSV in 21.9% and ADV in 7.8% of the studied cases.
In São Paulo, Brazil, Thomazelli et al.21 reported an overall positivity rate of 55.6% (187/336), with RSV in 24.1% and ADV in 6.8% of cases investigated by PCR for some of the same eight respiratory viruses analyzed in the present study, but in children up to 5 years of age hospitalized for suspected ARI. The high positivity for ADV observed in the present study could be the result of a convergence of different factors: the large number of hospitalized cases included, perhaps due to a broader range of acceptable diagnoses as inclusion criteria; the younger age group, likely to coincide with a peak incidence of disease associated with ADV;7,8,19 or the exclusive analysis of NPA samples collected in the first 24hours of admission, which contain higher viral titers.
ADV screening test by qualitative PCR is difficult to interpret, as it does not necessarily indicate it as the causative agent of the disease under investigation. Kuypers et al. compared viral positivity rates by IF and real-time PCR (qualitative and quantitative) and observed that most viruses that were not detected by IF, including the ADV, presented low viral loads, probably below the detection level of the IF, a situation more compatible with the persistence/latent states.22
RSV positivity by age range decreased with increasing age of the analyzed cases, in agreement with other studies that showed RSV as the main responsible agent for respiratory infections followed by hospitalization in young infants. Wolf et al.23 observed a decrease in RSV frequency compared to relatively constant rates of ADV during the first two years of life, from the analysis of over 1,000 NPA samples from children with radiological diagnosis of pneumonia. Khamis et al.20 also found a higher predisposition for RSV to affect younger individuals compared to other viruses, including ADV, noting the occurrence of RSV only in those younger than 2 years in their cohort that included children up to 5 years of age. Thomazelli et al.21 observed median ages of patients in whom ADV and RSV were detected very close to those found in the present study, 7 months and 4 months, respectively.
Regarding the antecedents, the influence of age could justify the differences between the groups analyzed concerning environmental hygiene conditions. The Grsv group comprised younger children, who possibly did not attend daycare due to their younger age, and who would suffer more from exposure to cigarette smoke, due to immunological and respiratory system immaturity, increasing the chance of hospitalizations.
Tachypnea, other signs of respiratory distress (difficulty breathing characterized by persistent retractions of the chest wall and/or sternal notch and/or use of accessory respiratory muscles in a calm child), and wheezing were more frequent among patients in the Grsv group, which had a younger mean age than the Gadv group. RSV traditionally causes lower airway pathology in young infants, more prone to respiratory failure, also due to the small airway diameter and greater compliance of the chest wall, which favor collapsed lung and bronchial obstruction.24 The same rationale can explain the higher frequency of admission diagnosis of bronchiolitis among cases from the Grsv group (67.2%), as verified by other similar studies, such as that by Khamis et al.20 (57%) and that by Thomazelli et al.(54%).21
A fever > 39°C occurred in 38.1% of cases in the Gadv group, while Tabain et al.25 reported a frequency of 85.7% among 135 children (71.1% below 2 years) hospitalized with ARIs associated with ADV isolation in cell cultures. It is worth mentioning that less sensitive techniques, such as cultures, are able to detect ADV only from a higher viral load and possibly in a more symptomatic status.
Coryza, a classic prodrome in viral bronchiolitis, showed higher occurrence in the Grsv group, while other studied prodromes had similar frequencies in both groups. A recent Peruvian publication, which analyzed clinical and epidemiological aspects associated with 656 cases with ADV detection by cell culture from over 20,000 samples of respiratory secretions from patients of all ages (median of 3 years) with several respiratory infections, did not verify a higher frequency of cases of conjunctivitis in cases exclusively positive for ADV when compared to other studied viruses.26
In agreement with the observed association between ADV detection and prescription of antibiotics (60%), Tabain et al.25 reported administration of antimicrobials to 76% (101/133) of the studied cases, a proportion as high as the 72% (139/193) observed in the study by Alharbi et al.27 Again, both studies were based on less sensitive diagnostic methods and, therefore, were possibly associated with higher viral loads.
Hospitalization time, with a median of five days for Gadv group cases, was similar to that observed by Alharbi et al.27 in their study of ALRIs associated with ADVs detected by cell culture in children aged up to 4 years, with no statistically significant difference between the Gadv and Grsv groups. The mortality rate of 3.4% in the Gadv group was compatible with the range described by another major study, conducted in Argentina, which was based on 916/48,544 NPA samples found to be positive for ADV by IF (1.1% to 5.3%, depending on the serotype) from children hospitalized for ALRI.28
According to Peltola et al.,29 the median values of total leukocyte count and C-reative protein (CRP) in invasive bacterial infections are higher than those related to viral infections, having a distinct pattern of increase of these inflammatory markers in children with ARI associated with ADV. Several studies suggest that ADV infections can mimic a bacterial infection picture, resulting in greater increase in inflammatory markers, such as that by Tabain et al.,25 which observed leukocytosis (> 15.0 × 109/L) in 77%, CRP > 40.0mg/L in 56%, and erythrocyte sedimentation rate (ESR) > 30mm/h in 71% of children with ARI associated to ADV, and that by Ruuskanen et al.,30 which observed CRP > 40mg/L in 38% of children with infection associated with ADV and in only 13% of those associated with RSV. In the present study, higher CRP and total leukocyte median values were observed in the Gadv group, although lower than levels suggestive of bacterial infection, perhaps because, unlike the abovementioned studies, a qualitative molecular technique of viral research was used, which also identifies cases of persistence/latency devoid of immune response.
ADV showed a pattern of epidemic occurrence, but there was no definite seasonality, while the RSV-positive cases were concentrated between the months of March and June of the studied years, as in other studies performed in Brazil.11,21
The main limitation of this study may be related to the fact that it represented a profile of the institution in which it was performed, and thus, to interpret it, it is necessary to include chronic diseases, not to delimit the time of symptom onset, and to consider the absence of multivariate analysis. The real significance of the finding of ADV associated with clinical pictures compatible with ALRIs, which could lead to a review of the indications of the available vaccine, still requires clarification, which will possibly be achieved with the use of modern techniques such as real-time PCR and a larger number cases in future studies.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Ferone EA, Berezin EN, Durigon GS, Finelli C, Felício MC, Storni JG, et al. Clinical and epidemiological aspects related to the detection of adenovirus or respiratory syncytial virus in infants hospitalized for acute lower respiratory tract infection. J Pediatr (Rio J). 2014;90:42–49.
The study was developed at the Department of Pediatrics and Child Care of Irmandade da Santa Casa de Misericórdia de São Paulo.