To assess the feeding profile of Brazilian infants and preschool children aged 6 months to 6 years, based on the qualitative and quantitative analysis of food and nutrient intake.
Data sourceThis review analyzed studies carried out in Brazil that had food survey data on infants and preschool children. The search was limited to publications from the last 10 years included in the LILACS and MEDLINE electronic databases.
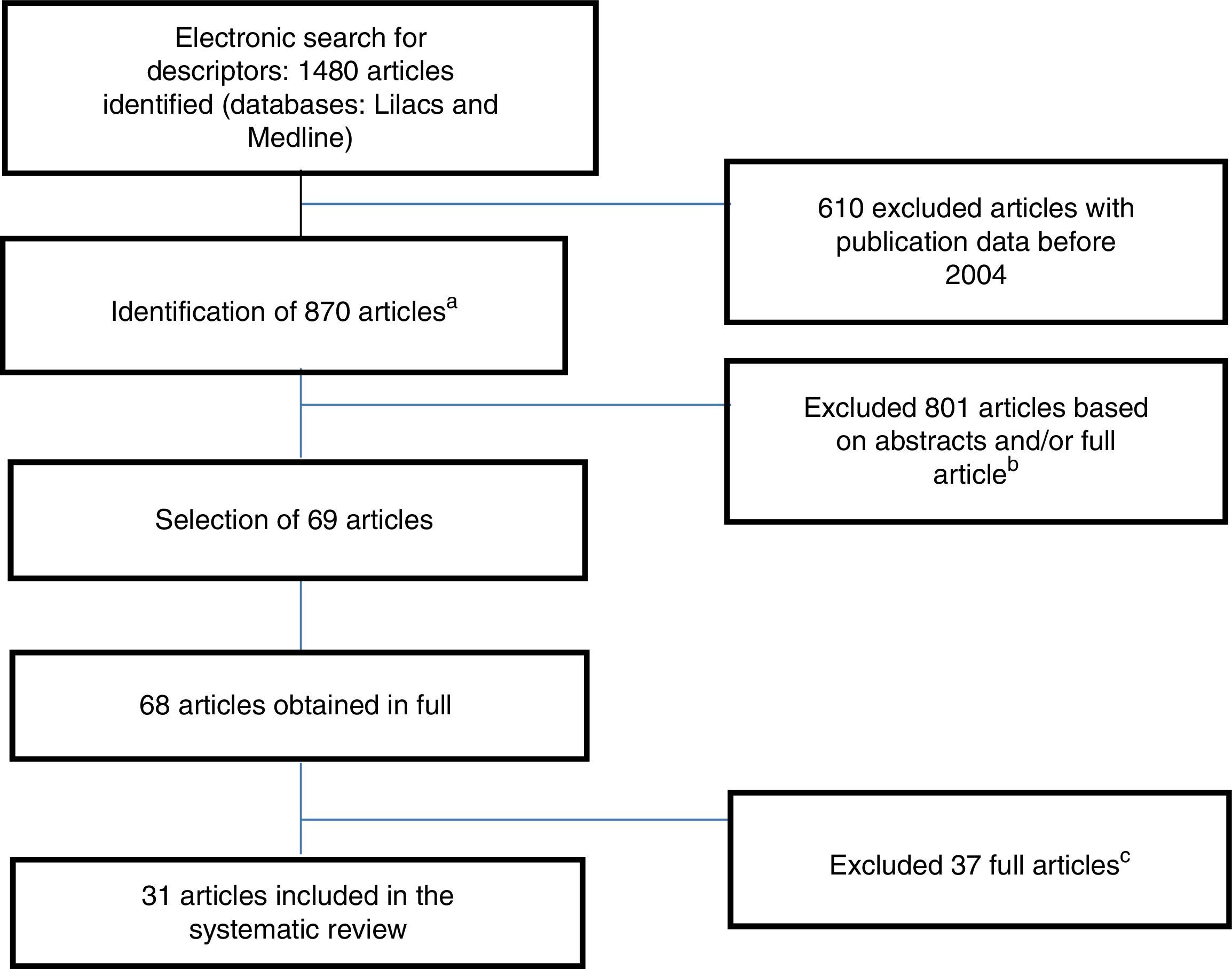
Data summaryThe initial search identified 1480 articles, of which 1411 were excluded after the analysis of abstracts, as they were repeated or did not meet the inclusion criteria. Of the 69 articles assessed in full, 31 articles contained data on food survey and were selected. Only three studies concurrently assessed children from different Brazilian geographical regions. Of the assessed articles, eight had qualitative data, with descriptive analysis of food consumption frequency, and 23 had predominantly quantitative data, with information on energy and nutrient consumption.
ConclusionsThe articles assessed in this review showed very heterogeneous results, making it difficult to compare findings. Overall, the feeding of infants and preschool children is characterized by low consumption of meat, fruits, and vegetables; high consumption of cow's milk and inadequate preparation of bottles; as well as early and high intake of fried foods, candies/sweets, soft drinks, and salt. These results provide aid for the development of strategies that aim to achieve better quality feeding of Brazilian infants and preschoolers.
Verificar o perfil alimentar do lactente e do pré-escolar brasileiro, na faixa etária de 6 meses aos 6 anos, a partir da análise qualitativa e quantitativa do consumo de alimentos e nutrientes.
Fontes de dadosNesta revisão foram analisados estudos realizados no Brasil que apresentavam dados de inquéritos alimentares de lactentes e pré-escolares. A busca foi limitada às publicações dos últimos 10 anos, incluídas nas bases de dados eletrônicas Lilacs e Medline.
Síntese dos dadosNa pesquisa inicial foram identificados 1480 artigos, 1411 foram excluídos após análise dos resumos, por serem repetidos ou não preencherem os critérios de inclusão. Dos 69 artigos avaliados na íntegra, foram selecionados 31 artigos que continham dados sobre alimentação. Apenas 3 trabalhos avaliaram concomitantemente crianças de diferentes regiões geográficas brasileiras. Dos artigos analisados, 8 apresentavam informações qualitativas, com análise descritiva da frequência de consumo alimentar e 23, informações predominantemente quantitativas, com dados de consumo energético e de nutrientes.
ConclusõesOs artigos analisados na presente revisão apresentaram resultados bastante heterogêneos, dificultando a comparação dos achados. De um modo geral, a alimentação do lactente e do pré-escolar é caracterizada pelo baixo consumo de carnes, frutas, legumes e verduras, por elevado consumo de leite de vaca e inadequação no preparo de mamadeiras, além de precoce e elevado consumo de frituras, doces, refrigerantes e sal. Nossos resultados constituem subsídios para a elaboração de estratégias que visem melhor a qualidade da alimentação do lactente e do pré-escolar brasileiro.
Growth and development are two complex, interrelated phenomena that are characteristic of pediatric patients. Growth depends on the interaction of genetic factors, which have their expression modulated by environmental, socioeconomic, emotional, and nutritional factors.1 Therefore, feeding is important not only to provide full growth and development, but also because it is involved in the genesis of the main nutritional disorders in childhood, such as protein–energy malnutrition, obesity, iron deficiency, and hypovitaminosis A.
One aspect that has received increasing attention in recent decades is the association between feeding and nutritional status in early life and the development of chronic diseases in adulthood.2–5 In this context, a systematic review6 showed that long-term breastfeeding is associated with lower values of blood pressure, total cholesterol, prevalence of overweight, and type 2 diabetes mellitus, as well as better intellectual development.
Based on cross-sectional studies carried out in Brazil in the 1970s, 1980s, and 1990s, a rapid decrease was observed in the prevalence of protein–energy malnutrition, as well as an increased prevalence of overweight and obesity, characterizing the nutritional transition phenomenon.5,7 The observed changes have particular characteristics according to geographical regions of Brazil and social classes, and are the result of profound changes in the country over recent decades.7 It should be noted that nutritional transition is a worldwide phenomenon. Across the world, the availability of food has increased by 10%, with a consequent reduction in the prevalence of malnutrition and increasing obesity, which has become a severe concern in terms of public health. It is considered that this phenomenon can be explained, at least in part, by the influence of economic growth, urbanization, and globalization of the dietary pattern.8
Despite the importance of the dietary pattern of infants and preschool children, there are no nationwide data to address this issue in Brazil, with the exception of the National Survey on Women's and Children's Health (Pesquisa Nacional de Demografia e Saúde da Criança e da Mulher [PNDS]),9 with the last survey performed in 2006.
It should be noted that the PNDS data are primarily qualitative, and are related to breastfeeding and complementary feeding.
As it is necessary to explore further scientific production in addition to the PNDS9 regarding dietary patterns in childhood, this article sought to gather not only current information on the feeding quality of Brazilian infants and preschool children, but also to highlight the main inadequacies related to nutrient intake in this population. Considering that there is some concern about the influence of nutritional inadequacies occurring from pregnancy to preschool age in the occurrence of long-term noncommunicable diseases and illnesses, as well as the high prevalence in Brazil of deficiency diseases in childhood, this review aimed to analyze studies on the feeding pattern of infants and Brazilian preschool children, between 6 months and 6 years of age, analyzing qualitative and quantitative information about the consumption of major food and nutrients groups.
MethodsFor inclusion in this review, studies carried out in Brazil were selected through a search of the LILACS and MEDLINE electronic databases. The search was carried out considering four groups of keywords: 1: (“feeding” OR “food consumption” OR “diet”) [Subject descriptor] AND (“child” OR “infant” OR “preschooler”) [Limits] AND Brazil [Words]; 2: (“feeding patterns” OR “feeding behavior” OR “feeding habits”) [Subject descriptor] AND (“child” OR “infant” OR “preschooler”) [Limits] AND Brazil [Words]; 3: (“child feeding” OR “complementary feeding” OR “child nutrition” OR “child nutrition” OR “food supplementation” OR “mixed feeding”) [Subject descriptor] AND (“child” OR “infant” OR “preschooler”) [Limits] AND Brazil [Words]; 4: (“nutritional status” OR “nutritional surveys” [Subject descriptor] AND (“child” OR “infant” OR “preschooler”) [Limits] AND “Brazil” [Words].
The aim of this strategy was to identify all the articles that had data on feeding (from complementary foods consumed after 6 months, to the foods consumed by older children up to the age of 6 years). Data on breastfeeding were not included in the analysis.
There was no restriction on language; however, only original articles were selected, carried out with Brazilian children. Considering the magnitude of the initial results, the search was limited to scientific articles published in the last ten years, with the last search carried out in March 2014. As the inclusion criteria, the authors selected articles carried out with children under the age of 7 years with food survey data (24-h recall, daily usual food, food record, food frequency, and/or direct weighing of food).
At the first analysis, repeated abstracts were excluded, those which coexisted in both databases. Later, two reviewers (MBM, CSM) independently selected abstracts based on the predefined eligibility criteria. For abstracts that did not contain enough information to be included in the literature review, it was decided to evaluate the full text. Cases of disagreement regarding the selection were reevaluated until a consensus was achieved.
Fig. 1 describes the flowchart of the research, selection, and inclusion of scientific articles in the literature review. A standardized assessment was carried out of the following information of the assessed articles: study location, year of data collection, type of study and sampling, methods used to evaluate the feeding, and summary of the main results.
Flowchart of the research, selection, and inclusion of scientific articles in the systematic review.
a Studies published in the last 10 years (since 2004).
b Repeated articles (64)/did not meet the inclusion criteria (1347).
c After reading the full article, it had no data on food survey or had data on children older than 7 years (37).
Using the initial search strategy with keywords, 1480 articles were identified in the databases. After the exclusion of repeated articles and the analysis based on the predefined inclusion criteria, 31 articles were eligible.
Analyzing the studies included in this literature review, an important heterogeneity was verified in the studies about the specific objectives, sample composition, methods used to evaluate the feeding (surveys), and expression of results, which prevented the comparison of different findings. Therefore, a descriptive analysis of the results shown in the reviewed articles was performed, aiming to aggregate the original information obtained from the different studies.
Only three articles assessed children from different geographical regions: (1) a study with 4322 children, carried out based on PNDS/2006 data10; (2) a study with 3058 children living in nine Brazilian cities11; and (3), a study with children from three cities: Recife, São Paulo, and Curitiba.12 The other articles (n=28) were carried out as follows: four in the North, nine in the Northeast, ten in the Southeast, and five in the South region. It should be noted that three studies in the Northeast carried out in Pernambuco13–15 and three from the South region in São Leopoldo16–18 addressed different results from the same population survey.
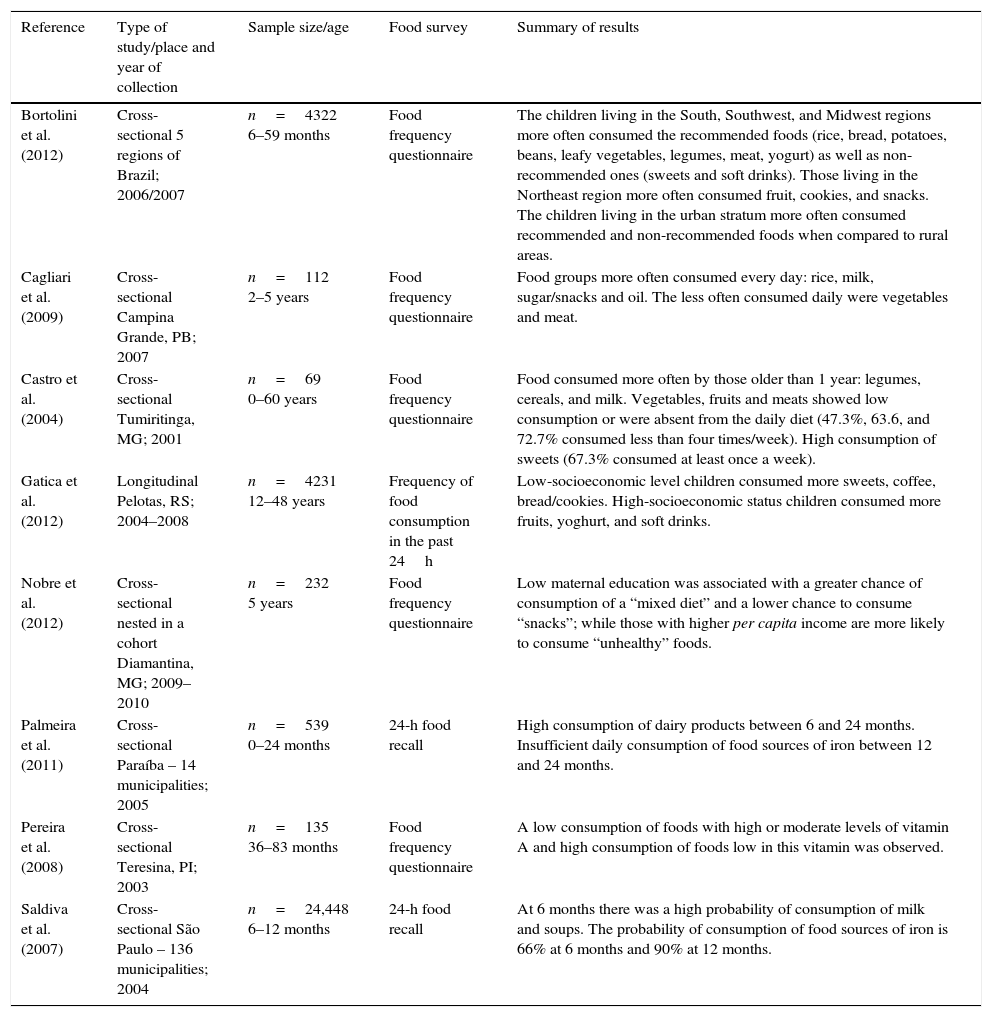
The articles were divided into two categories: those with mainly qualitative information and those with quantitative information. The articles were characterized as qualitative when they had only descriptive data on the frequency of consumption of specific foods or food groups. The quantitative articles were those with information related to energy and/or nutrient consumption. Tables 1 and 2 disclose the basic information on the eight qualitative and 23 quantitative studies, respectively.
Type of study, place and year of implementation, sample size, age, and method used for qualitative assessment of dietary intake of eight studies with Brazilian infants and preschool children.
| Reference | Type of study/place and year of collection | Sample size/age | Food survey | Summary of results |
|---|---|---|---|---|
| Bortolini et al. (2012) | Cross-sectional 5 regions of Brazil; 2006/2007 | n=4322 6–59 months | Food frequency questionnaire | The children living in the South, Southwest, and Midwest regions more often consumed the recommended foods (rice, bread, potatoes, beans, leafy vegetables, legumes, meat, yogurt) as well as non-recommended ones (sweets and soft drinks). Those living in the Northeast region more often consumed fruit, cookies, and snacks. The children living in the urban stratum more often consumed recommended and non-recommended foods when compared to rural areas. |
| Cagliari et al. (2009) | Cross-sectional Campina Grande, PB; 2007 | n=112 2–5 years | Food frequency questionnaire | Food groups more often consumed every day: rice, milk, sugar/snacks and oil. The less often consumed daily were vegetables and meat. |
| Castro et al. (2004) | Cross-sectional Tumiritinga, MG; 2001 | n=69 0–60 years | Food frequency questionnaire | Food consumed more often by those older than 1 year: legumes, cereals, and milk. Vegetables, fruits and meats showed low consumption or were absent from the daily diet (47.3%, 63.6, and 72.7% consumed less than four times/week). High consumption of sweets (67.3% consumed at least once a week). |
| Gatica et al. (2012) | Longitudinal Pelotas, RS; 2004–2008 | n=4231 12–48 years | Frequency of food consumption in the past 24h | Low-socioeconomic level children consumed more sweets, coffee, bread/cookies. High-socioeconomic status children consumed more fruits, yoghurt, and soft drinks. |
| Nobre et al. (2012) | Cross-sectional nested in a cohort Diamantina, MG; 2009–2010 | n=232 5 years | Food frequency questionnaire | Low maternal education was associated with a greater chance of consumption of a “mixed diet” and a lower chance to consume “snacks”; while those with higher per capita income are more likely to consume “unhealthy” foods. |
| Palmeira et al. (2011) | Cross-sectional Paraíba – 14 municipalities; 2005 | n=539 0–24 months | 24-h food recall | High consumption of dairy products between 6 and 24 months. Insufficient daily consumption of food sources of iron between 12 and 24 months. |
| Pereira et al. (2008) | Cross-sectional Teresina, PI; 2003 | n=135 36–83 months | Food frequency questionnaire | A low consumption of foods with high or moderate levels of vitamin A and high consumption of foods low in this vitamin was observed. |
| Saldiva et al. (2007) | Cross-sectional São Paulo – 136 municipalities; 2004 | n=24,448 6–12 months | 24-h food recall | At 6 months there was a high probability of consumption of milk and soups. The probability of consumption of food sources of iron is 66% at 6 months and 90% at 12 months. |
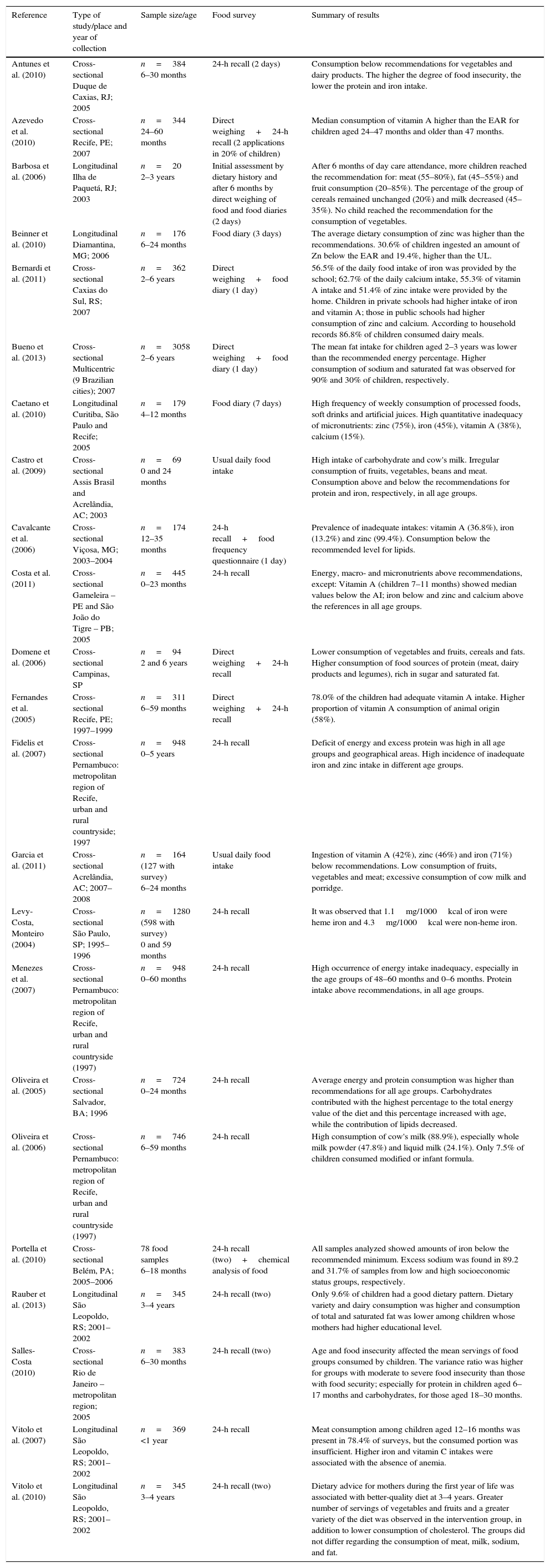
Type of study, place and year of study, sample size, age and method for qualitative and quantitative assessment of dietary consumption of 23 studies with Brazilian infants and preschoolers.
| Reference | Type of study/place and year of collection | Sample size/age | Food survey | Summary of results |
|---|---|---|---|---|
| Antunes et al. (2010) | Cross-sectional Duque de Caxias, RJ; 2005 | n=384 6–30 months | 24-h recall (2 days) | Consumption below recommendations for vegetables and dairy products. The higher the degree of food insecurity, the lower the protein and iron intake. |
| Azevedo et al. (2010) | Cross-sectional Recife, PE; 2007 | n=344 24–60 months | Direct weighing+24-h recall (2 applications in 20% of children) | Median consumption of vitamin A higher than the EAR for children aged 24–47 months and older than 47 months. |
| Barbosa et al. (2006) | Longitudinal Ilha de Paquetá, RJ; 2003 | n=20 2–3 years | Initial assessment by dietary history and after 6 months by direct weighing of food and food diaries (2 days) | After 6 months of day care attendance, more children reached the recommendation for: meat (55–80%), fat (45–55%) and fruit consumption (20–85%). The percentage of the group of cereals remained unchanged (20%) and milk decreased (45–35%). No child reached the recommendation for the consumption of vegetables. |
| Beinner et al. (2010) | Longitudinal Diamantina, MG; 2006 | n=176 6–24 months | Food diary (3 days) | The average dietary consumption of zinc was higher than the recommendations. 30.6% of children ingested an amount of Zn below the EAR and 19.4%, higher than the UL. |
| Bernardi et al. (2011) | Cross-sectional Caxias do Sul, RS; 2007 | n=362 2–6 years | Direct weighing+food diary (1 day) | 56.5% of the daily food intake of iron was provided by the school; 62.7% of the daily calcium intake, 55.3% of vitamin A intake and 51.4% of zinc intake were provided by the home. Children in private schools had higher intake of iron and vitamin A; those in public schools had higher consumption of zinc and calcium. According to household records 86.8% of children consumed dairy meals. |
| Bueno et al. (2013) | Cross-sectional Multicentric (9 Brazilian cities); 2007 | n=3058 2–6 years | Direct weighing+food diary (1 day) | The mean fat intake for children aged 2–3 years was lower than the recommended energy percentage. Higher consumption of sodium and saturated fat was observed for 90% and 30% of children, respectively. |
| Caetano et al. (2010) | Longitudinal Curitiba, São Paulo and Recife; 2005 | n=179 4–12 months | Food diary (7 days) | High frequency of weekly consumption of processed foods, soft drinks and artificial juices. High quantitative inadequacy of micronutrients: zinc (75%), iron (45%), vitamin A (38%), calcium (15%). |
| Castro et al. (2009) | Cross-sectional Assis Brasil and Acrelândia, AC; 2003 | n=69 0 and 24 months | Usual daily food intake | High intake of carbohydrate and cow's milk. Irregular consumption of fruits, vegetables, beans and meat. Consumption above and below the recommendations for protein and iron, respectively, in all age groups. |
| Cavalcante et al. (2006) | Cross-sectional Viçosa, MG; 2003–2004 | n=174 12–35 months | 24-h recall+food frequency questionnaire (1 day) | Prevalence of inadequate intakes: vitamin A (36.8%), iron (13.2%) and zinc (99.4%). Consumption below the recommended level for lipids. |
| Costa et al. (2011) | Cross-sectional Gameleira – PE and São João do Tigre – PB; 2005 | n=445 0–23 months | 24-h recall | Energy, macro- and micronutrients above recommendations, except: Vitamin A (children 7–11 months) showed median values below the AI; iron below and zinc and calcium above the references in all age groups. |
| Domene et al. (2006) | Cross-sectional Campinas, SP | n=94 2 and 6 years | Direct weighing+24-h recall | Lower consumption of vegetables and fruits, cereals and fats. Higher consumption of food sources of protein (meat, dairy products and legumes), rich in sugar and saturated fat. |
| Fernandes et al. (2005) | Cross-sectional Recife, PE; 1997–1999 | n=311 6–59 months | Direct weighing+24-h recall | 78.0% of the children had adequate vitamin A intake. Higher proportion of vitamin A consumption of animal origin (58%). |
| Fidelis et al. (2007) | Cross-sectional Pernambuco: metropolitan region of Recife, urban and rural countryside; 1997 | n=948 0–5 years | 24-h recall | Deficit of energy and excess protein was high in all age groups and geographical areas. High incidence of inadequate iron and zinc intake in different age groups. |
| Garcia et al. (2011) | Cross-sectional Acrelândia, AC; 2007–2008 | n=164 (127 with survey) 6–24 months | Usual daily food intake | Ingestion of vitamin A (42%), zinc (46%) and iron (71%) below recommendations. Low consumption of fruits, vegetables and meat; excessive consumption of cow milk and porridge. |
| Levy-Costa, Monteiro (2004) | Cross-sectional São Paulo, SP; 1995–1996 | n=1280 (598 with survey) 0 and 59 months | 24-h recall | It was observed that 1.1mg/1000kcal of iron were heme iron and 4.3mg/1000kcal were non-heme iron. |
| Menezes et al. (2007) | Cross-sectional Pernambuco: metropolitan region of Recife, urban and rural countryside (1997) | n=948 0–60 months | 24-h recall | High occurrence of energy intake inadequacy, especially in the age groups of 48–60 months and 0–6 months. Protein intake above recommendations, in all age groups. |
| Oliveira et al. (2005) | Cross-sectional Salvador, BA; 1996 | n=724 0–24 months | 24-h recall | Average energy and protein consumption was higher than recommendations for all age groups. Carbohydrates contributed with the highest percentage to the total energy value of the diet and this percentage increased with age, while the contribution of lipids decreased. |
| Oliveira et al. (2006) | Cross-sectional Pernambuco: metropolitan region of Recife, urban and rural countryside (1997) | n=746 6–59 months | 24-h recall | High consumption of cow's milk (88.9%), especially whole milk powder (47.8%) and liquid milk (24.1%). Only 7.5% of children consumed modified or infant formula. |
| Portella et al. (2010) | Cross-sectional Belém, PA; 2005–2006 | 78 food samples 6–18 months | 24-h recall (two)+chemical analysis of food | All samples analyzed showed amounts of iron below the recommended minimum. Excess sodium was found in 89.2 and 31.7% of samples from low and high socioeconomic status groups, respectively. |
| Rauber et al. (2013) | Longitudinal São Leopoldo, RS; 2001–2002 | n=345 3–4 years | 24-h recall (two) | Only 9.6% of children had a good dietary pattern. Dietary variety and dairy consumption was higher and consumption of total and saturated fat was lower among children whose mothers had higher educational level. |
| Salles-Costa (2010) | Cross-sectional Rio de Janeiro – metropolitan region; 2005 | n=383 6–30 months | 24-h recall (two) | Age and food insecurity affected the mean servings of food groups consumed by children. The variance ratio was higher for groups with moderate to severe food insecurity than those with food security; especially for protein in children aged 6–17 months and carbohydrates, for those aged 18–30 months. |
| Vitolo et al. (2007) | Longitudinal São Leopoldo, RS; 2001–2002 | n=369 <1 year | 24-h recall | Meat consumption among children aged 12–16 months was present in 78.4% of surveys, but the consumed portion was insufficient. Higher iron and vitamin C intakes were associated with the absence of anemia. |
| Vitolo et al. (2010) | Longitudinal São Leopoldo, RS; 2001–2002 | n=345 3–4 years | 24-h recall (two) | Dietary advice for mothers during the first year of life was associated with better-quality diet at 3–4 years. Greater number of servings of vegetables and fruits and a greater variety of the diet was observed in the intervention group, in addition to lower consumption of cholesterol. The groups did not differ regarding the consumption of meat, milk, sodium, and fat. |
EAR, Estimated Average Requirement; UL, Upper Tolerable Intake Level; AI, Adequate Intake.
It should be noted that a significant portion of the collected articles did not assess probabilistic samples that adequately represented the entire Brazilian population of the assessed age group. Therefore, the analyzed data cannot be extrapolated to the entire Brazilian population of infants and preschoolers. In turn, the information obtained represents the only currently available data and should be used with caution, until studies whose sampling takes into account all the peculiar characteristics of Brazil (e.g., urban and rural settings, different weather conditions, socioeconomic status, cultural and regional differences, among others) are carried out.
The following are critical comments integrating the results of different surveys according to the different categories of food and nutrient groups.
Consumption of cow's milk and dairy productsIn general, it can be stated that cow's milk is one of the most commonly consumed foods by Brazilian children. Whole milk was consumed daily on average by 76.9% of the children, considering different studies that included children aged between 1 and 7 years.19–21 In the state of Paraíba, it was found that 85.9% of children aged 6–12 months consumed dairy foods daily.22 Regarding the consumption of infant formula, one study found that only 6.7% of children older than 6 months received formula as a substitution for breast milk.10
Regarding the number of daily recommended servings of dairy foods, it was observed in Duque de Caxias, in Rio de Janeiro,23 that children aged 6–30 months had an average consumption of two servings/day, which is considered below the three servings recommended by national guidelines on food and nutrition.24 Meanwhile, in a small group of children aged 2–3 years from Paquetá Island (RJ), the average consumption was even smaller, 1.8 servings/day, also below the recommendation when considering the US dietary guidelines as reference,25 which recommend two servings/day. As for the per capita daily consumption of cow's milk and dairy products, according to data obtained in Salvador (BA), children aged 6–12 months consumed an average of 528.9mL/day and children aged 12–24 months, 548.1mL/day.26
In a study conducted with children aged between 4 and 12 months, living in three Brazilian cities (Curitiba, Sao Paulo, and Recife),12 the mean age for introduction of formula was three months, whereas the mean age for the introduction of complementary feeding and family foods was 4 months and 5.5 months, respectively.
According to worldwide guidelines, the continuation of breastfeeding should be encouraged as the exclusive source of dairy foods milk up to 2 years of age or older, and the introduction of whole cow's milk should be contraindicated before 12 months of life.27 It is already well established that early and/or excessive consumption of cow's milk may be related to the occurrence of iron deficiency anemia, food allergy, and obesity.27,28 Infant formulas, despite having intact proteins, are the first choice of diary feeding for weaned children, mainly due to the adequacy of protein and micronutrient requirements for infants.27
Consumption of meatRegarding the frequency of weekly consumption, the PNDS/2006 assessed 4322 children from five Brazilian regions, ages 6–59 months, and found that 24.6% consumed beef daily, 6.1% consumed chicken, and 1.5% consumed fish; i.e., the daily consumption of some type of meat was verified in only 32.2% of the assessed children.10 In São Paulo state,29 it was found that the probability children aged 6 months would consume meat in soups or cooked meals was 54% and 25%, respectively, showing a trend of increasing consumption close to 12 months of age. The consumption of some kind of meat in the last 24h, for children aged 6–12 months, occurred on average in approximately 35% of children, according to data from different studies,26,29 and on average in 47.3% of children aged 12–24 months.22,26
Regarding the consumption of daily servings, it was observed in São Leopoldo (RS)18 that 78.4% of children ate meat, but in insufficient quantities. In Campinas (SP),30 in children aged 2–6 years, a consumption of 1.32 servings/day from the meat food group was observed, with no difference between the male and female genders. Both national and international guidelines recommend the consumption of two servings per day from the meat food group.24,25
In Salvador (BA),26 an average per capita consumption of meat of 13.3g/day was observed in children aged 6 and 12 months, and 24.4g/day in children aged 12–24 months. Regarding the daily energy equivalent, a study in Acre31 observed that the meat food group (beef, chicken, and fish) contributed 3% of the total energy intake of children aged 6–11 months and 5% in children aged 12–24 months.
Meats comprise the food group that constitutes a source of iron with high bioavailability, and in addition to being a source of heme iron, it potentiates the absorption of non-heme iron. One should be aware of the difficulty in accepting meat by infants and preschool children, especially in relation to the consistency of the offered food. Another factor that confirms the deficient intake is the cost of food. Providing nutritional education can promote the appropriate qualitative and quantitative consumption of this food group, representing an essential strategy for the prevention of iron-deficiency anemia.32
Consumption of fruits and vegetablesAlthough some authors29 reported high rates of consumption of fruit (87%) by children aged 6–12 months in the last 24h, in an assessment of weekly frequency of consumption, the daily consumption of fruit and natural fruit juice, respectively, was confirmed by 44.6% and 32.5% of the children in different regions of Brazil.10 It was also observed that 11.6% of infants and preschool children did not consume fruits throughout the entire week, and that fruit consumption was more common in the South, Northeast, and Southeast regions of the country.10
The average per capita consumption of fruit, according to a study carried out in Salvador, was 183.1g/day for children aged between 6 and 12 months, and 223.1g/day for children aged 12–24 months. Oranges and bananas were the fruit most often consumed by children in both age groups.26
The group of vegetables was referred to as irregularly or little consumed by several authors in studies with infants and preschool children.16,19,23,30,33–37 In Acre, it was found that 53.4% of children aged 6–24 months did not consume any vegetables in their main meals.37
Regarding the weekly frequency of consumption, vegetables and green vegetables were the least eaten daily by children from daycare centers in Campina Grande (PB) (36% of those who stayed at school full time and 21% of those who stayed part time). Most children fit a pattern of consumption of between one to four times per week.19
The number of daily servings did not reach the recommendation of three servings per day24,25 for the children attending a philanthropic daycare center.33 For children aged between 6 and 12 months, the average per capita consumption of vegetables was 57g/day, and potatoes, carrots, pumpkin, and chayote were the vegetables most often consumed.26 There was also a lower per capita intake (45.7g/day) of this food group in children aged 6–12 months.26 Children from the South, Southeast and Midwest regions showed higher consumption of vegetables according to data from PNDS/2006.10
Nationwide studies9,38,39 have found that the consumption of fruits and vegetables is not sufficient for the majority of the population in all age groups. It is worth mentioning that these food groups constitute one of the main daily sources of vitamins, minerals, and dietary fibers.
Consumption of cereals and legumesConsidering the consumption of cereals in the form of flour to prepare porridge, it was found in Salvador (BA)26 that corn-based products were consumed by 42.5% of children aged between 6 and 12 months and 41% of children between 12 and 24 months old.
In Diamantina (MG),34 children aged 6–24 months had their diet characterized as showing poor quality and diversity. Rice, beans, and cornmeal were the main foods prepared by their mothers or guardians.34 Practically all assessed preschoolers in Campina Grande (PB) consumed rice daily, while the daily intake of beans was observed in 71% of the children.19 In a rural settlement in Minas Gerais, it was found that in children aged more than 1 year, cereals and legumes, more precisely, rice (92.7%) and beans (94.7%), were the most frequently consumed foods, considering that consumption occurred four to seven times per week.20
Regarding the consumption pattern, it was found that the average daily consumption of cereal and cereal products (rice, biscuits, bread, and pasta), for children aged between 6 and 12 months, amounted to 28g/day; for beans, it was 14g/day. Children aged 12–24 months had an average per capita consumption of cereals and legumes of 82g/day and 40g/day, respectively.26
In the PNDS/2006, a nationwide study,10 the daily consumption of rice and/or pasta was reported for 77.4% of children aged 6–59 months, bread for 52%, and beans/lentils for 66%. Rice and bread were the most often consumed foods by children living in the Midwest, Southeast, and South regions. Regarding the frequent consumption of beans, the highest frequency occurred in the Midwest and Southeast regions. Children from the North and Northeast regions had a lower daily frequency of consumption of both cereals (rice, pasta, and bread), and legumes (beans and lentils) compared to children from other Brazilian regions.10
The daily consumption of cereals and legumes is indicated in childhood, starting from the period of introduction of complementary foods at 6 months of life. These foods are sources of B vitamins, non-heme iron, and zinc, among other vitamins and minerals, and together they constitute an excellent source of protein.27,28
Consumption of oils and fatsIt was shown, considering the data of 4322 children from the five regions of Brazil (data from PNDS/2006), that 51% of them consumed fried foods at least once a week; a higher rate of consumption, ranging from one to three times per week, was found in children from the South and Southeast regions of Brazil.10
The group of oils had a high frequency of daily consumption in a study of preschool children in Campina Grande, and were consumed by 76% of children who remained full-time and 90% who remained part-time in day care centers.19
In Salvador (BA), it was found that the consumption of oil and margarine was low for children aged 6–12 months and 12–24 months, with an average daily intake of 0.7g/day and 0.6g/day, respectively.26
It is noteworthy that in dietary studies, the consumption of fats and oils, as well as salt, may frequently be under- or overestimated, due to lack of proper identification of the amount used in the preparation of foods.30 The consumption of fried foods, excess of salt, and added sugar are contraindicated in children's diet.24
Consumption of sugar, sweets, and sugary drinksSugars and sweets is a group that shows a high frequency of consumption by the pediatric population, as verified by several authors.10,12,19,26,30,31,40 In Curitiba, São Paulo, and Recife,12 it was found that during the preparation of baby bottles for infants aged between 6 and 12 months, sugar, cereals, chocolate milk, or both were added to 90.4% of them when prepared with powdered cow's milk.12 This addition occurred in the preparation of 54.7% of the infant formulas.
One study showed that the daily consumption of sweets and also soft drinks occurred in approximately 22% of children. Consumption of sweets and soft drinks at least once a week was verified for more than 70% of children. Higher frequency of daily consumption of sweets and soft drinks was found in children from the South and Southeast regions.10
The average daily consumption of sugar was 23g/day for children aged 6–12 and 37g/day for children aged 12–24 months in a study carried out in Salvador.26 In Acre,31 it was observed that the consumption of sweets and sugary drinks amounted to 14% of the total energy intake for children aged 6–11 months and to 18% of the total energy, for children aged between 12 and 24 months.
A multicenter study carried out in five Brazilian cities found that the consumption of sugary drinks, including soft drinks and artificial juices, accounted for 37% of the energy derived from liquids that were consumed daily by children aged 3–6 years.39 The excessive consumption of sugary drinks has been associated with the occurrence of overweight in children, favoring the early development of chronic noncommunicable diseases such as diabetes and hypertension. According to current guidelines,41 free sugar intake should be equivalent to less than 10% of the total daily energy value.
Food securityFood insecurity and/or low socioeconomic status was associated with increased consumption of carbohydrates and lower consumption of proteins23,35,42 and iron23,31 in several studies. Foods from the groups of meat and eggs, cereals, fruits, vegetables, and fat showed variations in their consumption, and were usually little consumed by children with some degree of food insecurity.22,23,43
Greater consumption of sweets may be associated with lower family income and lower parental education.19,20,44 High intake of coffee19,23,44 and bread and biscuits19,22,44 can be seen more frequently in those with lower socioeconomic status or food insecurity. There are no recommendations related to coffee consumption; however, it is known that excessive consumption may hinder the absorption of nutrients such as iron.27
Some authors emphasize the importance of institutions in improving the quality of child feeding.33,35,36,45 The guarantee of care in health and nutrition during the period spent in day care centers is favorable for children belonging to lower socioeconomic groups.33
Adequacy of macronutrients and dietary fiberAmong the macronutrients, proteins and lipids showed more frequent inadequacy findings. Protein consumption above the recommendations was observed in studies with children at different age ranges.13,14,26,35,42 Lipid consumption below the recommended was found in a multicenter study,11 in addition to other studies carried out in Belém (PA)42 and in Viçosa (MG).46 However, high intake of saturated fat was observed by some authors,11,16,30 which may characterize the quality of the offered diet and the high intake of dairy foods. The fat intake may be underestimated in some studies due to failure to account for the added fat in food preparation.
A study carried out in nine Brazilian capital cities11 found that dietary fiber intake was higher than the adequate intake of the Dietary Reference Intakes (DRIs)47 in only 22% of children younger than four years and 5% of children older than four years. The average dietary fiber intake ranged from 9.2 to 10g per 1000kcal. Dietary fiber intake in early childhood is scarcely investigated.
Micronutrient adequacyThe evaluation of the micronutrients iron, calcium, zinc, sodium, and vitamin A was considered in this literature review. Calcium and zinc, in general, showed that their requirements were achieved, and even exceeded the recommendations in some studies.11,34,35,48 Iron and vitamin A showed differences regarding the adequacy for different age groups.13,31,37,48 As for sodium intake, consumption higher than the recommended limit was the most frequent result.11,42
Milk and dairy products, which are foods often consumed by the pediatric population, are the main food sources associated with the adequacy of calcium and zinc. However, milk casein, as well as the presence of phytates, reduces the bioavailability of zinc.49 After the sixth month of life, approximately 70% of the iron and zinc requirements of infants should be met through supplementary feeding.12
High frequency of children with calcium intake higher than the recommended amounts was verified in some studies. A study48 with 445 children aged 0–23 months in Pernambuco and Paraiba showed that calcium intake was higher than recommended for all children in the assessed age group. In Caxias do Sul (RS),35 it was observed that approximately 67% of the 362 assessed children, aged 2–6 years, had calcium intake at or above the recommended vale. A multicenter study of preschool children from public and private schools found an average of inadequacy in calcium intake of 13.1% and 44.6% in children younger than 4 years and in children aged ≥4 years, respectively.11
A study13 with children from Pernambuco showed high percentage of vitamin A intake inadequacy for the children aged 1–3 years and 4–5 years living in the metropolitan area and the inadequacy (lower than the Estimated Average Requirement [EAR]) was 27.9% and 43.2%, respectively. Among those living of the urban countryside, the inadequacy in these age groups was 48.9% and 54.3%, respectively. In children belonging to the age group of 7–11 months in the same study, the median vitamin A intake (314μg) was below the Adequate Intake (AI)47 (500μg). Another study, also carried out in Recife (PE), found consumption below the EAR47 for vitamin A in 8.1% of children aged 24–47 months, and 21.3% in those aged 48–60 months, with this lower percentage of inadequacy being attributed to dietary quality in day care.45
It should be taken into account that the bioavailability of vitamin A in animal-source foods is higher when compared to the carotenoids with pro-vitamin A activity.36,45 Fernandes et al.,36 in addition to verifying the adequate intake of vitamin A by 77.9% of children under 5 years, found that approximately 58.0% of the consumption came from animal-source foods (preformed vitamin A) and 35.0% from vegetable foods (carotenoids).
Iron-deficiency anemia and vitamin A deficiency are nutritional deficiencies characterized as a public health problem in Brazil. The deficiency of micronutrients such as vitamin A, iron, and zinc impairs the normal growth and development of children and lowers their resistance to infectious diseases.46 Vitamin A deficiency has some endemic areas in Brazil. According to data from the PNDS/2006,9 inadequate levels of vitamin A (0.70mmol/L) were verified in 17.4% of the assessed children, with the highest prevalence occurring in the Northeast (19.0%) and Southeast (21.6%) of the country. In the same survey, the prevalence of anemia (hemoglobin<11g/dL) was 20.9% in Brazil, with the highest prevalence found in the Northeast (25.5%) and the lowest found in the North (10.4%).
One study analyzed the iron density in the diet of children aged 6–59 months in São Paulo, and found that 1.1mg/1000kcal were from heme iron and 4.3mg/1000kcal were from non-heme iron.50 Animal-source iron contributed 0.6% and 14.3% of total iron ingested by children aged 6–11 months and 12–24 months, respectively.31
In São Leopoldo (RS),18 a study of 369 children aged between 12 and 16 months found that the absence of anemia was significantly associated with higher consumption of heme iron and vitamin C, and with lower intake of calcium.
It was observed that the average cow's milk consumption was statistically lower in children who did not have severe anemia (523±315mL) when compared to those with severe anemia (648±387mL) (p=0.01). That is, the consumption of cow's milk can promote adequate calcium and zinc intake; however, it is related to the inadequacy of iron and may have an inhibitory effect on the absorption of dietary iron,50 favoring the occurrence of iron-deficiency anemia.15
Sodium intake higher than the recommendation was observed on average in 98.1% of the children in a study with preschool children from public and private schools in nine Brazilian cities, with an average daily consumption of 2186.5mg.11 In Belém (PA),42 it was demonstrated through the chemical analysis of food samples prepared at home for lunch that the sodium content was higher in the low socioeconomic (363.2±148.3mg) than in the high socioeconomic group (269.3±138.0; p=0.005). Excess sodium was more frequent in foods of the low socioeconomic group than in foods of the high socioeconomic group (89.2% vs. 31.7%; p=0.027).
Currently, the National Plan of Sodium Reduction in Processed Foods aims to reduce sodium intake among Brazilians, including actions to reduce the addition of salt to manufactured products and awareness regarding rational consumption of added salt. These strategies are part of the process of coping with noncommunicable diseases, such as arterial hypertension and cardiovascular diseases.51 According to data from the Household Budget Survey (2002–2003),52 the addition of salt and salt-based seasonings constituted the main sources of sodium in Brazilian diet. In the 2008–200953 survey, a reduction was observed in the annual per capita consumption of salt; however, there was an increase in the consumption of processed, ready-to-eat foods.
The results of this literature review depict the dietary quality of Brazilian infants and preschoolers in recent years. The dietary pattern and occurrence of nutritional disorders in children remain matters of concern, as demonstrated by studies published in Brazil after the data search to perform this literature review.54–57
From the methodological point of view, this study followed the principles for systematic literature reviews; i.e., the search was organized according to explicit, comprehensive, and reproducible criteria, followed by critical analysis of the relevant gathered information.
ConclusionThe results of the different studies assessed in this literature review allow a broader evaluation of the feeding profile characteristics of Brazilian infants and preschoolers. Despite the heterogeneity of the evaluated articles, one can observe that irrespective of socioeconomic status, region of origin, or age, qualitative and quantitative inadequacies related to the consumption of food and nutrients are similar. Overall, a low frequency of consumption of meat, fruits, and vegetables is observed. The protein adequacy in the diet is guaranteed by the high consumption of cow's milk; however, the ingestion of this nutrient is often excessive. The preparation of baby bottles is inappropriate, considering the addition of unnecessary ingredients to infant formulas. Excessive consumption of fried foods, soft drinks, sweets, candies, and salt is also observed.
The occurrence of inadequacies in nutrient intake may be associated with the perpetuation of the main public health problems found in the pediatric population, such as iron deficiency anemia, vitamin A deficiency, and excess weight associated with the early onset of comorbidities that are highly prevalent in adults, such as diabetes mellitus and systemic arterial hypertension.
Considering that food choices are related not only to purchasing power, but mainly to actions based on the food and nutrition education, it is worth emphasizing the importance of more effective adoption and implementation of health policies aimed at this vulnerable population, in order to promote adequate growth and development as well as to prevent diseases and nutritional disorders. The results assessed in this review represent aids for the development of strategies to improve the dietary quality of Brazilian infants and preschoolers.
Conflicts of interestCSM and MBM participated in the international project by Danone Early Nutrition known as NUTRIPLANET (2013) in Brazil; KVB is part of the team of Danone Early Nutrition in Brazil.
This research was supported by Danone Early Nutrition as an extension of the NUTRIPLANET project in Brazil (2013). The content of this article was based exclusively on scientific evidence and is not linked to any product of the supporting company. The scientific content of the article is the responsibility of the authors.
Please cite this article as: Mello CS, Barros KV, Morais MB. Brazilian infant and preschool children feeding: literature review. J Pediatr (Rio J). 2016;92:451–63.